Extract
Preservation of natural tooth structure during an endodontic procedure is paramount in order to ensure predictable clinical success. In the past, access cavity preparation, instrument design and taper as well as spatial accommodation for obturation techniques has inadvertently induced iatrogenic potential to the results achieved and over time, functional stresses have caused the tooth to fail both biologically and structurally. The winds of change in endodontics are negating these unfortunately sequelae as a result of bio-minimalistic considerations in access, metallurgical and engineering redesign of files systems and the introduction of new obturation materials.
Introduction
This is the first in a series of articles to be written by Drs. Trope and Serota in regard to the evolutionary changes in the endodontic armamentarium that are redressing past misconceptions and enacting new technologies to both preserve tooth structure and eradicate existing and recrudescent apical periodontitis.
The recent history of endodontics has been an evolution through several transitional stages; nickel-titanium (NiTi) instruments for sculpting and debridement, microscopes for illumination and magnification, indispensable for detection and exploration of the inner space of teeth (Figs. 1a-d) and of late, the inclusion of cone beam computed tomography for diagnosis and treatment planning.
Fig. 1a
4 rooted maxillary molar.

Fig. 1b
Maxillary molar fused roots.

Fig. 1c
Mandibular molar A.

Fig. 1d
Mandibular molar B.

The root canal system is an arborizational, an astomotic, byzantine, labyrinthine complexity, morphologically comparable to the passages of a maze. While primary canals exist, the tributaries, accessory branches and luminae of the dentinal tubuli harbor extensive tissue and microflora, which if left untreated remain vectors for persistent and refractory pathology. Carabelli documented the first description of these vast and capacious pathways in 1842. Since then, Muhlreiter (1870), G. V. Black (1890), Preiswerck (1901), Fischer (1907), Dewey (1916), Hess (1917), Okumura (1918-1926), Davis (1923), Barret (1925), De Deus (1960) among others studied the magical mystery tour of root canal anatomy. The quest continues to this day with the use of micro-computed tomography. (Appreciation to Marco Versiani, Jesus D. Pécora and Manoel D. Sousa Neto – http://rootcanalanatomy.blogspot.com)
The clinician can thus anticipate, visualize and treat with unprecedented levels of accuracy and safety. However; the failure to overcome all potential mechanical and pathologic vectors that negate treatment success continues in spite of these technologic advances. The most current evolution is a minimalistic approach to access design by shifting the outline configuration towards greater dentin preservation and idealizing the endodontic-restorative interface (Figs. 2a-d). This article will address aspects of the access, treatment and restorative paradigm shifts in development.
Minimally invasive dentistry (MID) is the application of “a systematic respect for the original tissue”. This implies that the profession as a whole recognize that artifice has a lesser biologic value than the original healthy tissue. MID or bio-minimalism proposes that the common denominator is tissue preservation, preferably by preventing disease from occurring and intercepting its progress, but also by removing and replacing pathology with as little tissue loss as possible. 1,2 These aims are logical if taken in the appropriate context. They do not suggest that that respect for original tissue is more important than preventing or treating disease, only that the disease prevention and/or elimination should be performed without unnecessarily sacrificing native tissue.
The aspects in clinical endodontics that are essential for biological success in the absence of peri-radicular disease and paramount for the survivability of the tooth are; the eradication of microbial presence, particularly in the apical 3 to 4 mm of the root canal space, minimal removal of native tissue in the coronal two thirds of the root to enhance long term success and optimal access to the root canal space both in the coronal two-thirds and apical 3 to 4 mm segment. Prior to addressing the question, “how are we doing at the moment”, it is wise to reflect upon the value derivative from “clinical impact factors” and “scientific impact factors”. 3 The many variables in clinical dental research make it unlikely that they will have the same scientific potentials as, for example, a laboratory study. In this aspect, we are at an impasse as traditional in vitro studies, from a clinical practice point of view, are essentially of little or no value and anecdotal empirical protocol change based on extrapolation may seem valid, but lack the substantiation of a controlled study.
Fig. 2a, Fig. 2b
Traditional access preparations were slightly divergent to enable convenience form in the era prior to the introduction of super-elastic metallurgy into the instrumentation armamentarium. The more constrained, constricted or preferably conservative access cavity encourages the retention of soffits ostensibly to minimize cuspal flexure during mastication. Modification of the access design is predicated on planar geometry of the roots and factors such as limitation of inter-occlusal distance.

Fig. 2c, Fig. 2d
Clark and Khademi 1 have described a revisionist concept of conservative endodontic access that prioritizes the removal of restorative materials before tooth structure, of enamel before dentin and of occlusal tooth structure before cervical dentin. It negates the traditionalist straight line access protocol and the totality of de-roofing the pulp chamber. The biologic mandate of greatest imperative is the preservation of the critical region of peri-cervical dentin (PCD–4mm above and below the crestal bone) to the paramount achievable degree without compromising debridement or inducing iatrogenic misadventure. [Appreciation to Hany Mohamed Aly Ahmed, BSc, HDD (Endo), PhD – Universiti Sains Malaysia].
![Clark and Khademi 1 have described a revisionist concept of conservative endodontic access that prioritizes the removal of restorative materials before tooth structure, of enamel before dentin and of occlusal tooth structure before cervical dentin. It negates the traditionalist straight line access protocol and the totality of de-roofing the pulp chamber. The biologic mandate of greatest imperative is the preservation of the critical region of peri-cervical dentin (PCD–4mm above and below the crestal bone) to the paramount achievable degree without compromising debridement or inducing iatrogenic misadventure. [Appreciation to Hany Mohamed Aly Ahmed, BSc, HDD (Endo), PhD – Universiti Sains Malaysia].](https://media.oralhealthgroup.com/uploads/2017/05/Serota-Fig-2c-d-300x206.jpg)
Biological Success
Assessment of university based studies shows that endodontic treatment outcome success ranges from 80% for infected teeth to 96% for non-infected teeth. This suggests that even when the clinician has limited experience (dental students) the (biological) success rate for root canal treatment can be extremely high. Unfortunately, cross-sectional cohort studies in general dentistry practices in a practice based research network (PBRN) show that the success rate ranges from 40 to 73% for a myriad of reasons. 4,5 Of all those reasons, caries, periodontal disease and fracture are most prominent. The perception that the incidence of fracture in endodontically treated teeth is intrinsically related to the amount and quality of remaining dentin is valid in a generic sense; 6,7 however, it discounts the myriad of restorative factors and design scenarios causing unfavorable biomechanical shear stresses that must be held to account. 8-10
Functional Success
The majority of studies on functional success have been performed to justify root canal versus implant (partial edentulism) survival rates. The functional success of root treated teeth ranges as high as 97% 11 and is actually more favorable than implants de facto if length of time and post treatment complications are taken into account. It must be acknowledged however, that many of these studies on functional success were performed on teeth treated with stainless steel files with 0.02 tapers. In vitro studies using NiTi files with larger tapers have shown micro-cracks develop in the tooth structure as the taper increases leading to possible fractures and thus a decrease in the reported functional success rates. 12
Cone Beam Computed Tomography
The scope of this article prevents an elaborate discussion of cbCT; however, in the context of an image speaks a thousand words, the value of the sagittal, coronal and axial images obtained from small field of view (FOV) scans is a quantum leap forward in diagnosis and treatment planning. As demonstrated in Figure 1, for decades we have been treating three-dimensional teeth with two-dimensional images. Axial slices assist in the identification of the number of canals (Figs. 3a-c), they are an aid in determining the location of external root resorptions, bifidities, diametral width and curvature at various levels along the length of the root. Coronal slices offer an evaluation of the myriad of configurations characteristic of premolars and molars, predominantly in the mandible. They assist in guiding the clinician to avoid hard tissue removal in exploring for canal angulation and orientation (Fig. 4). Sagittal slices assist in eliminating the anatomic noise of overlapping structures, particularly in the maxilla and enables a clarity of “z” axis perspective in both orthograde and retrograde treatment previously unobtainable (Fig. 5).
Fig. 3a
The traditional flat film used to pre-operatively asses number of roots, the degree of calcification and the planar geometries of the roots along their length has now been augmented by axial slices which assist in identification of the number of canals and various anatomical configurations and aberrations.

Fig. 3b
The 3 canals untreated in MB root of tooth #2 (1.7).

Fig. 3c
Canals obturated – [Appreciation to Wild Bill Nudera and his daughter Farrah].
![Canals obturated – [Appreciation to Wild Bill Nudera and his daughter Farrah].](https://media.oralhealthgroup.com/uploads/2017/05/Serota-Fig-3c-300x189.jpg)
Fig. 4
The coronal view can assist in determining branching otherwise undetectable and assist in access orientation to ensure optimal preservation of peri-cervical dentin. [Appreciation for the contribution of Dr. Charlie Boveda].
![The coronal view can assist in determining branching otherwise undetectable and assist in access orientation to ensure optimal preservation of peri-cervical dentin. [Appreciation for the contribution of Dr. Charlie Boveda].](https://media.oralhealthgroup.com/uploads/2017/05/Serota-Fig-4-140x140.jpg)
Fig. 5
Sagittal views provide the clinician with the z axis perspective to identify the distance between splits in roots and the orientation of the roots about themselves. This is of paramount importance particularly in micro-surgical treatment. [Appreciation to Wild Bill].
![Sagittal views provide the clinician with the z axis perspective to identify the distance between splits in roots and the orientation of the roots about themselves. This is of paramount importance particularly in micro-surgical treatment. [Appreciation to Wild Bill].](https://media.oralhealthgroup.com/uploads/2017/05/Serota-Fig-5-300x239.jpg)
Bio-minimalism recognizes that the peri-cervical dentinal (PCD) zone is crucial for buttressing the residual coronal tooth structure during functional loading stress and ostensibly acts to minimize cuspal flexure during mastication. The challenge to the clinician is to negotiate all canals, debride residual pulp tissue from all loci and avoid iatrogenic complications while working through a restricted access without “convenience form”. 13 This begs the question, “how can we remove as many microbes as possible while still maintaining the strength of the tooth?”.
Fortunately, there are technological advances in the instrumentation armamentarium that bring us closer to the aims of minimally invasive endodontics. We are in an era in endodontics with the introduction of disinfection systems that do not require changing the non-round canal to a round shape. This previous formulistic alteration meant that sculpting of the inner space was overly minimized or too much native tissue was removed. We now have files and finishers that are able to adjust to the original shape of the canal, scrape biofilm in a manner similar to periodontal scalers and facilitate irrigants to act upon exposed microbes. These systems will continue to iterate enabling the clinician to retain more native root structure while more effectively removing inflammatory vectors (Figs. 6a-e).
Fig. 6a
The XP -endo Finisher [FKG Dentaire SA, La Chaux-de-Fonds, CH] is used after preparation of the canal to the size of at least a #25 file. The Finisher file is produced using an exclusive alloy, NiTi MaxWire which enables it to react at different temperature levels. It’s small core size, ISO 25 in diameter and its zero taper allows it to contact the walls of the canal and clean them without changing the original shape of the canal.
![The XP -endo Finisher [FKG Dentaire SA, La Chaux-de-Fonds, CH] is used after preparation of the canal to the size of at least a #25 file. The Finisher file is produced using an exclusive alloy, NiTi MaxWire which enables it to react at different temperature levels. It’s small core size, ISO 25 in diameter and its zero taper allows it to contact the walls of the canal and clean them without changing the original shape of the canal.](https://media.oralhealthgroup.com/uploads/2017/05/Serota-Fig-6a-113x300.jpg)
Fig. 6b
The canal working length is fixed by using a plastic tooth to adjust the rubber stopper and cooled down inside the tube using a cold spray.
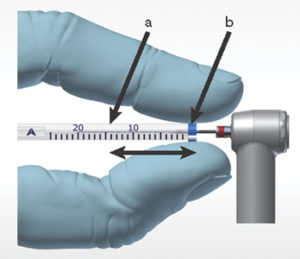
Fig. 6c
The Finisher is placed in rotation mode and removed from the tube by applying lateral motion to ensure it remains straight. Once the straight file is inside the canal, the rotation is turned on and the file inserted incrementally into the canal the irrigant in the chamber is constantly replenished.

Fig. 6d
The Finisher is used for 1 minute using slow and gentle 7 to 8 mm lengthwise movements to the contact the full length of the canal and after that period removed from the canal while rotating.
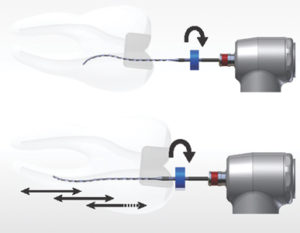
Fig. 6e
The concept of a continuously tapering funnel relates to a technical need for a shape that will accommodate condensers for vertical compaction of thermo-labile gutta-percha. The logical shape to preserve integral tooth structure is for a taper in the apical region alone, with a minimal or no taper in the coronal two-thirds of the canal system. With the advent of bioceramics as an optimal sealing modality, the endodontic-restorative interface is never compromised to facilitate the Obturation phase–(Appreciation to Dr. Gilberto Debelian for sharing this case).

From the standpoint of survivability, the future looks increasingly bright, not only due to bio-minimalistic technical changes but also due to the introduction of new obturation materials. Until recently, the preparation of the coronal two thirds of the canal was designed to facilitate plugger placement to within 4mm of the apical terminus in order to generate the hydraulic forces necessary to deform thermo-labile gutta-percha in the apical capture zone with optimal gravitometric density. This necessitated large tapers destructive to the native root structure with minimal benefit to microbial removal. The introduction of bioceramics brings a material with antimicrobial potential (high alkaline pH), biocompatibility, bioactivity, and no evidence of shrinkage upon setting (EndoSequence[S®l] BC Sealer™ and BC RRM-Fast Set Putty, Brasseler USA Savannah, GA). The myriad of applications from orthograde to retrograde to resorptive treatment facilitates enhanced sealing without the need for removal of excess inner or outer root structure. 14
Unfortunately, minimally invasive access design has dominated the discussion of bio-minimalism in endodontics. Traditional endodontic access design adhered to the restorative axiom extension for prevention which manifested as straight line access; de-roofing the pulp chamber and pre-flaring the canal orifice to facilitate the subsequent shaping of the entire root-canal system in order to negotiate the apical terminus. However; optimal diametral retention of coronal/radicular dentin and maintenance of the planar geometry of the root canal anatomy essential for the structural integrity of endodontically restored teeth was unduly compromised. 15
There are many limitations to what is preached as the perfect minimally invasive cavity design (conservative access preparation). In teeth requiring root canal treatment, the shape and size of the access opening is invariably dictated by caries, failing or lost restorations. It is imprudent and unlikely that a clinician would leave diseased tooth structure in order to configure a textbook access cavity. Removal of unnecessary dentin during access preparation was never the biologic mandate of access design. Even in the Schilderian era, the goal was to retain as much of the cervical dentin as possible while still achieving straight-line access to the apical termini (the greater the curvature in the canal the greater the relevance for a glide path to achieve a “straighter line access”).
Perhaps the aim of conservative cavity preparation should be reframed from “removal of as little tooth structure as possible” to “removal of as little as necessary”. As discussed previously, clinicians now have a myriad of technologies at their disposal to assist in the execution of this redefined objective. Restoratively in the adhesion era, we are now blessed with an abundance of riches to move away from the post/core and full coverage paradigm of the past, which only further compromised the retention of foundational tooth structure to a truly bio-minimalistic restorative template.
One can barely skim the surface in a publication of this brevity, however, the purpose is to create an energy dynamic analogous to the ripples produced by dropping a stone in a pool of water. With minimal resistance they can expand concentrically in greater and greater diameters. Or one could be a curious octopus and go off in all directions; that will be forthcoming in the online curriculum under development for Dentaltown.com. Perhaps the answer to all the issues that remain to be corrected in endodontics was articulated eloquently over a hundred years ago by the man who predicted waves in the gravitation fields of the universe. “We cannot solve our problems with the same thinking we used when we created them” – Albert Einstein OH
Oral Health welcomes this original article.
References
1. Clark D, Khademi J. Modern Molar Endodontic Access and Directed Dentin Conservation. DCNA. 2010;54(2):249-73.
2. Ericson D. What is minimally invasive dentistry? Oral Health Prev Dent. 2004;2(sup1):287-92.
3. Mjor IA. Scientific Impact and Clinical Impact. J Adhesion Dent. 2009;11(3): 171-2.
4. Gilbert GH et al. Outcomes of root canal treatment in Dental Practice-Based Research Network practices. Gen Dent. 2010; 58(1):28.
5. Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endodontic Topics. 2006;13:57-83.
6. Trope M, Maltz DO, Tronstad L. Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol. 1985;1(3):108-11.
7. Schmitter M, Sterzenbach et al. A flood tide of systematic reviews on endodontic posts: methodological assessment using of R-AMSTAR. Clin Oral Investig. 2013;17:1287-94.
8. Naumann M, Blankenstein et al. Risk factors for failure of glass fiber-reinforced composite post restorations: a prospective observational clinical study. Eur J Oral Sci. 2005;113:519-24.
9. Torbjorner A. Fransson B. Biomechanical aspects of prosthetic treatment of structurally compromised teeth. Int J Prosthodont. 2004;17:135-41.
10. Salehrabi R, Rotstein I. Endodontic Treatment Outcomes in a Large Patient Population in the USA: An Epidemiological Study. J Endo. 2004;30(12): 846-50.
11. Pop I et al. Synchroton light-based microCT to analyse the presence of dentinal microcracks post-rotary and reciprocating instrumentation. Clin Oral Invest. 2014 Feb (published online) Christie WH, Thompson GK. The importance of endodontic access in locating maxillary and mandibular molar canals. JCDA. 1994;60(6):527-36.
12. Haapasalo M. Clinical use of bioceramic materials. Endo Topics. 2015;32:97-117.
13. Castellucci A. Endodontics; Access Cavity and Endodontic Anatomy. Editions Martina, Bologna IT;244-329.
About the Author
 Dr. Martin Trope was born in Johannesburg, South Africa where he earned his BDS degree in dentistry in 1976. From 1976 to 1980, he practiced general dentistry and endodontics. In 1980, he moved to Philadelphia to specialize in Endodontics at the University of Pennsylvania. After graduating as an endodontist, he continued at the University of Pennsylvania as a faculty member until 1989 when he became Chair of Endodontology at Temple University, School of Dentistry. In 1993, he accepted the JB Freedland Professorship in the Department of Endodontics at the University of North Carolina at Chapel Hill, School of Dentistry. Named in honor of one of the founding fathers of Endodontics, the Freedland Professorship recognizes significant contributions to the specialty. Dr. Trope is currently clinical professor, Department of Endodontics, School of Dental Medicine at the University of Pennsylvania. Some of Dr. Trope’s past achievements include: Director of the American Board of Endodontics, Editor-in-chief of both journals, Dental Traumatology and Endodontic Topics, Member of the Editorial Board of Oral Surgery, Oral Medicine, Oral Pathology, Member of the Advisory Board of Esthetic Dentistry, The Louis I. Grossman Award for publication of significant research (April 2002). As well, Dr. Trope frequently does research in the following subjects: dental trauma, clinical treatment outcomes, new diagnostic tests for pulpal and periapical disease and material development for root canal filling.
Dr. Martin Trope was born in Johannesburg, South Africa where he earned his BDS degree in dentistry in 1976. From 1976 to 1980, he practiced general dentistry and endodontics. In 1980, he moved to Philadelphia to specialize in Endodontics at the University of Pennsylvania. After graduating as an endodontist, he continued at the University of Pennsylvania as a faculty member until 1989 when he became Chair of Endodontology at Temple University, School of Dentistry. In 1993, he accepted the JB Freedland Professorship in the Department of Endodontics at the University of North Carolina at Chapel Hill, School of Dentistry. Named in honor of one of the founding fathers of Endodontics, the Freedland Professorship recognizes significant contributions to the specialty. Dr. Trope is currently clinical professor, Department of Endodontics, School of Dental Medicine at the University of Pennsylvania. Some of Dr. Trope’s past achievements include: Director of the American Board of Endodontics, Editor-in-chief of both journals, Dental Traumatology and Endodontic Topics, Member of the Editorial Board of Oral Surgery, Oral Medicine, Oral Pathology, Member of the Advisory Board of Esthetic Dentistry, The Louis I. Grossman Award for publication of significant research (April 2002). As well, Dr. Trope frequently does research in the following subjects: dental trauma, clinical treatment outcomes, new diagnostic tests for pulpal and periapical disease and material development for root canal filling.
 Dr. Ken Serota graduated from the University of Toronto Faculty of Dentistry in 1973 and was awarded the George W. Switzer Memorial Key for excellence in Prosthodontics. He received his Certificate in Endodontics and Master of Medical Sciences Degree in nuclear medicine from the Harvard-Forsyth Dental Center in Boston, Massachusetts. In 1981 he was the recipient of the American Association of Endodontics Memorial Research Award for his work in nuclear medicine screening procedures related to dental pathology. He provided an interactive endodontic program for the Ontario Dental Association from 1983 to 1997 and was awarded the O.D.A. Award of Merit in 1987 for his efforts in the provision of continuing education. Active in online education since 1998, he is the founder of the online endo forum ROOTS, the Facebook forums NEXUS and Dental Divas Global and he is currently Global Clinical Director for Dentaltown.
Dr. Ken Serota graduated from the University of Toronto Faculty of Dentistry in 1973 and was awarded the George W. Switzer Memorial Key for excellence in Prosthodontics. He received his Certificate in Endodontics and Master of Medical Sciences Degree in nuclear medicine from the Harvard-Forsyth Dental Center in Boston, Massachusetts. In 1981 he was the recipient of the American Association of Endodontics Memorial Research Award for his work in nuclear medicine screening procedures related to dental pathology. He provided an interactive endodontic program for the Ontario Dental Association from 1983 to 1997 and was awarded the O.D.A. Award of Merit in 1987 for his efforts in the provision of continuing education. Active in online education since 1998, he is the founder of the online endo forum ROOTS, the Facebook forums NEXUS and Dental Divas Global and he is currently Global Clinical Director for Dentaltown.
RELATED ARTICLE: Dynamic Navigation For Orthograde And Retrograde Endodontics












