Abstract
Collagen repair and regeneration is a continual process. With chronic inflammation, however, collagen and tissue repair are compromised. Not only is the periodontium severely impacted, but systemic health is placed at risk. What causes excessive collagen breakdown and how does this impact oral health? Collagen supplementation (with questionable science) has become a fast-growing trend, particularly targeted at the structural and esthetic decline of our aging population. What is the evidence-based science behind recommendations to minimize the breakdown of collagen? What are the current clinical guidelines?
What exactly is collagen?
Collagen is the major insoluble fibrous protein in the extracellular matrix and in connective tissue. In fact, it is the single most abundant protein in the animal kingdom”1 comprising one-third of the total protein in the human body. There are twenty-eight different types of collagen found in the human body. The vast majority (80-90%) are types I, II and III. Type I collagen may be found in skin, tendons, bones, ligaments, dentin, and interstitial tissues. Type II is found in cartilage and vitreous humor (which fills the space between the lens and retina of the eye). Type III collagen is found in skin, muscle and blood vessels. Collagen is very rigid and resistant to stretching, making it the perfect matrix for skin, tendons, bones, and ligaments. It accounts for three-quarters of the dry weight of our skin.2 Being an essential protein in the human body and having multiple health benefits and functions, collagen significantly impacts systemic health.
The Collagen Trend
Collagen supplementation has become a fast-growing trend, targeting the health and esthetic concerns of the aging population – all with uncertain scientific evidence. It has been named one of the ‘top food [and beverage] trends for 2019’ and expected to reach 7.5 billion dollars in sales on the global market by 2027.3 (Fig. 1) The escalating increase in demand is attributed to esthetic procedures, cosmetic surgeries, and its role in wound healing treatments. Cosmetic surgery and wound healing emerged as the largest healthcare segment of collagen supplementation in 2019, based on the ability of hydrolyzed collagen to treat chronic wounds, through its inhibition of metalloproteinase, an enzyme specifically implicated in collagen destruction.3
Fig. 1

With aging, the loss of collagen results in the skin losing its firmness and elasticity. Despite small sample size studies and biased funding, collagen is perceived by many as a ‘fountain of youth’. “There’s very little evidence-based medicine to show that collagen is effective as an anti-aging treatment,” says Lisa Kellett, a Toronto dermatologist.4 The science is scant on how digested collagen is channeled along the correct metabolic pathway to positively impact the skin’s integrity.
There is a quest to produce the ‘perfect’ supplement. Supplement types include powder, broth, gelatin, with the latest trend being collagen water. The manufacturing sources for collagen are varied and include bovine, porcine, poultry and marine origins. 35% of the market share is from bovine sources supported by good availability and desirable price point. Marine sources are considered superior to bovine or porcine due to bioavailability and absorption rate.
Collagen production is supported by a well-balanced diet rich in Vitamin C along with other foods containing zinc (seafood, meats, beans, legumes) and copper (lamb, oysters and almonds) coupled with ample dietary protein. This simple dietary approach under normal circumstances should suffice in maintaining the balance between collagen loss and regeneration.4
What happens at the cellular level when the body is not producing collagen at the same turnover rate as it is being destroyed? Are we capable of addressing the root cause with supplementation? In the human body, the process of collagen synthesis occurs mainly within fibroblast cells. The biochemical pathway is carefully regulated and controlled. As with any process, there can be various mutations, modifications or deficiencies which may adversely affect the ongoing synthesis of collagen.5 Collagen repair and regeneration is continual, but chronic inflammation has a significant negative impact on its progress.
Role of Collagen in the Periodontium and Systemic Health
Without collagen, there would be no periodontium; plain and simple. The periodontium is made up of and supported primarily by collagen. The gingival tissues are comprised of 60% collagen, the periodontal ligament is 70-80% collagen and the alveolar bone matrix is 90% collagen.
The health and subsequent repair and renewal of the periodontium and supporting structures of the body is strongly contingent on the capability of collagen regeneration. The important biomechanical role of collagen in the body is seriously compromised when collagen is diminished or ‘damaged’. Chronic inflammatory conditions may alter the connective tissue matrix leading to its functional impairment.6 The deterioration of collagen in the presence of chronic inflammation is due to the excessive accumulation and release of matrix degrading enzymes or metalloproteinases (MMPs) that directly attack collagen integrity. The primary function of MMP-8 is the degradation of type I, II and III collagens. Not only is the periodontium severely impacted, but systemic health is placed at risk.
Guidelines for Clinical Practice
As the collagen trend continues to boom, the biggest question looming is what is the cause or etiologic pathway that impacts collagen loss? What we do know is that continuing to ignore the inflammatory component of periodontal disease and treating it as a bacterial infection only, is placing our periodontal patients at ongoing risk for systemic disease. In fact, the American Association of Periodontology (AAP) has redefined periodontal disease as an inflammatory disease capable of far reaching systemic implications. “Research has shown that periodontal disease is associated with several other diseases. For a long time, it was thought that bacteria were the factor that linked periodontal disease to other disease in the body; however, more recent research demonstrates that inflammation may be responsible for the association. Therefore, treating inflammation may not only help manage periodontal diseases but may also help with the management of other chronic inflammatory conditions.”7,8 The most current JADA (Journal of the American Dental Association) guidelines for treatment of chronic periodontitis are reflective of this same principal.9
Current research directs us to address the host-response mechanisms as the mediators of the destruction of the collagen-rich periodontium. Over three decades ago a novel discovery identified the ‘host-modulating’ capabilities of a sub-antimicrobial dose of doxycycline to directly inhibit the excessive production of matrix metalloproteinases in connective tissues in the presence of chronic inflammation.
Historically we have treated periodontitis using a mechanical or surgical approach versus a pharmaceutical approach.10 “Bacteria initiate periodontitis. They are essential but they are insufficient. What is required is a susceptible host.”11 Today’s periodontal therapy program employs a 3-pronged approach:
- Assessment and management of risk factors
- Management of dental biofilm
- Management of host response and inflammation
The current JADA guidelines support the clinical use of a non-antibiotic formulation of low-dose doxycycline as a favoured adjunct to scaling and root planing.12 Addressing host response is a ‘must’ or our treatment outcomes will be at a standstill.
Low dose doxycycline (LDD) will reduce the over-production of collagenase (MMP-8, MMP-9, enzymes responsible for the accelerated breakdown and destruction of collagen) and osteoclasts (bone cells responsible for the resorption of bone) that are present in overabundance during a chronic, prolonged and destructive inflammatory response. C-reactive protein (CRP-a biomarker for elevated inflammation) levels have also been reduced with low-dose doxycycline.
Systemically, this exaggerated inflammatory response is common among inflammatory diseases such as periodontitis, cardiovascular disease and rheumatoid arthritis.
Periostat (low-dose doxycycline), when used BID for 3 to 9 months, will help modulate the chronic, prolonged and destructive inflammatory response into a normal and healthy inflammatory response. (Fig. 2)
Fig. 2

Future Directions
Low-dose doxycycline also showed efficacy in patients with systemic diseases relevant to periodontitis, including diabetes mellitus and arthritis, and in postmenopausal women with local and systemic bone loss. Importantly, long-term administration of LDD or sub-antimicrobial dose doxycycline (SDD) of up to 2 years in clinical trials, did not produce antibiotic side-effects. “SDD (and in the future, new host modulating therapeutics, such as low-dose CMT-3 (chemically modified tetracyclines), resolvins and chemically modified curcumins may shift the paradigm of periodontal therapy from a predominantly surgical approach to the greater use of medicinal/pharmacologic strategies, ultimately to benefit larger numbers of patients.”13
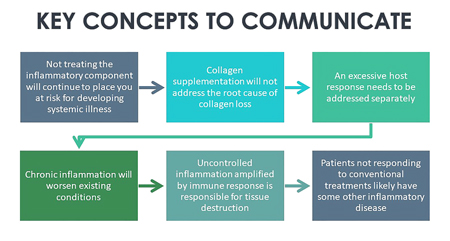
With strong science supporting the influence of the host response as the ‘driver’ of tissue breakdown in the pathogenesis of periodontitis, we have a strong responsibility to integrate host modulation into our periodontal treatment planning. Research is focusing on the exploration of using this principle to address other inflammatory/collagenolytic responses in the body.14 As dental professionals, we must also communicate key concepts to educate our patients as to the benefits of these therapies on oral health, their potential to mitigate the risk of systemic disease, and to ultimately help maintain overall wellness. (Table 1)
Table 1
Oral Health welcomes this original article.
Disclaimer: The author does not endorse or dissuade the use of collagen supplementation. The article is written with the intent of clarifying the role of collagen in the periodontium, examining the root cause of excessive tissue loss and published clinical guidelines. The author has received no financial compensation for the writing of this article.
References
- Lodish H, Berk A, Zipursky SL, et al. Molecular Cell Biology. 4th edition. New York: W. H. Freeman; 2000. Section 22.3, Collagen: The Fibrous Proteins of the Matrix.
- Shoulders, M. D., & Raines, R. T. (2009). Collagen structure and stability. Annual review of biochemistry, 78, 929–958.
- https://www.grandviewresearch.com/press-release/global-collagen-market
- https://dlkonavenue.com/edible-collagen/
- Wu M, Cronin K, Crane JS. Biochemistry, Collagen Synthesis. [Updated 2020 May 4]. In: StatPearls Publishing; 2020 Jan.
- Narayanan AS, Engel LD, Page RC. The effect of chronic inflammation on the composition of collagen types in human connective tissue. Coll Relat Res. 1983;3(4):323-334. https://pubmed.ncbi.nlm.nih.gov/6413124/
- https://www.perio.org/consumer/gum-disease-and-other-diseases
- Donley T, Golub LM, Jones JD, et al. Addressing the inflammatory response in periodontal and related systemic disease. Oral Health Periodontics Fall 2015.
- Smiley CJ, Tracy SL, Abt E, et al. Systematic review and meta-analysis on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. JADA 2015; 146(7):508-524.
- https://pubmed.ncbi.nlm.nih.gov/27009489/
- Goldstep F. Periodontal Inflammation: Simplified. December 2013. Oral Health Journal. 103(12);8-17.
- Smiley CJ, Tracy SL, Abt E, et al. Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. JADA 2015;146(7):525-535.
- Golub LM, Elburki MS, Walker C, Ryan M, et al. Non-antibacterial tetracycline formulations: host-modulators in the treatment of periodontitis and relevant systemic diseases. International Dental Journal 2016; 66: 127-135. https://pubmed.ncbi.nlm.nih.gov/21357860/
- Golub LM, Lee HM. Periodontal therapeutics: Current host-modulation agents and future directions. Periodontol 2000. 2020;82(1):186-204. https://pubmed.ncbi.nlm.nih.gov/31850625/
About the Author
 Jo-Anne Jones is an international speaker, president of a clinical and educational training company and continues to maintain active registration as a dental hygienist. She joins the Dentistry Today CE Leaders in 2020 for the 10th consecutive year. Jo-Anne has received the Elizabeth Craig Award of Distinction for her contribution to the profession of dental hygiene. To contact Jo-Anne, email at jjones@jo-annejones.com
Jo-Anne Jones is an international speaker, president of a clinical and educational training company and continues to maintain active registration as a dental hygienist. She joins the Dentistry Today CE Leaders in 2020 for the 10th consecutive year. Jo-Anne has received the Elizabeth Craig Award of Distinction for her contribution to the profession of dental hygiene. To contact Jo-Anne, email at jjones@jo-annejones.com












