
Burning mouth syndrome (BMS) is a pain condition discussed in the dental literature as a disorder isolated to the mouth, but it is more easily understood as part of a larger family of burning syndromes that have unique features and locations because of the type of nerve cell that is malfunctioning.
In BMS small, C-type neurons that transmit temperature and burning from the mouth to the brain are “misbehaving”. They are turning “on” spontaneously at the level of the brainstem. There is no actual damage to the skin of the mouth, which is why BMS has been so difficult to understand and the patients have often been thought to have a psychiatric problem. In the normal state the brainstem neurons wait quietly in the “off” state until a specific temperature message from the skin comes along, then they send a burning message to the brain. But under certain circumstances, for example if they are missing key metabolic factors needed for their normal function, the neurons become “hyper-excitable” and they send burning messages when there is no skin injury. Surprisingly, the metabolic elements they are missing are all inexorably linked to the bacteria of our gut microbiome, and returning the gut microbiome and vitamin D levels to normal can bring about a complete resolution of BMS. (see below)
PATIENT EXAMPLE
Michelle S. MSDH, RDH is a 41-year-old dental hygienist with no pregnancies and no medical problems aside from intermittent irritable bowel syndrome (IBS). She started to have burning of the anterior ½ of her tongue in 2018. After meeting the author at a conference in fall of 2018 she had her first vitamin D blood level performed and despite being an avid paddleboarder, she was surprised to find that she had a vitamin D level of 17ng/ml. (Lab normals are variable but are generally 30-100 ng/ml.) In 2019 she had abdominal surgery for bowel obstruction. A volvulus due to congenitally shortened mesentery was removed, with improvement in her IBS symptoms. She started on vitamin D supplementation but irregularly and in unclear dose, without any resolution of her mouth burning.
In late 2021 she continued to have tongue burning and started on the RightSleep Program. (Her B12 was normal, over 1000 pg/ml). She began a vitamin D dose of 15,000 IU/day, B50 and a multivitamin and had rapid resolution of her burning tongue as soon as she started B50. By 2021 her IBS symptoms had also returned and those improved with starting D and B50. Follow-up D level 2/2021 after 2-3 months of 15,000 IU’s of D/day was 78ng/ml. She reduced her D dose to 5000 IU/day and follow-up D level in 8/2021 was 51. No follow-up D levels were done until she had return of burning mouth in 3/2022 and a D level done 4/2022 was 46 (irregular dosing). She restarted B50 and 5000 IU’s of D and her burning resolved in 2 weeks. She’s had no further recurrence of mouth burning, but continues to have intermittent IBS symptoms.
HISTORY OF BURNING MOUTH SYNDROME
Most authors have described BMS as intractable and minimally responsive to treatment, its cause unknown.1-8 It has been reported in association with B12 and vitamin D deficiency states, psychiatric disorders such as depression and anxiety, as well as other “inflammatory” conditions; cardiac disease and auto-immune disorders.3-8 It is now clear that the cause of BMS, and the other associated disorders can both be traced back to deficiencies that we can develop when vitamin D levels are low for extended periods and we lose the normal, healthy bacterial species of the intestinal microbiome. The medical conditions and sensory disorders are ultimately linked to a deficiency of the neurotransmitter acetylcholine at specific locations.9
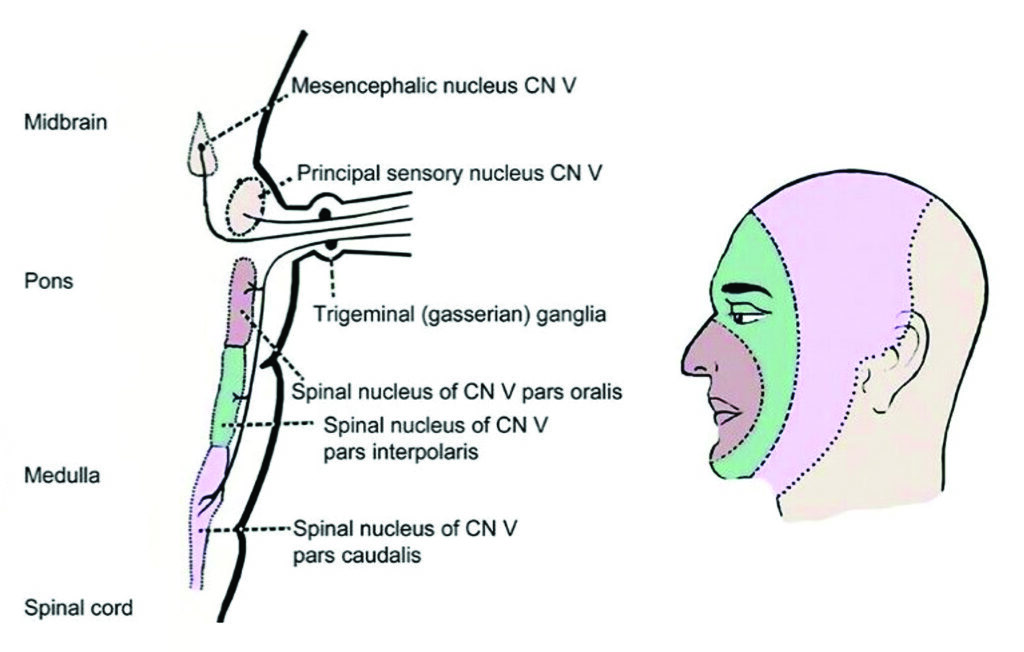
Fig. 1
CLINICAL PRESENTATION
The burning of BMS often starts at the tip of the tongue spreading out bilaterally to the lips and mouth in an “onion skin distribution”. This distribution represents a central, brainstem location of the small, C-fiber neurons of the spinal nucleus of cranial nerve V, which becomes the trigeminal nerve, but the sensory derangement does not follow a “trigeminal distribution”.
The burning pain of BMS is distinguished from the tingling (not burning) and blisters that identify an outbreak of herpes simplex on the lips and mouth, and the trigeminal distribution of lancinating, stabbing pains that characterizes trigeminal neuralgia.
OTHER PRESENTATIONS OF BURNING CAUSED BY MISBEHAVING C-FIBERS
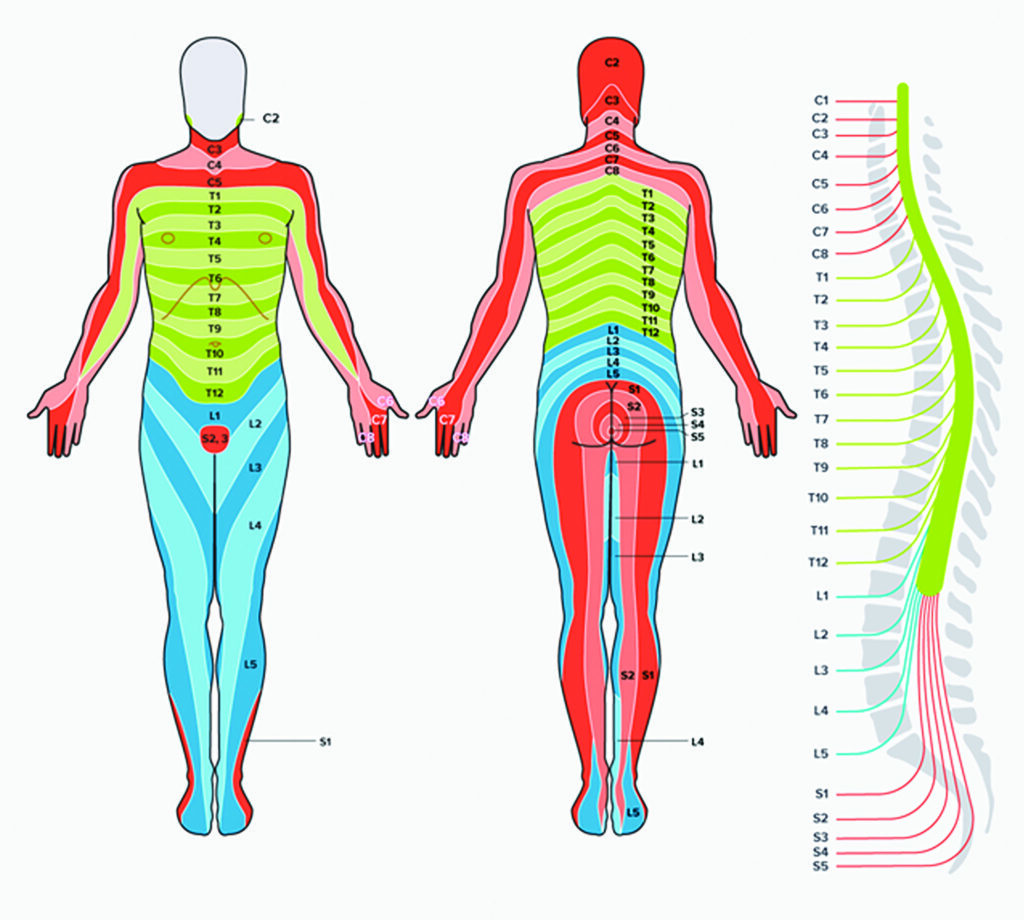
There are many other presentations of the same burning pain, usually in nerve root patterns, usually bilateral, but remaining in a specific, focal location unique to each patient, rarely spreading out to become generalized. (personal observations)
- bilateral cervical roots radiating down the arms
- bilateral thoracic roots encircling the chest
- “saddle-distribution”; sacral roots, buttocks
- “sciatic-distribution”; buttocks, back of the legs
- bottom of the feet
- feet plus the perineum
- palms of the hands, soles of the feet
The mouth, palms of the hands, soles of the feet and perineum have the highest density of the C-type pain/temperature fibers, which is probably why burning in the hands and feet together is also one of the possible presentations.10 Though the burning is usually concentrated symmetrically in a particular body part, patients also describe accompanying ‘’pokey-pains” “needle-stabs” or “pin-pricks” that are irregular and fleeting in other parts of the body. These represent spontaneous firing of the same C-type neurons but in areas where there are fewer fibers per square inch, such as the back or chest. A single cell misfiring is perceived as a “stab” but a group of fibers all turning on together is felt as burning, or with less intensity, itching or warmth. These clinical syndromes are usually called ‘’small fiber neuropathies” but as discussed, they are not really happening in the peripheral nerve.11-13
Frequently, burning in the feet is most noticeable at bed time, when the feet are no longer in contact with socks or the floor. The other distinctive features are that the patient wants to cool the skin of the involved area, putting ice on the mouth or the feet. These C-type sensory neurons that are misbehaving are affected by temperature and their firing rate is decreased by cooling and enhanced by heating.14,15 They are also part of the temperature-sensing autonomic pathway that adjusts capillary flow to the skin in response to hot or cold so malfunction of these fibers can lead to white or red to purplish discoloration of isolated fingers or toes, recently called ‘’Covid toe” in association with burning pain.16
If bladder hypersensitivity accompanies perineal burning or foot burning the patient may have been told that they have another diagnosis, “interstitial cystitis”. A poorly understood hyper-reactivity of the bladder. If refractory burning and itching involves the peri-vaginal area or the skin of the penis or scrotum the patient may have been told that they have ‘’lichen planus” of that area, a poorly understood skin disorder. Both symptoms of bladder hypersensitivity and chronic, unexplained perineal burning and itching have resolved together with treatment. (personal observations)
BURNING FEET AND “DIABETIC NEUROPATHY”
The most common presentation of burning is both feet, which has historically been blamed on diabetes where possible. However, the same complaint occurs just as frequently in those without diabetes, and the overly simplistic dogma of ‘’the sugar hurts the nerves”, used to explain coexistence of diabetes and burning feet doesn’t hold up when normalization of sugar levels doesn’t usually change the burning.17 Burning of the feet has also been grouped with other “length-dependent neuropathies”, inherited and diabetes-related neuropathies characterized by reduced sensation in the feet. Burning of the type discussed here is not a “neuropathy” it is a central disorder of hyper-excitability of neurons and can occur in an identical form around the mouth belying the proposed ‘’length dependent” relationship.1-8, 11-13
Fig. 2
CLINICAL OBSERVATIONS AND THE DISCOVERY OF D/B5 RELATED BURNING
In 2013 several patients who had been participating in a 2-year trial of vitamin D and B12 supplementation to improve sleep18 developed unexplained burning of the hands and feet. Further investigation led to articles about B5 deficiency and burning. In the 1950s pantothenic acid deficiency was induced by giving an oral pantothenic acid blocker for two weeks.19 Participants rapidly developed symptoms of insomnia, a puppet-like gait and burning in the hands and feet. With these articles as support, supplementation with B5 and a large dose B complex called B100 (100 mg or mcg of each of 8 B’s) was recommended and burning pain resolved within days. (personal observations)
The affected patients apparently became B5 deficient at the end of two years of D and B12 supplementation but had no accompanying change in diet. However, they did have accompanying irritable bowel syndrome suggesting that their gut microbiome was abnormal.20 Articles about the source of the B vitamins confirmed that each of the eight B vitamin are made by the normal human gut bacteria suggesting that the patients’ abnormal gut bacteria were not supplying enough B5 and once B5 stores were depleted a B5 deficiency symptoms occurred.21-23
VITAMIN D DEFICIENCY CAUSES AN ABNORMAL GUT MICROBIOME
Over the last 50 years vitamin D deficiency has become the norm. We are advised to avoid sun exposure and since the advent of air conditioning and computers our lives are spent largely indoors. Even farmers plow their fields from air-conditioned tractors. The resultant vitamin D deficiency means a lower supply of vitamin D to the gut bacteria, and because the normal, healthy bacterial species of the gut require vitamin D there has been an accompanying, unhealthy change in our gut bacteria towards species that don’t require D.24-28 (The use of antibiotics has been blamed for this change but is not the primary cause.)
The D-related change in gut bacterial populations has a myriad of effects but one of the most important is that as the species living inside us change, we lose our normal supply of the 8 B vitamins. The B vitamins do not come directly from the food we eat, they are produced in specific amounts by our gut bacteria.21,29,30 Change in the gut bacterial populations upends the normal supply of B’s and leads to deficiencies in several B vitamins at once.
CLINICAL USE OF THE B VITAMINS – DISPELLING THE MYTHS
Both BMS and burning of the hands and feet have been reported in the setting of B12 and B5 deficiency.2,4,19 But, unfortunately, in the 1980’s Medicine arbitrarily decided that “if you have a good diet, you don’t need vitamins” and that vitamins were no longer related to the practice of Medicine. Therefore, valid published scientific and clinical observations regarding 1) the lack of relevance of B vitamin blood levels in assessing deficiency states and 2) the presence of B vitamin body stores, have been ignored or forgotten.22,23 Also unfounded, incorrect statements are widely published in the current literature; “B5 deficiency doesn’t exist because it’s in every food”.21 Luckily there has been a recent resurgence in scientific articles in the human and veterinary literature about signs and symptoms of B5 deficiency, reporting B5-related abnormal gait in pigs and pathological studies documenting B5 deficiency in several pertinent areas of the brain.31-33 These support the observation that over the last 40 years, since D deficiency has become the norm, there has been an accompanying epidemic of B5 deficiency disorders. Because B vitamin blood levels bear no relationship to cellular deficiency states clinical symptoms appear to be the only reliable way to assess B5 deficiency of the nervous system.9
USING THE B VITAMINS TO TREAT CLINICAL SYMPTOMS
It is important to understand that the B vitamins are needed for hundreds of cellular processes. The dogma before the 1980’s was ‘’If you give one B vitamin you should give all of them”. The B vitamins are interdependent for both production by the gut bacteria, who secrete them into our gut lumen, and in our cellular processes once we absorb them. Thus, the pharmaceutical use of individual B’s needs to be re-evaluated and the historical custom of giving all 8 B’s together also needs to be re-considered in view of the current knowledge of the gut microbiome production.
We now know that there are many other important metabolites made and supplied by our gut bacteria that we must absorb and use in order to function normally. In other words, there are lots of newly discovered metabolites produced by the gut bacteria that we haven’t named “vitamins”. And they are certainly not ‘’extra’’ or something that ‘’we don’t need if we have a good diet” they are absolutely required for normal health. There are bacterial products that we absorb that regulate our mineral 4absorption and storage, allowing our body to know if it is in iron overload or iron deficiency.34 There are other bacterial products that are the building blocks which become the endocannabinoids, necessary for normal brain and spinal cord development in childhood, as well as ongoing normal pain perception, appetite, sleep and inflammatory response.35
CONCLUSIONS
The last ten years of experience returning the gut microbiome to normal function and watching the effect of the B vitamins on sleep, mood, burning, autonomic function, including bladder and bowel function supports the idea that many of the medical problems we are currently treating with pharmaceuticals are really deficiency states that can be reversed slowly by maintaining a healthier vitamin D blood level, converting the microbiome to normal and optimizing repair in sleep.9
Though BMS is not a daily event in routine dental practice, for a patient with BMS the confirmation that it is not a psychosomatic disorder but is in fact a treatable condition can be life-changing!
To watch a video about the origins of the RightSleep Program go here. To read more about the scientific basis of RightSleep and the connections of vitamin D and B vitamins to routine dental practice go to www.drgominak.com.
Oral Health welcomes this original article.
References:
- Burning mouth syndrome: A review on its diagnostic and therapeutic approach. Aravindhan R, Vidyalakshmi S, Kumar MS, Satheesh C, Balasubramanium AM, Prasad VS. J Pharm Bioallied Sci. 2014 Jul; 6(Suppl 1): S21–S25. doi: 10.4103/0975-7406.137255
- Burning mouth syndrome: results of screening tests for vitamin and mineral deficiencies, thyroid hormone, and glucose levels-experience at Mayo Clinic over a decade. Morr-Verenzuela C , Davis M, Bruce AJ, Torgerson RR. Int J Dermatol. 2017 Sep;56(9):952-956.doi: 10.1111/ijd.13634.
- Non-Communicable Diseases and Associated Risk Factors in Burning Mouth Syndrome Patients. Parlatescu I, Dugan C, Popescu BO, Tovaru S, Dobre M, Milanesi E. Medicina (Kaunas). 2023 Nov 27;59(12):2085. doi: 10.3390/medicina59122085.
- Hypovitaminosis D, objective oral dryness, and fungal hyphae as three precipitating factors for a subset of secondary burning mouth syndrome. Gu Y, Baldwin S, Canning C. Heliyon 2023 Sep 7;9(9):e19954.doi: 10.1016/j.heliyon.2023.e19954.
- Anemia, hematinic deficiencies, and hyper-homocysteinemia in younger and older burning mouth syndrome patients. Wu YH, Wu YC, Chang J, Lang MJ, Chiang CP, Sun A. J Dent Sci. 2022 Jul;17(3):1144-1150. doi: 10.1016/j.jds.2022.02.005.
- Effects of self-perceived psychological stress on clinical symptoms, cortisol, and cortisol/ACTH ratio in patients with burning mouth syndrome. Lee YH, Suk C. BMC Oral Health 2023 Jul 22;23(1):513. doi: 10.1186/s12903-023-03235-0
- Psychiatric comorbidities in chronic orofacial pain during COVID-19 pandemic. Maeda C, Watanebe M, Huyen Tu TT, et al. J Psychosom Res. 2023Sep:172:111420.doi:10.1016/j.jpsychores.2023.111420.
- Exploring the Association of Burning Mouth Syndrome with Depressive and Anxiety Disorders in Middle-Aged and Older Adults: A Systematic Review. Dibello V, Ballini A, Lozupone M, et al. J Pers Med. 2023 Jun 19;13(6):1014. doi: 10.3390/jpm13061014.
- Vitamin D deficiency changes the intestinal microbiome reducing B vitamin production in the gut. The resulting lack of pantothenic acid adversely affects the immune system, producing a “pro-inflammatory” state associated with atherosclerosis and autoimmunity. Gominak SC. Med Hypotheses. 2016 Sep;94:103-7. doi: 10.1016/j.mehy.2016.07.007.
- Sensory Processing: Tactile innervation densities across the whole body. Corniani G, Saal HP. J Neurophysiol 124: 1229–1240, 2020.doi:10.1152/jn.00313.2020
- Case-control study of small-fiber neuropathies, with regards on smoking and vitamin D deficiency and other possible causes. Fouchard M, Brenaut E, Genestet S, Ficheux A-S, Marcorelles P, Misery L (2023) Observational Front. Med. 9:1051967. doi: 10.3389/fmed.2022.1051967
- Non-length-dependent small fiber neuropathy: Not a matter of stockings and gloves. Gemignani F, Bellanova MF, Saccani E, Pavesi G. Muscle Nerve 2022 Jan;65(1):10-28.doi: 10.1002/mus.27379.
- Small fiber neuropathy: Swiss cohort characterization. Bitzi LM, Lehnick D, Wilder-Smith EP. Muscle Nerve. 2021 Sep;64(3):293-300. doi: 10.1002/mus.27340.
- Novel classes of responsive and unresponsive C nociceptors in human skin. Schmidt R, Schmelz M, Forster C, Ringkamp M, Torebjörk E, Handwerker H. J Neurosci. 1995 Jan;15(1 Pt 1):333-41.doi: 10.1523/JNEUROSCI.15-01-00333.1995.
- Endothelin 1 activates and sensitizes human C-nociceptors. Namer B, Hilliges M, Ørstavik K, et al. Pain. 2008 Jul;137(1):41-49. doi: 10.1016/j.pain.2007.08.008.
- Architecture of the Cutaneous Autonomic Nervous System. Glatte P, Buchmann SJ, Hijazi MM, Illigens B, Siepmann T. Front Neurol. 2019; 10: 970.doi: 10.3389/fneur.2019.00970
- Burning through the pain: treatments for diabetic neuropathy. Javed S, Alam U, Malik RA. Diabetes Obes Metab. 2015 Dec;17(12):1115-25. doi: 10.1111/dom.12535.
- The world epidemic of sleep disorders is linked to vitamin D deficiency. Gominak SC, Stumpf WE. Med Hypotheses. 2012 Aug;79(2):132-5. doi: 10.1016/j.mehy.2012.03.031. Epub 2012 May 13. PMID: 22583560
- Pantothenic acid deficiency induced in human subjects. Bean WB, Hodges RE, Daum K. J Clin Invest 1955;34(7):1073–84.
- Gut microbiota and common gastrointestinal diseases: a bidirectional two-sample Mendelian randomized study. Qiu B, Shen Z, Yang D, Qin X, Ren W, Wang Q. Front Microbiol. 2023 Nov 17;14:1273269. doi: 10.3389/fmicb.2023.1273269
- Intestinal absorption of water-soluble vitamins in health and disease. Said H. Biochem J 2011;437:357–72.
- Metabolic response to a pantothenic acid deficient diet in humans. Fry PC, Fox HM, Tao HG. J Nutr Sci Vitaminol 1976;22:339–46
- Availability of vitamin B6 and pantothenate in an average American diet in man. Tarr JB, Tsanenobu T, Stokstad ELR. Am J Clin Nutr 1981;34:1328–37.
- The Effect of Various Doses of Oral Vitamin D3 Supplementation on Gut Microbiota in Healthy Adults: A Randomized, Double-blinded, Dose-response Study. Charoenngam N, Shirvani A, Kalajian TA, Song A, Holick MF. Anticancer Research 40: 551-556 (2020) doi:10.21873/anticanres.13984
- Gut microbiota interactions with the immunomodulatory role of vitamin D in normal individuals. Luthold RV, Fernandes GR, Franco-de-Moraes AC, Folchetti LG, Ferreira SR. Metabolism. 2017 Apr;69:76-86. doi: 10.1016/j.metabol.2017.01.007.
- Relationships Between Vitamin D, Gut Microbiome, and Systemic Autoimmunity. Yamamoto EA, Jørgensen TN. Front Immunol. 2020 Jan 21;10:3141. doi: 10.3389/fimmu.2019.03141.
- Effects of high doses of vitamin D3 on mucosa-associated gut microbiome vary between regions of the human gastrointestinal tract. Bashir M, Prietl B, Tauschmann M, et al. Eur J Nutr (2016) 55:1479–1489 doi 10.1007/s00394-015-0966-2
- Role of Vitamin D in the Hygiene Hypothesis: The Interplay between Vitamin D, Vitamin D Receptors, Gut Microbiota, and Immune Response. Clark A, Mach N. Front Immunol. 2016 Dec 23;7:627. doi:10.3389/fimmu.2016.00627.
- B vitamin acquisition by gut commensal bacteria. Putnam EE, Goodman AL. PLoS Pathog. 2020 Jan 23;16(1):e1008208. doi: 10.1371/journal.ppat.1008208.
- Systematic genome assessment of B-vitamin biosynthesis suggests co-operation among gut microbes. Magnúsdóttir S, Ravcheev D, de Crécy-Lagard V, Thiele I. Front. Genet. 2015 6:148.doi: 10.3389/fgene.2015.00148
- Motor and somatosensory degenerative myelopathy responsive to pantothenic acid in piglets. Lorenzett MP, Armién AG , Henker LC. Veterinary Pathology 2023, Vol. 60(1) 101 –114
- Cerebral deficiency of vitamin B5 (d-pantothenic acid; pantothenate) as a potentially-reversible cause of neurodegeneration and dementia in sporadic Alzheimer’s disease. Xu J, Patassini S, Begley P, et al. Biochem Biophys Res Commun. 2020 Jun 30;527(3):676-681. doi: 10.1016/j.bbrc.2020.05.015.
- Coenzyme A-Dependent Tricarboxylic Acid Cycle Enzymes Are Decreased in Alzheimer’s Disease Consistent with Cerebral Pantothenate Deficiency. Sang C, Philbert SA, Hartland D, et al. Neurosci 2022 Jun 10;14:893159.
- Microbial metabolite signaling is required for systemic iron homeostasis. Das NK, Schwartz AJ, Barthel G, et al. Cell Metab. 2020 January 07; 31(1): 115–130.e6. doi:10.1016/j.cmet.2019.10.005.
- Altered gut microbiota and endocannabinoid system tone in vitamin D deficiency-mediated chronic pain. Guida F, Boccella S, Belardo C, et al. Brain Behav Immun. 2020 Mar;85:128-141. doi: 10.1016/j.bbi.2019.04.006.
About the Author:

Dr. Stasha Gominak attended Baylor College of Medicine and received an MD degree in 1983. Her Neurology residency was done at the Harvard-affiliated Massachusetts General Hospital in Boston. She practiced Neurology in the San Francisco Bay area from 1991-2004 and then moved to Tyler, Texas with her husband. Starting in 2004 she began to dedicate more of her practice to the treatment of sleep and sleep disorders. In 2012 and 2016, she published two pivotal articles about the global struggle with worsening sleep, the possible causes and solutions related to vitamin D deficiency and the intestinal microbiome. In 2016 she retired from her office practice to have more time to teach.









