A good light curing unit (LCU) is required to activate the photoinitiator(s) in the resin-bonded composite (RBC) and transform it into a durable, functional restoration.1-3 The international standard ISO 40494 stresses that the RBC should be properly photocured according to the instructions of the manufacturer of the RBC (not the LCU) and no resin manufacturer recommends undercuring their RBC, or using a 1 s exposure. With advancements in light-curing technology, the dental profession now benefits from a wide range of LCUs to photocure the RBC. This article provides an overview of the technology, attributes, and clinical applications of LCUs with special attention to choosing and optimizing LCUs for various procedures to improve patient care and optimize clinical outcomes.
Historical perspective
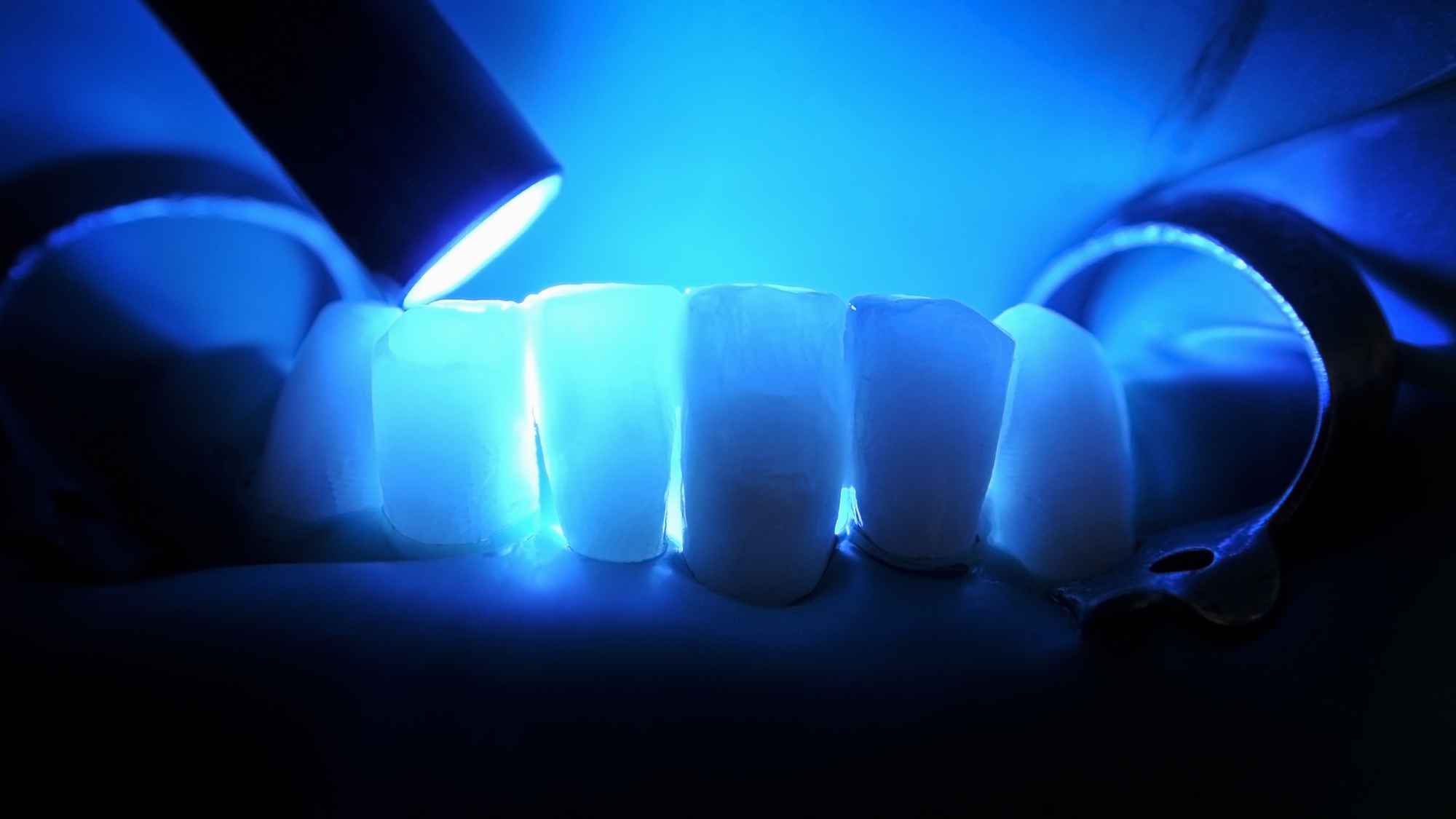
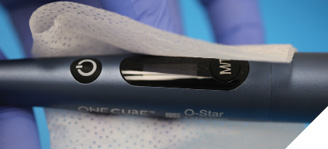
Quartz-tungsten-halogen (QTH) curing lights were initially used to photocure RBCs. However, they were inefficient; the bulb and reflector had a short lifespan, and the LCUs were prone to overheating. Photo-curing the resin used to take as long as 40-60 seconds for each RBC increment.5 The halogen bulbs used in these LCUs are now being phased out, and light-emitting diode (LED) technology is used in most LCUs. LEDs offer improved energy efficiency, a longer lifespan, and a focused wavelength output. LED technology is also improving, and, as illustrated in Figure 1, a Woodpecker light made 10 years ago is not the same as the current generation Woodpecker X-Star curing light (Oral Science, Brossard, Quebec). In addition, Class 4 laser-diode LCUs such as the Monet from AMD (West Jordan, UT, USA) are available and claim to offer short exposure times.6 However, they are expensive, have a smaller spot size, a narrow emission spectrum, and require additional laser certification.
Fig. 1

Although some LCU manufacturers claim an adequate cure in just one second, most peer-reviewed dental articles7-11 do not support a one-second exposure time, and these conflicting claims confuse the clinician. The authors recommended that clinicians review the Instructions For Use (IFUs) provided by both the LCU and resin manufacturers and not go “off-label” when photocuring the RBC.12
Regulatory compliance
Dental curing lights are classified as medical devices13-15 and are subject to government regulation (FDA in the US and Health Canada in Canada). Using an unlicensed medical device on a patient can result in adverse legal or ethical consequences for the dentist. Some retailers may sell products that do not meet the necessary regulatory standards, and some of these LCUs are so cheap that it is questionable whether any of their claims are accurate.16, 17 Therefore, when buying any medical device, verifying that the product has been tested and validated for use on a patient is essential.15 Of note, no medical device should be advertised as “FDA approved or cleared.” This is considered misbranding by the FDA under section 21 CFR 807.97.18
Fundamentals of light polymerization
Two fundamental photochemical laws govern the polymerization reaction that converts resin monomers to a solid polymer matrix:2, 8
- Grotthuss-Draper Law: Light must first be absorbed for a photochemical reaction to occur.
- Stark-Einstein Law: One photon of light activates only one molecule.
Thus, successful photocuring requires that the LCU deliver the correct wavelengths of light to the initiator, sufficient irradiance (mW/cm²), and an adequate radiant exposure (J/cm²).
Spectral matching
According to the Grotthuss-Draper Law, the compatibility of the LCU light wavelengths with the resin photoinitiators is critical. If the LCU wavelengths do not match the absorption characteristics of the photoinitiator, the resin will not polymerize, no matter how high the irradiance or how much light is delivered.
Camphorquinone (CQ) is the most common photoinitiator used in dental resins. CQ absorbs light in the 400–500 nm range, with a peak absorbance at ~470 nm.1-3 Some companies have developed resins that use a combination of CQ and alternative photoinitiators such as Lucirin TPO and Ivocerin™ (Ivoclar, Buffalo, NY) that are more efficient and require fewer photons to produce free radicals.19 These photoinitiators do not require co-initiators, they are less yellow in color and have higher absorptivity, but they are most sensitive to violet light, not blue light. While they are activated by QTH lights, most single-peak LED and laser diode LCUs do not emit violet light and thus do not activate most of these initiators (Fig. 2).
Fig. 2
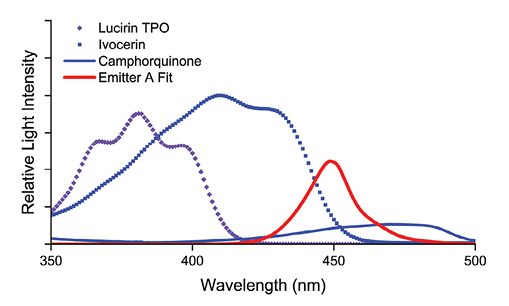
To overcome this problem, some LCU manufacturers use a combination of violet and blue LEDs, making their LCUs multiple-peak, or polywave™ (Fig. 3).
Fig. 3
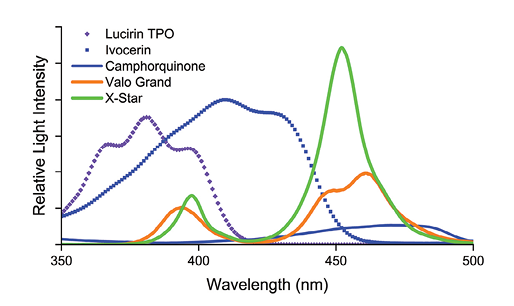
While polywave/multiple peak LCUs may deliver improved polymerization of RBCs,20-22 violet light does not penetrate RBCs or ceramics very well. Little or no violet light reaches the bottom of 4mm of RBC.23-25 Thus, a single peak LCU may deliver greater depths of cure than a polywave/multiple peak LCU of the same power, because it emits more blue light and delivers more energy to the CQ initiator at the bottom of the RBC.
Dental radiometer
Dentists should purchase a good dental radiometer to monitor that their LCU is functioning correctly and can deliver a sufficient number of photons to photocure the RBC (Stark-Einstein Law).
Figure 4 illustrates two recommended dental radiometers. The Bluephase Meter II (Ivoclar Vivadent, Buffalo NY) can measure radiant power (mW) from 380–550nm within ±10% compared to a laboratory-grade meter.26, 27 When the light tip diameter is included, it can also report the irradiance (mW/cm2). An alternative radiometer, the CheckUP.28, 29 (BlueLight Analytics Halifax, Nova Scotia, Canada) provides an irradiance value and recommended exposure times for the specific LCU and RBC.
Fig. 4

Effect of distance
At the light tip, the radiant exitance equals the irradiance (both are reported in mW/cm2). However, as the RBC distance from the light tip increases, the irradiance usually decreases. Since LCU emissions are focused beams of light, this reduction does not follow the ‘inverse-square law’. Figure 5 illustrates the effect of distance from the light tip on the irradiance received at the RBC, showing how the distance effect varies between three LCUs.
Fig. 5
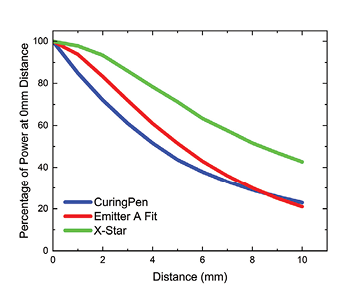
It can be seen that irradiance measurements at 0mm give little indication of the irradiance at 10mm. In this image, the X-Star light (Oral Science, Brossard, QU) is less affected by distance compared to the Curing Pen (Sifary Medical Technology Co., Ltd., Changzhou City, Jiangsu Province, China) or the Emitter A Fit (Schuster, Santa Maria, RS, Brazil). Since the light tip may easily be 6 to 8mm away from the resin at the bottom of a proximal box,30 manufacturers should ideally report their LCU irradiance at clinically relevant distances (8mm) from the light tip. Given this information, the dentist can increase the exposure time to deliver sufficient energy to the RBC.
Heat generation
Excessive heat during light curing can harm the soft tissues and the pulp, especially in deep cavities. As LCUs have become ever more powerful and with large diameter light tips, the potential for causing direct heat and radiant thermal damage to soft tissues and dental pulp has increased.31-34 Figure 6 illustrates the problem that can occur when using a high-power LCU that has a wide light tip. The wide tip will also deliver light to the gingival tissues (A) and this may cause a burn (B).
Fig. 6AB

A simple test to determine how much heat the LCU delivers is to test the end of the LCU on the dentist’s tongue or lips for the typical clinical RBC curing time. This readily demonstrates oral tissue effects when light-curing gingival Class V areas, the gingival portions of veneers, and crown margins. Thus, the location of the LCU tip must be monitored, and exposure duration must not be arbitrarily increased. Intermittent exposure cycles or directing a stream of air across the tooth will minimize the thermal risks of using a high-power LCU.35, 36
Beam uniformity
LCU light beam profile measurement assesses the:
- Light beam uniformity.
- Spectral radiant power distribution across the light beam.
- Effect of distance on the irradiance received.3, 37
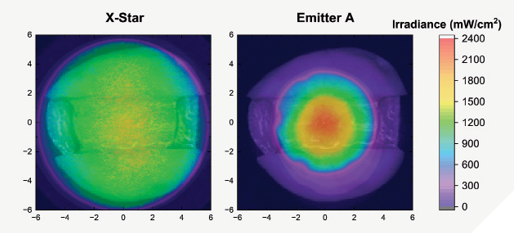
LCUs with well-designed internal optics produce well-collimated beams: in poorly designed LCUs the inhomogeneous beam profile causes a rapid dispersion of light with distance from the light tip.37, 38 This leads to uneven RBC curing (well-polymerized center and insufficiently cured edges).7, 39-42 Figure 7 illustrates the irradiance beam profile of the Woodpecker X-star (uniform beam profile, without hot spots of high/low irradiance, producing a more uniform cure across the entire RBC) and the Schuster Emitter A (inhomogeneous light distribution, a lower irradiance is delivered to the cavity’s proximal boxes) superimposed over a molar tooth.37, 41
Fig. 7
Access to the restoration
Figures 8 and 9 illustrate how the light guide size and/or shape can make light tip access to certain areas of the mouth difficult,37, 43, 44 significantly affecting irradiance, and even the light wavelength reaching the RBC. A low-profile head such as from the Woodpecker X-Star, can access the lingual of mandibular posterior and the anterior teeth (Fig. 9). Thus, the high irradiance values in the laboratory or at a sales booth may not be repeatable if the light tip cannot be placed perpendicularly (Fig.8A) over the restoration.45-47
Fig. 8
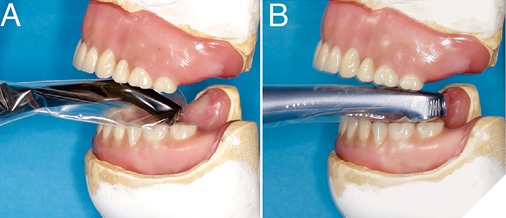
Fig. 9

The Optical “Blue Light Hazard”
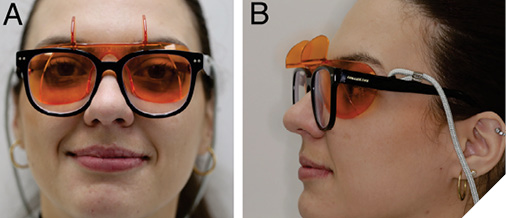
Chronic exposure to artificial blue light may disrupt sleep patterns, accelerate retinal aging, and cause age-related macular degeneration (ARMD) in humans.48-50 These effects have been termed “The Blue Light Hazard,” with the greatest risk occurring between 415 and 480 nm, peaking at 440nm.51, 52 This wavelength range falls within the emission spectra of all dental curing lights,37, 53 notably the LED curing lights. Given the concerns about the potential risks of blue light, appropriate eye protection should always be used with dental curing lights.53, 54
Most manufacturers supply acceptable blue-blocking orange shields to protect the eyes. These orange plastic shields may be attached to the light tip and adjusted in any direction to maximize eye protection. Protective glasses and paddles are also available in various sizes, thicknesses, and designs. Figure 10 shows behind-the-glasses Ease-in-Shields (Ultradent South Jordan, UT, USA) that allow clinicians to watch the light tip position when light curing, even when wearing loupes.
Fig. 10
Infection control
Although some fiber-optic light guides can be autoclaved,55, 56 the body of the curing light itself cannot. Therefore, plastic barriers should cover the entire curing light and light guides. To minimize light output reduction, the barrier must fit tightly and smoothly, with no seams or wrinkles, over the tip end as illustrated in Figure 11.57
Fig. 11
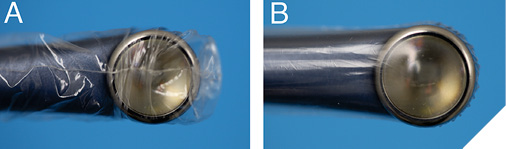
While third-party or inappropriate barriers reduce light output by up to 40%,28, 57-60 even a good barrier will decrease it by 5-10%.57 Thus, the LCU output should be tested on a radiometer with and without the barrier over the light tip so that the clinician can assess the amount of light loss and increase the exposure duration.61
In addition to using barrier sleeves, the LCU body must still be disinfected between patients (Fig. 12). Since some disinfectants can damage the light guide, the body, or the stabilizing ‘O’-rings, only manufacturer-approved disinfectants should be used. If the light guide is detachable, the lens, reflector, and filter inside the curing light and both ends of the light guide should be checked periodically to ensure that they are clean and undamaged.1 If damage is observed, the curing light should be serviced.
Fig. 12
Challenges and emerging trends
Deep cavities and shaded areas challenge adequate curing. Emerging intelligent curing lights, such as the Loop from Garrison (Spring Lake, MI, USA) and the Bluephase G4 and PowerCure from Ivoclar (Buffalo, NY), provide real-time feedback on how well the operator uses them (Fig. 13).
Fig. 13

In some of these new LCUs, if the light tip moves far enough away from the tooth, the LCU first vibrates, and then it turns off, thus warning the operator that they are no longer over the tooth. This feature is similar to the “lane assist” technology in cars and should help the user to keep the LCU over the resin. In others, if the distance between the light tip and the RBC increases, the LCU increases its output. These lights are relatively new, and time will tell if dentists find this feature useful.
General recommendations when using a curing light
Figure 14 illustrates some recommended LCUs from major manufacturers that a clinician should feel confident purchasing.
Fig. 14

Clinicians should follow the following guidelines to ensure the effective and safe use of curing lights in dental procedures.1, 37, 62 These guidelines are available in pictorial form from https://www.cda-adc.ca/en/services/essentials/2016/issue6/index.html#30 and can be easily printed for your office staff:62
- Use only LCUs that have been accepted for use by your regulatory authorities.
- Understand the LCU’s power output, beam profile, irradiance, and emission spectrum.
- Read the ‘Instructions For Use (IFU)’ from both the manufacturer of the LCU and RBC before using them on your patients.
- Regularly check the light output using a radiometer.
- Ensure alternative curing methods are available if the primary LCU malfunctions or the batteries die.
- Deliver sufficient radiant exposure at the correct wavelength for the RBC.
- Hold the light tip close to, and perpendicular to, the restoration. Avoid shadows.
- Use appropriate eye protection so that you can watch what you are doing when light curing.
- Minimize heat by using air cooling and limiting continuous exposure time.
Conclusions
Delivering enough light at the correct wavelengths is essential for successful resin-based restorations. Understanding the attributes of the LCU and how to use it will help ensure optimal patient outcomes. As technology evolves, clinicians must stay informed and adopt advancements that enhance patient care. 
Oral Health welcomes this original article.
References
- F.A. Rueggeberg, M. Giannini, C.A.G. Arrais, R.B.T. Price, Light curing in dentistry and clinical implications: a literature review, Braz Oral Res 31(suppl 1) (2017) e61. doi:10.1590/1807-3107BOR-2017.vol31.0061.
- D.C. Watts, Light-curing dental resin-based composites: How it works and how you can make it work, Frontiers in Dental Medicine 4 (2023). doi:10.3389/fdmed.2023.1108316.
- M.A. Hadis, A.C. Shortall, W.M. Palin, The power of light – From dental materials processing to diagnostics and therapeutics, Biomater Investig Dent 11 (2024) 40308. doi:10.2340/biid.v11.40308.
- ISO 4049 (2019) Dentistry Polymer-based filling, restorative materials., International Standards Office, Geneva, Switzerland, 2019, p. 27.
- F.A. Rueggeberg, W.F. Caughman, J.W. Curtis, Jr., Effect of light intensity and exposure duration on cure of resin composite, Oper. Dent. 19(1) (1994) 26-32.
- J.C. Comisi, R.B. Price, K. Kinley-Howard, C. Maucoski, E. Rader, Ability of Six Curing Lights to Photocure Four Resin-Based Composites in a MOD-Mold: A Double-Blind Study, Eur. J. Prosthodont. Restor. Dent. 32(3) (2024) 301-313. doi:10.1922/EJPRD_2661Comisi13.
- M.G. Rocha, C. Maucoski, J.F. Roulet, R.B. Price, Depth of cure of 10 resin-based composites light-activated using a laser diode, multi-peak, and single-peak light-emitting diode curing lights, J. Dent. 122 (2022) 104141. doi:10.1016/j.jdent.2022.104141.
- E. Lempel, D. Szebeni, Z. Ori, T. Kiss, J. Szalma, B.V. Lovasz, S. Kunsagi-Mate, K. Boddi, The effect of high-irradiance rapid polymerization on degree of conversion, monomer elution, polymerization shrinkage and porosity of bulk-fill resin composites, Dent. Mater. 39(4) (2023) 442-453. doi:10.1016/j.dental.2023.03.016.
- M. Par, D. Marovic, T. Attin, Z. Tarle, T.T. Taubock, The effect of rapid high-intensity light-curing on micromechanical properties of bulk-fill and conventional resin composites, Sci. Rep. 10(1) (2020) 10560. doi:10.1038/s41598-020-67641-y.
- N.C. Odum, J.T. Ross, N.S. Citrin, D. Tantbirojn, A. Versluis, Fast Curing with High-power Curing Lights Affects Depth of Cure and Post-gel Shrinkage and Increases Temperature in Bulk-fill Composites, Oper. Dent. 48(1) (2023) 98-107. doi:10.2341/21-160-L.
- M. Ribeiro, C. Maucoski, R.B. Price, C.J. Soares, Effect of a 3-second Off-label Exposure on the Depth of Cure of Eight Resin-based Composites, Oper. Dent. 49(4) (2024) 421-431. doi:10.2341/23-155-L.
- FDA, Guidance for Industry and FDA Staff Dental Curing Lights – Premarket Notification [510(k)] Submissions., 2006. https://www.fda.gov/media/74206/download. (Accessed August 5, 2021.
- MDCG, 2021-24 Guidance on classification of medical devices, in: D.-G.f.H.a.F.S. European Commission (Ed.) European Commission, 4 October 2021.
- R.B. Price, J.L. Ferracane, B.W. Darvell, J.F. Roulet, Caveat emptor when purchasing dental products online, J. Am. Dent. Assoc. 153(3) (2022) 196-199. doi:10.1016/j.adaj.2021.10.013.
- R.B. Price, J.L. Ferracane, R. Hickel, B. Sullivan, The light-curing unit: An essential piece of dental equipment, Int. Dent. J. 70(6) (2020) 407-417. doi:10.1111/idj.12582.
- J.E. Harlow, B. Sullivan, A.C. Shortall, D. Labrie, R.B. Price, Characterizing the output settings of dental curing lights, J. Dent. 44 (2016) 20-6. doi:10.1016/j.jdent.2015.10.019.
- FDA, Code of Federal Regulations, Title 21–Food And Drugs Chapter I–Food And Drug Administration Department Of Health And Human Services Subchapter H – Medical Devices Part 872 Dental Devices, 2020. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=872&showFR=1. (Accessed April 1, 2020 Volume 8).
- A. Kowalska, J. Sokolowski, K. Bociong, The Photoinitiators Used in Resin Based Dental Composite-A Review and Future Perspectives, Polymers (Basel) 13(3) (2021). doi:10.3390/polym13030470.
- A. Correa, G. Moro, L.E. Cechin, L. Goncalves, R.O. Rocha, F.Z.M. Soares, Polywave LEDs increase the degree of conversion of composite resins, but not adhesive systems: a systematic review and meta-analysis of in vitro studies, Lasers Med. Sci. 40(1) (2025) 111. doi:10.1007/s10103-025-04368-0.
- R. Elsharawy, M. Elawsya, A. AbdAllah, A. ElEmbaby, Polymerization efficiency of different bulk-fill resin composites cured by monowave and polywave light-curing units: a comparative study, Quintessence Int. 55(4) (2024) 264-272. doi:10.3290/j.qi.b4984231.
- R.B.W. Lima, A. Melo, J.D.N. Dias, L.M.M. Barbosa, J. Santos, G.M. Souza, A.K.M. Andrade, I.V. Assuncao, B.C.D. Borges, Are polywave light-emitting diodes more effective than monowave ones in the photoactivation of resin-based materials containing alternative photoinitiators? A systematic review, J Mech Behav Biomed Mater 143 (2023) 105905. doi:10.1016/j.jmbbm.2023.105905.
- D. Marovic, P. Danicic, G. Bojo, M. Par, Z. Tarle, Monowave vs. Polywave Light – Curing Units: Effect on Light Transmission of Composite without Alternative Photoinitiators, Acta Stomatol. Croat. 58(1) (2024) 30-38. doi:10.15644/asc58/1/3.
- N. Ilie, G. Furtos, A Comparative Study of Light Transmission by Various Dental Restorative Materials and the Tooth Structure, Oper. Dent. 45(4) (2020) 442-452. doi:10.2341/19-037-L.
- J.E. Harlow, F.A. Rueggeberg, D. Labrie, B. Sullivan, R.B. Price, Transmission of violet and blue light through conventional (layered) and bulk cured resin-based composites, J. Dent. 53 (2016) 44-50. doi:10.1016/j.jdent.2016.06.007.
- M. Giannini, C.B. Andre, V.C. Gobbo, F.A. Rueggeberg, Accuracy of Irradiance and Power of Light-Curing Units Measured With Handheld or Laboratory Grade Radiometers, Braz. Dent. J. 30(4) (2019) 397-403. doi:10.1590/0103-6440201902430.
- C. Maucoski, R.B. Price, C.A.G. Arrais, Irradiance from 12 LED light curing units measured using 5 brands of dental radiometers, J Esthet Restor Dent 35(6) (2023) 968-979. doi:10.1111/jerd.13107.
- T.A. Imbery, S.Y. Bergeron, J. Boyle, Radiant Exitance of Old, New, and Damaged LED Light Curing Units, Oper. Dent. 47(6) (2022) 693-700. doi:10.2341/21-177-L.
- D.C. Holmes, W. Lien, C.J. Raimondi, W.L. Hoopes, K.S. Vandewalle, Novel chairside spectrometer-trained system for measuring the irradiance of light-curing units, Gen. Dent. 71(2) (2023) 59-63.
- R.B. Price, T. Derand, M. Sedarous, P. Andreou, R.W. Loney, Effect of distance on the power density from two light guides, J. Esthet. Dent. 12(6) (2000) 320-7. doi:10.1111/j.1708-8240.2000.tb00241.x.
- C. Maucoski, R.B. Price, C.A.G. Arrais, B. Sullivan, In vitro temperature changes in the pulp chamber caused by laser and Quadwave LED-light curing units, Odontology 111(3) (2023) 668-679. doi:10.1007/s10266-022-00780-y.
- J.A.G. Guarneri, M.V.A. Chima, D.G. Assis, F.A. Rueggeberg, C.A.G. Arrais, Influence of light exposure techniques on in vitro pulp temperature rise during bulk fill composite Class I restorations, Odontology 112(2) (2024) 479-488. doi:10.1007/s10266-023-00867-0.
- R.K. Nakagawa, H.H. Araujo de Oliveira, L.G. Abreu, C.A. R, D. Lf, N.M. A, Pulpal Temperature Variances During Step-by-step Adhesive Restorative Procedure Using Three Different High-irradiance Light-curing Units, Oper. Dent. 49(1) (2024) 43-51. doi:10.2341/22-045-L.
- C. Maucoski, D.C. Zarpellon, F.A. Dos Santos, L.C. Lipinski, E.B. Campagnoli, F.A. Rueggeberg, C.A.G. Arrais, Analysis of temperature increase in swine gingiva after exposure to a Polywave((R)) LED light curing unit, Dent. Mater. 33(11) (2017) 1266-1273. doi:10.1016/j.dental.2017.07.021.
- D.C. Zarpellon, P. Runnacles, C. Maucoski, U. Coelho, F.A. Rueggeberg, C. Arrais, Controlling In Vivo, Human Pulp Temperature Rise Caused by LED Curing Light Exposure, Oper. Dent. 44(3) (2019) 235-241. doi:10.2341/17-364-C.
- M. Mouhat, L. Stangvaltaite-Mouhat, E. Finnas, A. Andersen, A.L. Evertsen, B.W. Nilsen, How does indirect air-cooling influence pulp chamber temperature in different volume teeth and absence/presence of resin-based composite during light curing?, BMC Oral Health 22(1) (2022) 538. doi:10.1186/s12903-022-02545-z.
- J.A.G. Guarneri, R.B. Price, C. Maucoski, C.A.G. Arrais, The dark art of light curing in dentistry, J. Dent. 150 (2024) 105375. doi:10.1016/j.jdent.2024.105375.
- S.M. Juckes, B. Sullivan, I. Kostylev, R.B. Price, D. Labrie, Three-dimensional beam profiling used to characterize dental light-curing units, Appl Opt 58(35) (2019) 9540-9547. doi:10.1364/AO.58.009540.
- C. Maucoski, A.H. Balzer, A. Kudrek de Souza, S.S. Lourenço Braga, B. Sullivan, R.B. Price, C.A.G. Arrais, Influence of a budget single-peak light-curing unit on the microhardness and bond strength of bulk-fill resin composites to the gingival floor of proximal class II cavity preparations, International Journal of Adhesion and Adhesives 118 (2022) 103239. doi:10.1016/j.ijadhadh.2022.103239.
- C.J. Soares, S. Braga, R.B. Price, Relationship Between the Cost of 12 Light-curing Units and Their Radiant Power, Emission Spectrum, Radiant Exitance, and Beam Profile, Oper. Dent. 46(3) (2021) 283-292. doi:10.2341/19-274-L.
- C. Shimokawa, M.L. Turbino, M. Giannini, R.R. Braga, R.B. Price, Effect of Curing Light and Exposure Time on the Polymerization of Bulk-Fill Resin-Based Composites in Molar Teeth, Oper. Dent. 45(3) (2020) E141-E155. doi:10.2341/19-126-L.
- S. Oh, H.J. Kim, H.J. Kim, S.A. Antonson, S.Y. Kim, Influence of irradiation distance on the mechanical performances of resin composites polymerized with high-irradiance light curing units, Biomater Res 26(1) (2022) 18. doi:10.1186/s40824-022-00267-5.
- A. Osseiran, R.B. Price, K. Dunn, D. Tran, C. Maucoski, G. Kugel, Buyer Beware: Curing Lights, Dent. Econ. 02 (2022) 18-22.
- C.B. Andre, G. Nima, M. Sebold, M. Giannini, R.B. Price, Stability of the Light Output, Oral Cavity Tip Accessibility in Posterior Region and Emission Spectrum of Light-Curing Units, Oper. Dent. 43(4) (2018) 398-407. doi:10.2341/17-033-L.
- R.J. Moreira, R.A. de Deus, M.T.H. Ribeiro, S.S.L. Braga, A.C.T. Schettini, R.B. Price, C.J. Soares, Effect of Light-curing Unit Design and Mouth Opening on the Polymerization of Bulk-fill Resin-based Composite Restorations in Molars, J. Adhes. Dent. 23(2) (2021) 121-131. doi:10.3290/j.jad.b1079561.
- K.L. Konerding, M. Heyder, S. Kranz, A. Guellmar, A. Voelpel, D.C. Watts, K.D. Jandt, B.W. Sigusch, Study of energy transfer by different light curing units into a class III restoration as a function of tilt angle and distance, using a MARC Patient Simulator (PS), Dent. Mater. 32(5) (2016) 676-86. doi:10.1016/j.dental.2016.02.007.
- D.D. Kojic, O. El-Mowafy, O. Falenchuk, C.J. Felix, R.F. Mondelli, J.F. Bombonatti, Radiant-exposure attenuation through Class-2 proximal slots, Am. J. Dent. 34(2) (2021) 116-119.
- ANSES, Effets sur la santé humaine et sur l’environnement (faune et flore) des diodes électroluminescentes (LED), ANSES, 2019.
- A. Neitz, A. Rice, L. Casiraghi, I.L. Bussi, E.D. Buhr, M. Neitz, J. Neitz, H.O. de la Iglesia, J.A. Kuchenbecker, Toward an Indoor Lighting Solution for Social Jet Lag, J. Biol. Rhythms 39(5) (2024) 502-507. doi:10.1177/07487304241262918.
- A. Fietz, F. Corsi, J. Hurst, S. Schnichels, Blue Light Damage and p53: Unravelling the Role of p53 in Oxidative-Stress-Induced Retinal Apoptosis, Antioxidants (Basel) 12(12) (2023). doi:10.3390/antiox12122072.
- A.C.o.G.I.H. (ACGIH). TLVs and BEIs Based on the Documentation for Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices, ACGIH Cincinnati, Ohio (2023).
- A.R. Wielgus, J.E. Roberts, Retinal photodamage by endogenous and xenobiotic agents, Photochem. Photobiol. 88(6) (2012) 1320-45. doi:10.1111/j.1751-1097.2012.01174.x.
- D. Oliveira, M.G. Rocha, Dental Light-Curing-Assessing the Blue-Light Hazard, Dent. Clin. North Am. 66(4) (2022) 537-550. doi:10.1016/j.cden.2022.05.004.
- M.T. Fluent, J.L. Ferracane, J.G. Mace, A.R. Shah, R.B. Price, Shedding light on a potential hazard: Dental light-curing units, J. Am. Dent. Assoc. 150(12) (2019) 1051-1058. doi:10.1016/j.adaj.2019.08.012.
- [54] K.R. Kofford, C.W. Wakefield, M.E. Nunn, The effect of autoclaving and polishing techniques on energy transmission of light-curing tips, Quintessence Int. 29(8) (1998) 491-6.
- F.A. Rueggeberg, W.F. Caughman, R.W. Comer, The effect of autoclaving on energy transmission through light-curing tips, J. Am. Dent. Assoc. 127(8) (1996) 1183-7. doi:10.14219/jada.archive.1996.0409.
- C.J. Soares, S.S.L. Braga, M.T.H. Ribeiro, R.B. Price, Effect of infection control barriers on the light output from a multi-peak light curing unit, J. Dent. 103 (2020) 103503. doi:10.1016/j.jdent.2020.103503.
- R.A. Ajaj, H.M. Nassar, F.A. Hasanain, Infection Control Barrier and Curing Time as Factors Affecting the Irradiance of Light-Cure Units, J Int Soc Prev Community Dent 8(6) (2018) 523-528. doi:10.4103/jispcd.JISPCD_226_18.
- R.T. Khode, P.R. Shenoi, R.R. Kubde, C.S. Makade, K.D. Wadekar, P.T. Khode, Evaluation of effect of different disposable infection control barriers on light intensity of light-curing unit and microhardness of composite – An in vitro study, J Conserv Dent 20(3) (2017) 180-184. doi:10.4103/JCD.JCD_171_16.
- R.J. Sword, U.N. Do, J.H. Chang, F.A. Rueggeberg, Effect of Curing Light Barriers and Light Types on Radiant Exposure and Composite Conversion, J Esthet Restor Dent 28(1) (2016) 29-42. doi:10.1111/jerd.12173.
- A.C. Shortall, R.B. Price, L. MacKenzie, F.J. Burke, Guidelines for the selection, use, and maintenance of LED light-curing units – Part II, Br. Dent. J. 221(9) (2016) 551-554. doi:10.1038/sj.bdj.2016.814.
About the author

Dr. Price is a world-renowned authority on dental curing lights. With over 250 peer-reviewed publications, Dr. Price’s work on light curing technology has significantly improved patient outcomes worldwide.

Dr. Maucoski is a postdoctoral fellow at Dalhousie University (Canada) and is actively involved in studies evaluating various light curing units and their effect on dental materials and thermal changes.

Alex Gareau is a research assistant at Dalhousie University. He works in Dr. Price’s lab to study the properties of dental materials and light curing units.