INTRODUCTION
In the past few decades, dentistry and dental technology have advanced by leaps and bounds. These advances have been driven by improvements in computer processing power leading to advances in digital technology (CAD/CAM). The evolution in biomaterials has led to the development of zirconium oxide ZrO2 or, as it is most commonly referred to, zirconia. However, the communication between dentists and their dental technologists seems to be lagging. We can all do better!
Anyone who has visited a dental laboratory or had a frank discussion with a dental technologist would be able to see firsthand “the good, the bad and the ugly” of the doctor/technician relationship. It essentially boils down to trust that each party will listen to the other’s challenges and will work together to achieve a common goal. Working together as a team from the treatment planning stage, to interim restorations, to final insertion, can eliminate problems by considering both clinical and laboratory issues simultaneously. This will lead to a result that creates predictable success for the dentist and, most importantly, a satisfied patient. Essentially, effective communication results in a WIN, WIN, WIN: 1. a happy patient, 2. increased productivity for the clinician, 3. significant reduction in remakes and/or modifications for the laboratory.
The goal of this article is to discuss the main aspects of the communication process between the dentist and the laboratory. What is the most effective method of communication available to the dentist? How can the laboratory assist the dentist in the treatment planning and treatment execution phases? What are the responsibilities of the clinician to the patient and the laboratory? What are the responsibilities of the laboratory to the prescribing dentist?
METHODS OF COMMUNICATION
To effectively treat cases involving multiple teeth, altering the vertical dimension of occlusion, and/ or in highly sensitive aesthetic situations, involving the laboratory earlier on in the treatment planning phase will allow for a greater chance of a successful treatment outcome. (Fig. 1) Communication between the dentist and the patient is critical during the treatment planning phase of a large aesthetic case. The patient’s expectations may not match the dentist’s expectations. Furthermore, the patient may have specific ideas about how his or her smile should look. If the patient’s vision does not match the final result, he or she will most likely be disappointed followed by dissatisfied. To ensure this does not happen, it is important to plan effectively. This means taking time with your patient to make sure their vision is understood. It has been said that “the beauty is in the eye of the beholder”. As such, we are beholden to the patient to ensure they are satisfied. Asking the patient to bring in historical photos or photos of someone whose smile they want to mimic can be very insightful. Ask them about their shade preference during the consultation period and accurately capture it. (Fig. 2) The patient’s presenting condition should be captured as well, both for communications with the lab and medical-legal purposes. This includes necessary radiographs, accurate impressions (either analogue or digitally captured) to produce models, stable interocclusal records at the correct vertical/horizontal position for accurate articulation, facebow records when required, as well as representative digital photos to convey both dental and facial parameters. (Fig. 3) With this information in hand, the savvy clinician should consult with their laboratory technician to discuss the occlusal scheme, biomaterial selection, overall size, shape, shade, and contours of the teeth, to start developing a plan that will achieve the patient’s aesthetic goals while, at the same time, allowing for the predictable outcome in practice. (Fig. 4)
Fig. 1

Fig. 2

Fig. 3

Fig. 4

Working as a team member, the laboratory can assist in several ways. First, the material selection process is a service that a laboratory can provide. Often, the difference between success and failure with biomaterial technologies is their proper selection for the case circumstances. The dental laboratory is uniquely positioned to experience success or failure with the myriad of dental restorative materials and their use in particular cases. The laboratory technician is able to offer valuable input as to the material properties and their intraoral applications, limitations, and techniques for success. The goal in selecting the most appropriate biomaterial is to optimize the balance between the aesthetic quality of the restoration, and its long-term clinical performance
and predictability. Simply put, we want the result to be aesthetic enough to satisfy the patient, and strong enough to last.
Second, the best way to communicate with the technician is to allow him/her to see what you see. If you have an in-office laboratory, then the lab technician should have an opportunity to interview the patient at the consult appointment. However, in most cases the lab is off site. As a result, good photographic documentation is crucial. In addition, it would be incredibly valuable to record and share a video of the patient speaking and going through multiple continuous chewing strokes to observe them “in function”. Allow the patient to describe their vision in their own words and allow the lab technician the opportunity to “meet” the patient virtually, so the casts being worked on will come to life. Armed with this information, a laboratory-fabricated diagnostic wax-ups can be created. (Fig. 5) A “wax up” is an excellent tool for the treatment planning phase. They can demonstrate for the dentist and the patient what the laboratory can accomplish
with specific restorative materials. Many contours can be created in wax, but the specific dimensions required for a given material are an important consideration. Third, the choice of the restorative material combined with the wax-up can guide the dentist in the amount of preparation required to duplicate the result created in wax. Once the dentist, lab technician and patient are happy, the diagnostic wax up can be approved. Now the reparation/ reduction guides can be fabricated, as well as matrices or provisional shells for making interim restorations.
Fig. 5

A highly aesthetic outcome satisfactory to the patient is dependent on communicating color (chroma, hue, and value), translucency, and surface texture. The underlying challenge for the clinician is to determine all these parameters accurately and then to successfully communicate the details and expectations for the patient case. The challenge for the lab team is to understand exactly what the dentist is asking for and to successfully implement the information received into the restorative product. In order to facilitate communication, the dentist will provide the lab technician with a written prescription describing what is expected. Of course, the detailed prescription needs to be accompanied by impressions, diagnostic casts, a bite registration, face-bow records, and clinical photos.
WHAT IS EXPECTED OF THE DENTIST?
- A well written prescription describing the patients name, age, sex and mastication habits and the type of restoration needed (fixed or removable).
- The clinician should provide accurate final and opposing arch impression either analogue or digital (Fig. 6) that duplicate the intraoral tooth preparations. (Fig. 7) Analog impressions should be free of bubbles, margins visible and taken on a stable impression tray. All outgoing materials should be disinfected according to current infection control standards, placed in an appropriate container, packed properly to prevent damage, and transported.
- Accurate bite registrations are a MUST using a more rigid material to aid with proper articulation.
- Digital photographs are important and necessary to create a precise dental prosthesis. A proper shade guide that is identical to the one being used by the dental laboratory is needed including the stump shade for the anterior region. Chairside custom shading or sending the patient to the dental lab is recommended for anterior restorations.
- In restoring implants, it is important to mention the type of implant being used, how long the patient will be in temporaries, will the final prosthesis be screw or cement retained.
- An X-ray which shows the placement of the implant is extremely important for a dental technologist. A stone model does not provide adequate information regarding bone level, a radiograph of the patient allows for the proper selection of the correct prefabricated abutment or to customize one to achieve a successful final restoration.
Fig. 6
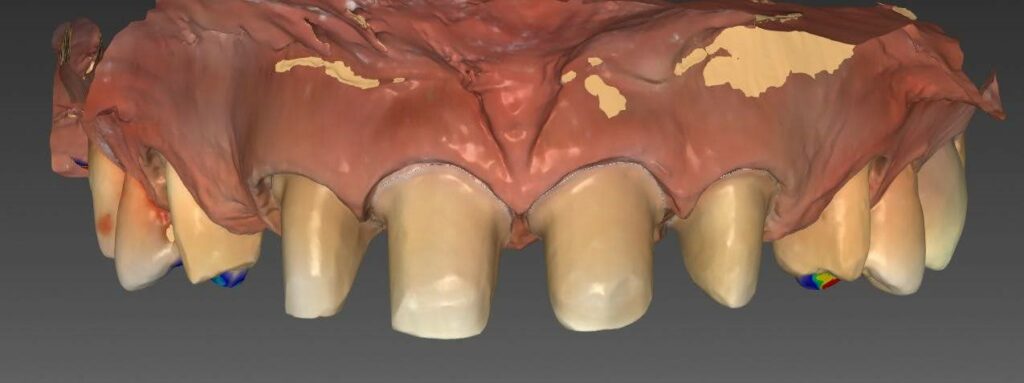
Fig. 7

WHAT IS EXPECTED OF THE LAB TECHNICIAN?
- The laboratory technician should custom manufacture dental prostheses/appliances which follow the written instructions provided by the dentist and should fit properly on the casts and mounting.
- The laboratory should return the case to the dentist to verify the mounting if there is any question regarding the accuracy of the bite registration provided by the dentist.
- The laboratory/technician should match the shade which was described in the original written instructions.
- After acceptance of the written instructions, the laboratory/technician should custom manufacture and return the prostheses/appliances in a timely manner.
- The laboratory should follow current infection control standards with respect to the personal protective equipment and disinfection of prostheses/appliances and materials. All materials should be checked for breakage and immediately reported, if found.
- The laboratory/technician should inform the dentist of the materials used to prepare the case and suggest methods how to properly handle and adjust these materials.
- The laboratory/technician should clean and disinfect all incoming and outgoing items from the dentist’s office (impressions, occlusal registrations, prostheses, etc.) according to current infection control standards, placed in an appropriate container, packed to prevent damage, and transported.
At the end of the day, the dentist has the overall responsibility for the treatment rendered. The laboratory will produce the prosthetic restorations for a try-in (Fig. 8) but whether or not to finalize the case, (Fig. 9) is the clinician’s decision. Delegating many procedures to auxiliary team members is possible if all the necessary information is provided to enable them to deliver high-quality service. When working with a laboratory, however, errors such as insufficient tooth reduction, ambiguous margins, unstable interocclusal records and articulations, and poor communication of the desired shades for aesthetic restorations to the technician will lead to unhappy patients, unproductive practices and lab technician who feels defeated. Good communication coupled with good clinical and technical skills is the winning formula for success. (Fig. 10) We can all strive to do better.
Fig. 8

Fig. 9

Fig. 10

Oral Health welcomes this original article
About the Authors
 Joseph Fava earned his DDS, MSc and prosthodontic specialty certificate at the University of Toronto. He is a clinical instructor in the Graduate Prosthodontic Program at U of T and co-director of U of T’s Implant Residency Program. Dr. Fava is clinical director of Yorkville Village Dentistry and Forest Hill Prosthodontics where he maintains a specialty prosthodontics practice.
Joseph Fava earned his DDS, MSc and prosthodontic specialty certificate at the University of Toronto. He is a clinical instructor in the Graduate Prosthodontic Program at U of T and co-director of U of T’s Implant Residency Program. Dr. Fava is clinical director of Yorkville Village Dentistry and Forest Hill Prosthodontics where he maintains a specialty prosthodontics practice.
 Karim Sahil acquired his Dental Technology certificate at George Brown College as a Registered Dental Technologist. He earned his Master Dental Technologist certificate from New York on the study of mandibular physiology, occlusion and full mouth reconstruction. He maintains an in-house dental laboratory at Yorkville Village Dentistry
Karim Sahil acquired his Dental Technology certificate at George Brown College as a Registered Dental Technologist. He earned his Master Dental Technologist certificate from New York on the study of mandibular physiology, occlusion and full mouth reconstruction. He maintains an in-house dental laboratory at Yorkville Village Dentistry












