I. INTRODUCTION
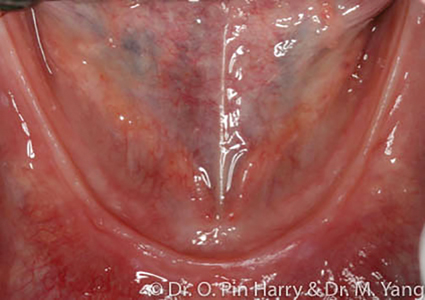
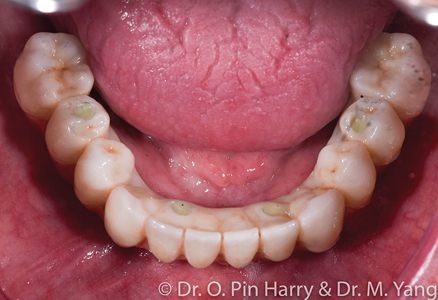
The prevalence of terminal dentitions and edentulism is undeniable. Predicted population studies and data have forecasted present findings.1 Edentulism (Fig. 1) is a recognized physical disability associated with multiple co-morbid health concerns including local, systemic, and psychological factors.2 The basic premise of prosthodontic rehabilitation of the edentulous patients has been and still is conventional complete denture therapy. Despite our best approach to care, a significant percentage of patients are unable to tolerate removable conventional prostheses.3 This is particularly prevalent for the mandibular arch (Fig. 2) where retention, stability and comfort constitute a triad of elusive quest for most. Data suggests that dental providers involved in full mouth implant supported reconstructions are seeing an increase in patient seeking this type of treatment. The desire and need for care are mainly motivated by the patients seeking to improve their oral health related quality of life. Rehabilitation of edentulous or soon to be edentulous patients (terminal dentitions) involve a prosthetically driven patient centered approach to diagnosis and treatment planning, from which an equally involved and necessary surgical phase is necessary to complete extractions of remaining natural teeth, site preparations and implant surgery.
Fig. 1
Fig. 2
II. PROSTHETIC SOLUTIONS FOR THE EDENTULOUS JAWS
Broadly and generally, edentulous prosthetic solutions include removable implant retained prostheses. These modalities of reconstructions include metal-acrylic overdentures retained by individual resilient attachments (Fig. 3) or bar-supported (Fig. 4), fixed full arch prostheses which can be metal-acrylic, porcelain fused to metal or zirconia. (Figs. 5,6 & 7) This article will discuss a general approach to care for the fixed rehabilitation of edentulous arches where some well-known prosthetic complications present challenges to clinicians and patients alike. The cases examples illustrate the reconstructions of patients who have been edentulous for several years or have significant dental and dento-alveolar bone loss – the type of prosthetic solutions, therefore are electively FP-2 or FP-34 including prosthetic gingival reconstruction as part of the definitive restoration. Implant numbers and surgical phases are beyond the scope of this article however if the treating clinician assumes and ensures adequate placement of an adequate number of implants per arch to provide acceptable angulation, spread and depth for restorative space, technical and prosthetic complications can most certainly be minimized.
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
III. COMPLICATIONS AND CHALLENGES
A systematic review5 on implant prosthetic complications has shown the most prevalent complication with fixed implant reconstructions is acrylic tooth fractures, acrylic debonding. This was further proven with clinical studies involving metal acrylic fixed prostheses.6 In this regard, there has been attempts to optimize metal framework designs and robustness, however the acrylic failures (Fig. 8) remain a real challenge, requiring spotted repairs in best case scenarios to full acrylic re-processing of teeth and acrylic base. Clinicians must be thorough in informing the patient pf these potential and expected complications, however the patient is ultimately surprised and somewhat disappointed when they occur. Technical complications, even when small and simple to rectify, can strain a good doctor/patient rapport. It has been shown that technical prosthetic complications can be a financial burden to both patients and clinicians.7 It is difficult to quantify such time-cost factor objectively in clinical practice. Patient loss in time-cost factor even for the best informed and prepared as well as opportunity cost can be a real problem over time. Other the past 20 years or more, solutions have been sought, often via trial and error starting with laboratory studies which often did not translate to expected clinical success. Porcelain fused to metal fixed prosthesis can bypass the acrylic problem. However, the laboratory time and cost factor can be a serious barrier. Precious alloy frames are onerous, casting technology has inherent challenges in achieving passive fitting frame-work and base metal milled frames have been alternatives that help resolve some issues. The prevalence of porcelain veneer fractures and debonding of metal frameworks is also prevalent8 although less frequent than acrylic. Porcelain complications are more common when opposing prostheses are all implant-borne due to the lack of resilience from the periodontal ligament in fixed reconstructions on natural teeth.
Fig. 8
IV. CONTEMPORARY ZIRCONIA PROSTHESES
More recently, zirconia frameworks purported the dual advantage of framework robustness and esthetic qualities of so-called YTZ. Such framework still requires a layering veneer porcelain to enhance the optical qualities of texture, translucency, chroma gradient and hue all combined. Generally, more robust/dense materials forgo desired optical properties such as translucency (3Y-TZP versus 5Y-TZP, just to cite an example).9 Monolithic prostheses virtually eliminate the risks of veneer porcelain failures (fractures and chips). The most sophisticated zirconia materials offer monolithic finishing capabilities with less esthetic compromises,10 added strength, reduced ceramic finishing laboratory bench times and very accurate shape replications derived from provisional prostheses that have been tested functionally and esthetically intraorally before confirmation for definitive porcelain fabrication. To that effect, the authors emphasized this aspect of predictability and consistency of monolithic materials over the layered veneer approaches – no matter how experienced and talented the ceramist, it is virtually impossible to replicate exactly the intricate shapes, dimensions, cusp angles, incisal guidance pathways that have been created, modified, and tested intra-orally. This superior technological feat of monolithic finishes provides seamless transition from a confirmed verified provisional to the final porcelain prosthesis. In addition, in the realm of superior posterior tooth anatomy, monolithic prostheses draw access to ultimate tooth-libraries from a broad spectrum of shapes and form. To be fair, the “monolithic digital technician” spends a significant amount of time in the virtual design of the case before pressing “Mill” to begin the CAM process of the green state zirconia blank. The traditional talented ceramist who stacks porcelain in powder liquid form and bakes the veneer on sintered frame works would spend less “virtual design” time and more bench time for the esthetic veneer portion.11 One major initial draw-back of monolithic materials is the lack of chroma gradient and the “life-like” glaze obtained with veneered prostheses. However, in the author’s more recent experiences with sophisticated monolithic zirconia and carefully executed stain, dye and glazing from pre-sintered to sintered phases, the esthetic results have become more and more promising. Although it is still possible for the “trained” eye to spot a monolithic finish versus a veneered finish, the esthetic gap has narrowed significantly compared to 5-7 years ago. Monolithic applications have increased for posterior restorations namely as the esthetic requirements are less demanding than anterior restorations. In the authors opinion, the profession will see a broader expansion of monolithic prostheses in time and by the same token less bench time to stack porcelain. Of course, talented esthetic ceramists will always have their place to veneer custom matched cases when required – these same ceramists will naturally develop the “feel” it takes to stain and glaze monolithic zirconia.12
PRESENT CLINICAL OUTLOOK
In the authors’ clinical experiences, several re-treatment cases can be attested whereby, the patients had undergone multiple surgical procedures over 6-12 months while wearing a removable temporary denture, involving extractions, delayed implant placement, delayed loading that fits a traditional implant-prosthetic protocol. Surely, not all cases can be non-grafted and one-surgical intervention with immediate fixed provisional loading, however the clinician who favors a multiple surgical/delayed implantation approach must be cognisant of the psychological and physical impact on the patient’s quality of life during active treatment. Rather than surgically over-treating the arch with multiple surgical interventions, involving delayed implants, current scientific evidence and clinical studies have clearly shown that immediate implantation can be predictable13 and equally successful for qualified cases. If a clinician’s therapeutic goals are to minimize the most frequent technical complications of fixed implant prostheses, foundational prosthodontic principles remain primordial: passive fitting frameworks, reduced componentry, strategically distributed implants across the edentulous arch for optimal A-P spread while avoiding anatomical structures, utilizing OEM implant components, and following a strict protocol from diagnosis to the final delivery and fitting of the prosthesis. Given this goal, the ultimate sophistication should be found in simplicity while respecting esthetics and function. This could include reduction of unnecessary implant components and elimination of hybrid materials within a singular prosthesis where possible. In simple lay terms, elimination of unnecessary junctions of dissimilar materials, screws, layering material, creating predictable sintering dimensional changes to optimize predictable framework fit.
CLINICAL CASES
The following clinical cases demonstrate two approaches to full arch All-on-X contemporary protocols:
A – Selectively layered prosthesis in non-functional areas (Figs. 9-11)
B – Monolithic non-layered prosthesis with only pink porcelain as layered (Figs. 12-14)
Fig. 9
Fig. 10
Fig. 11
Fig. 12
Fig. 13
Fig. 14
Both cases presented with terminal dentitions with high risk of recurrent caries. The patient desired a fixed implant supported prosthesis to rehabilitate function and esthetics. The diagnosis and treatment plan follows a facially generated approach whereby the teeth set up using esthetic and anthropomorphic averages.14 First the broad esthetic evaluation from a social distance and subsequently delving in a more detailed set up following anatomical references: facial midline, maxillary and mandibular incisal edge positions, the frontal and sagittal orientation of the occlusal plane, the adequate vertical dimension in centric relation where the maxilla-mandibular relationship is established and finally completed with adequate individual tooth shapes that define the occlusal relationships from cusps to fossa. The occlusal function is matched with esthetics from occlusal static points to dynamic eccentric pathways of the intricately designed inter-arch occlusal relationships. The initial digital design is rendered as an interim prosthesis that can be immediately loaded on the implants provided adequate initial implant stability is obtained. Following required time for osseo-integration, the final porcelain prosthesis is fabricated deriving accurate references from the interim fixed prosthesis. It is not uncommon, at this final stage, to provide some refinements as deemed necessary when designing the final prosthesis.
CONCLUSION
This article reviewed the traditional methods used to fabricate fixed implant-supported prostheses. The observed technical complications and challenges encountered with hybrid prostheses lead to a need for more durable and robust materials for these type of implant reconstructions. Contemporary fixed full arch zirconia restorations seem to show promising results in both in-vitro studies and clinical studies. A few case examples were presented to illustrate contemporary modes of treatment in a specialty prosthodontic practice. We are perhaps not that far away from an optimized material that offers function, perennity, esthetics and reduced technical complications.
Oral Health welcomes this original article.
References
- Douglass CW, Shih A, Ostry L. Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent. 2002 Jan;87(1):5-8. doi: 10.1067/mpr.2002.121203. PMID: 11807476.
- Felton DA. Edentulism and comorbid factors. J Prosthodont. 2009 Feb;18(2):88-96. doi: 10.1111/j.1532-849X.2009.00437.x. PMID: 19254297.
- Celebic´ A, Knezovic´ -Zlataric´ D, Papic´ M, Carek V, Baucic´ I, Stipetic´ J. Factors related to patient satisfaction with complete denture therapy. J Gerontol A Biol Sci Med Sci. 2003 Oct;58(10):M948-53. doi: 10.1093/gerona/58.10.m948. PMID: 14570864.
- Misch’s Contemporary Implant Dentistry 4th Edition
- Goodacre BJ, Goodacre SE, Goodacre CJ. Prosthetic complications with implant prostheses (2001-2017). Eur J Oral Implantol. 2018;11 Suppl 1:S27-S36. PMID: 30109297.
- Purcell BA, McGlumphy EA, Holloway JA, Beck FM. Prosthetic complications in mandibular metal-resin implant-fixed complete dental prostheses: a 5- to 9-year analysis. Int J Oral Maxillofac Implants. 2008 Sep-Oct;23(5):847-57. PMID: 19014154.
- Ravidà A, Tattan M, Askar H, Barootchi S, Tavelli L, Wang HL. Comparison of three different types of implant-supported fixed dental prostheses: A long-term retrospective study of clinical outcomes and cost-effectiveness. Clin Oral Implants Res. 2019 Apr;30(4):295-305. doi: 10.1111/clr.13415. Epub 2019 Mar 29. PMID: 30758878.
- Heitz-Mayfield LJ, Needleman I, Salvi GE, Pjetursson BE. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int J Oral Maxillofac Implants. 2014;29 Suppl:346-50. doi: 10.11607/jomi.2013.g5. PMID: 24660208.
- Passos SP, Nychka JA, Major P, Linke B, Flores-Mir C. In vitro fracture toughness of commercial Y-TZP ceramics: a systematic review. J Prosthodont. 2015 Jan;24(1):1-11. doi: 10.1111/jopr.12179. Epub 2014 Jun 27. PMID: 24975460.
- Shahmiri R, Standard OC, Hart JN, Sorrell CC. Optical properties of zirconia ceramics for esthetic dental restorations: A systematic review. J Prosthet Dent. 2018 Jan;119(1):36-46. doi: 10.1016/j.prosdent.2017.07.009. Epub 2017 Sep 18. PMID: 28927925.
- Papaspyridakos P, Chochlidakis K, Kang K, Chen YW, Alghfeli A, Kudara Y, Weber HP. Digital Workflow for Implant Rehabilitation with Double Full-Arch Monolithic Zirconia Prostheses. J Prosthodont. 2020 Jul;29(6):460-465. doi: 10.1111/jopr.13166. Epub 2020 Apr 9. PMID: 32185825.
- Papageorgiou-Kyrana K, Fasoula M, Kontonasaki E. Translucency of Monolithic Zirconia after Hydrothermal Aging: A Review of In Vitro Studies. J Prosthodont. 2020 Jul;29(6):489-500. doi: 10.1111/jopr.13174. Epub 2020 May 28. PMID: 32275345.
- Gallardo YNR, da Silva-Olivio IR, Gonzaga L, Sesma N, Martin W. A Systematic Review of Clinical Outcomes on Patients Rehabilitated with Complete-Arch Fixed Implant-Supported Prostheses According to the Time of Loading. J Prosthodont. 2019 Dec;28(9):958-968. doi: 10.1111/jopr.13104. Epub 2019 Oct 18. PMID: 31433096.
- Martone AL. Complete denture esthetics and its relation to facial esthetics. Dent Clin North Am. 1967 Mar:89-100. PMID: 5225609.
- Murrell GA. Complete denture esthetics. Dent Clin North Am. 1989 Apr;33(2):145-55. PMID: 2656314.
About the Author
 Dr. Oliver Pin-Harry earned his DDS from L’Université de Montpellier, France and his MS and Certificate in Prosthodontics from the University of North Carolina at Chapel Hill, where he serves as Adjunct Assistant Professor. He serves as a Clinical Instructor in Graduate Prosthodontics at U of T and maintains full-time specialty clinics at Burlington Prosthodontics and M Prosthodontics in Toronto.
Dr. Oliver Pin-Harry earned his DDS from L’Université de Montpellier, France and his MS and Certificate in Prosthodontics from the University of North Carolina at Chapel Hill, where he serves as Adjunct Assistant Professor. He serves as a Clinical Instructor in Graduate Prosthodontics at U of T and maintains full-time specialty clinics at Burlington Prosthodontics and M Prosthodontics in Toronto.
 Dr. Michael Yang completed his DDS from the New York University, College of Dentistry and his Certificate in Prosthodontics and MS degree at the University of Illinois at Chicago. He holds the position of Staff Prosthodontist at SickKids Hospital and is an Instructor at the University of Toronto. Dr. Yang maintains private practice at M Prosthodontics and Burlington Prosthodontics.
Dr. Michael Yang completed his DDS from the New York University, College of Dentistry and his Certificate in Prosthodontics and MS degree at the University of Illinois at Chicago. He holds the position of Staff Prosthodontist at SickKids Hospital and is an Instructor at the University of Toronto. Dr. Yang maintains private practice at M Prosthodontics and Burlington Prosthodontics.