Mention “Botox” (the neuromodulator Botulinum Neurotoxin Type A or “BoNt-A”) sold in North America as Botox, Dysport, and Xeomin (Fig. 1), and the average person thinks immediately of wrinkles. However, the January 16, 2017 issue of Time Magazine’s cover page article (Fig. 2) identified 800 medical uses of BoNt-A including depression, heart trouble, migraines, erectile dysfunction, back pain, sweaty palms, drooling and 793 other problems. As dental health practitioners, it is important for us to open our minds and begin to understand how BoNt-A fits into our diagnostic and treatment armamentarium, thereby improving the well-being of our patients.
Fig. 1
The three most common neuromodulators are Botox Cosmetic by Allergan, Dysport by Galderma, Xeomin by Merz.

Fig. 2
Time Magazine issue January 16, 2017

As Canadians, we should feel proud that in the 1990’s, Drs. Jean and Alastair Curruthers put Vancouver, B.C., on the map medically speaking, discovering how BoNt-A can be used to improve facial aesthetics. Huge strides have occurred since they first pioneered its use for reducing crow’s feet around the eyes (Fig. 3) (peri-orbital rhytids). Few then would have thought that BoNt-A would be used today for treating the muscles of mastication and other muscles of the face and neck (Fig. 4).
Fig. 3
Relaxed Close up 45 degree right Orbicularis Oculi (Crow’s feet) before (left) neuromodulator injection and after (right) neuromodulator treatment using Facetec software.

Dynamic Close up 45 degree right Obicularis Oculi (Crow’s feet) before (left) neuromodulator injection and after (right) neuromodulator treatment using Facetec software.

Relaxed Full Face 45 degree right Obicularis Oculi (Crow’s feet) before (left) neuromodulator injection and after (right) neuromodulator treatment using Facetec software

Fig. 4
The muscles of facial expression and mastication of the head and neck.

A few years later in Toronto, two other Canadians, Drs. Marvin Schwartz and Brian Freund, pioneered the therapeutic use of BoNt-A for relieving chronic pain and dysfunction. Their research led to the understanding of the multiple mechanisms of action of BoNt-A. Again, few would have thought that today BoNt-A would be used to treat clenching, bruxism, TMD, myofascial pain, trigeminal neuralgia, headache, migraine, etc.
As with any treatment modality, proper training is essential. Some practitioners have felt that BoNt-A is useful only for treating frivolous aesthetic concerns and have proceeded to administer it as such; hence the popularity of the ‘Botox Party’. With such haphazard administration, numerous (two to nine percent) negative side effects became common.
To achieve predictable results and avoid negative side effects, in-depth knowledge of the relevant anatomy is essential (Fig. 5). Reviewing facial anatomy in the lab, learning how to locate bony landmarks (Fig. 6) and facial muscle origins and insertions, permits accurate placement of the drug with no negative side effects. Simply taking a syringe of BoNt-A and “injecting into wrinkles” without a clear understanding of the bony landmarks, origin, and insertion of relevant muscles, is a recipe for disaster.
Fig. 5
Cadaver section PTIFA Level 1 anatomy of the head and neck.

Fig. 6
Skull section PTIFA Level 1 bone, muscle origin and innervation of the head and neck.

Additionally, to drastically improve treatment results, one needs a way to accurately assess results by comparing before and after images. The Roberts Facial Rejuvenation Photography (RFRP) series (Fig. 7A-D) provides such a means. The photography series comprises a set of 29 photographs taken from a variety of angles before treatment and again two weeks later.
Fig. 7A
RFRP series Full Face relaxed and dynamic.

Fig. 7B
RFRP series Close Up Face relaxed and dynamic.

Fig. 7C
RFRP series Upper Face Close up relaxed & dynamic.
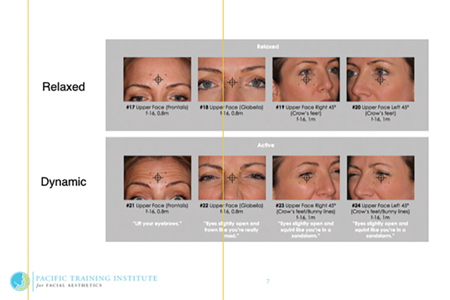
Fig. 7D
RFRP series Mid Face, Lower Face relaxed and dynamic plus intra-oral.

Fig. 7E
RFRP series American Academy of Cosmetic Dentistry Intra-oral series.

Using comparative “Facetec” software both patient and practitioner can view the changes and assess the results (Fig. 8). By marking and photographically recording the landmarks (Fig. 9), plus the actual injection sites (Fig. 10), it is possible to ascertain if any adjustments are required in the anatomical placement of the medication to obtain optimal results. Precise photography is required to ensure before and after photographs are comparing “apples with apples” and not “apple with oranges” (Fig. 11).
Fig. 8
The patient and practitioner review the photos.

Using Facetec software technology to review, compare and to access the results.

Fig. 9
Marking the Glabellar bony landmarks, muscle and injection sites.

Marking the Temporal bony landmarks, muscle and injection sites.

Fig. 10
The PTIFA weal Injection technique using the Glabellar bony landmarks for precise neuromodulator placement.

The PTIFA weal Injection technique using the Frontal bony landmarks for precise neuromodulator placement.

The PTIFA weal Injection technique using the Temporal bony landmarks for precise neuromodulator placement.

Fig. 11
Relaxed Full Face Frontal before (left) neuromodulator injection and after (right) neuromodulator treatment review on Facetec software.

Dynamic Full Face Frontal before (left) neuromodulator injection and after (right) neuromodulator treatment review on Facetec software.

Precise anatomical placement also allows assessment of proper dosage. Somewhat higher dosages than those used for aesthetic treatment alone results in reduction of headaches and migraines (Allergan PREEMPT study) (Fig. 12). A threshold dosage, carefully placed, must be reached in order to obtain therapeutic relief. At this juncture, the secondary and tertiary mechanisms of action of BoNt-A come into play and there is a synergy between aesthetic and therapeutic outcomes. Additionally, and not inconsequentially, there is a relationship between “looking good” and “feeling good” (Fig. 13). In 2018, the US FDA is expected to approve the use of BoNt-A for treatment of anxiety and depression.
Fig. 12
Proper diagnosis, precise neuromodultor placement and higher dosage achieves headache & migraine rduction.

Fig. 13
Relaxed Close up Face before neuromodulator -first appointment.

Relaxed Close up Face 2 weeks post neuromodulator (upper face) treatment with increased smile at rest.

This synergistic relationship between aesthetic and therapeutic injections is frequently accomplished with lower dosages than those recommended in studies such as Allergan’s “PREEMPT” migraine study. The lower dosages can be attributed to an understanding of the three distinct mechanisms of action of BoNt-A.
The primary mechanism of action works on muscle (Fig. 14) (initially applied to the muscles of facial expression and since expanded to many muscles of the human body). The secondary mechanism of action works on afferent pain pathways. An understanding of these pathways allows anatomical placement of BoNt-A to diminish painful input. The tertiary mechanism of action acts directly and indirectly on the Central Nervous System. The dental profession would be well served by understanding the relationship amongst these three mechanisms of action and their impact on our dental diagnosis and treatment.
Many aspects of dental treatment should include an understanding of how BoNt-A works. Hyperactive muscles can be detrimental to periodontal (Fig. 15), surgical and implant procedures (Fig. 16). Angiogenesis is greatly affected by muscle pull. Gingival recession can also be exacerbated by muscle pull. Differential diagnosis of endodontic pain (Fig. 17) can be aided with the use of BoNt-A. Bruxism and myogenic TMD often involve hypertrophic muscles (Fig. 18). Chronic grinding can be revealed in the RFRP photography series by identification of the “PTIFA Platysma band” (Fig. 19), providing a clue to the source of discomfort and pain. Hypertrophic muscles are readily observed thru the RFRP photography series (Fig. 20), often thru the size and shape of the face.
Fig. 14
Summary of the primary mechanism of action of neuromodulators.

Fig. 15
Insertion of Platysma into the Modiolus, frenums and soft tissue.

The dynamic forces of Platysma on the intra-oral tissue.

Fig. 16
The dynamic forces of the Maxillary levators on the extra-oral soft tissue producing a gummy smile.

The dynamic forces of the Maxillary levator muscles on the intra-oral tissue.

The dynamic muscle forces can effect the angiogenesis and success of the implants.


Fig. 17
Referred pain from the middle section of Temporalis to the Maxillary bicuspids.

Referred pain from the lower Masseter to the Mandibular molars.

Fig. 18
Relaxed Full Face Frontal (left) demonstrating chronic hypertrophic muscle in bruxism and myogenic TMD prior to neuromodulators and Relaxed Full Face Frontal (right) musculature 3 months post neuromodulator treatment copy.
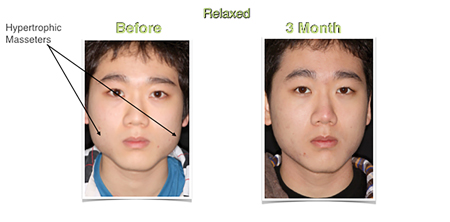
Fig. 19
The PTIFA Platysma band running superior onto Masseter is a diagnostic aid to bruxing, TMD and Myofascial pain diagnosis.

Fig. 20
Relaxed Full Face hypertrophic Masseter (left) and 6 week post neuromodulator treatment (right) on Facetec software.

There is significant overlap between aesthetic and therapeutic treatment. Many practitioners only perform “aesthetic” BoNt-A injections while others only “therapeutic”. A deeper understanding of how the two are related is required in order for the profession to serve our patients most effectively. As the medical profession has discovered over 800 uses for BoNt-A, the dental profession needs to expand its knowledge to the benefits this medication can provide and not dismiss it as a frivolous drug.
Deeper understanding of the anatomy involved and thorough recording of the pre-treatment and post-treatment results along with the injection sites will provide our patients with a higher level of care.
We must open our minds to the benefits that BoNt-A can provide our patients and erase the concept that its use is only for “frivolous aesthetic concerns”. Incorporating this treatment modality into our practices can significantly benefit our patients. OH
Oral Health welcomes this original article.
About the Authors
 Dr. Roberts is the Co-Founder and Clinical Director for the Pacific Training Institute for Facial Aesthetics (PTIFA)–an international educational organization that teaches physicians, dentists and nurses in the field of botulinum toxin, dermal fillers and facial aesthetics. Over the last 10+ years, Dr. Roberts has been a leading voice for raising the standard of patient care using botulinum toxin–both therapeutically and cosmetically. His educational model has been used by colleges to develop the “Standard of Practice” for facial aesthetic procedures. Dr. Roberts has developed a number of injection techniques and templates that make the patient experience remarkable. He is continuously recognized by Dentistry Today as one of the top 100 CE speakers. For more information, visit PTIFA.com.
Dr. Roberts is the Co-Founder and Clinical Director for the Pacific Training Institute for Facial Aesthetics (PTIFA)–an international educational organization that teaches physicians, dentists and nurses in the field of botulinum toxin, dermal fillers and facial aesthetics. Over the last 10+ years, Dr. Roberts has been a leading voice for raising the standard of patient care using botulinum toxin–both therapeutically and cosmetically. His educational model has been used by colleges to develop the “Standard of Practice” for facial aesthetic procedures. Dr. Roberts has developed a number of injection techniques and templates that make the patient experience remarkable. He is continuously recognized by Dentistry Today as one of the top 100 CE speakers. For more information, visit PTIFA.com.
 Dr. Jan Roberts is the Co-Founder and Senior Clinical Instructor for PTIFA. Dr. Roberts is a top cosmetic dentist in Vancouver and has been in practice for 35+ years. She is currently in the final stages of her AACD accreditation. It is this drive for excellence that means that Dr. Roberts is always on the forefront of new advancements. She is currently the leading voice on how the combination of cosmetic dentistry and facial rejuvenation treatments can work together to push patient satisfaction to the next level. Through her work with PTIFA, she is creating a new understanding of how doctors can achieve better outcomes in therapeutic and cosmetic cases with the two disciplines working together. As a result, Dr. Roberts is in demand as a speaker, and an author having published several articles for international and national publications, including Dentistry Today, Teamwork and Oral Health.
Dr. Jan Roberts is the Co-Founder and Senior Clinical Instructor for PTIFA. Dr. Roberts is a top cosmetic dentist in Vancouver and has been in practice for 35+ years. She is currently in the final stages of her AACD accreditation. It is this drive for excellence that means that Dr. Roberts is always on the forefront of new advancements. She is currently the leading voice on how the combination of cosmetic dentistry and facial rejuvenation treatments can work together to push patient satisfaction to the next level. Through her work with PTIFA, she is creating a new understanding of how doctors can achieve better outcomes in therapeutic and cosmetic cases with the two disciplines working together. As a result, Dr. Roberts is in demand as a speaker, and an author having published several articles for international and national publications, including Dentistry Today, Teamwork and Oral Health.












