
The purpose of endodontics is to prevent or heal lesions of endodontic origin (LEO).1 If preventing and healing is the purpose of endodontics, how do we increase endodontic predictability in order to accomplish the preferred result?
The first step to successful endodontics is to decide if what I am doing is predictable. As a clinician and educator for more than 35 years, it is always interesting to hear what the most frequent questions are asked by students and dentists. The most frequent question is, “How do you fill all those root canal system foramina?” In fact, obturated foramina or endodontic portals of exit (POEs) have been the benchmark of exceptional endodontics. The second most frequent question posed by students is, “Are all those POEs important?” The answer is that sometimes they are important, and sometimes they are not. The situation is, however, that we do not know over time, which POEs are important, and which are not. There are factors that influence LEO prevention and cure that we may not be able to control such as biology: host resistance, degree of root canal system bacterial invasion, presence or absence of periradicular LEO, vital versus infected or necrotic pulp, and time. However, there are factors that we as dentists can control or, at least, significantly influence such as endodontic mechanics: thoroughness of root canal system cleaning, proper radicular canal shaping in order to facilitate 3-dimensional obturation, quality of obturation technique, and quality of coronal seal.
What Matters?
Given the seeming multitude of predictability factors, however, what really matters? In my career, it has boiled down to the most fundamental process of disease healing: if we remove a disease, symptom removal also predictably follows. They vanish. There are no human disease symptoms that are sustained without their cause. Endodontic disease is no different. The rationale for endodontic success is really the rationale for all disease. Just eliminate the disease and predictable healing follows. Specifically, in endodontics, “The rationale for endodontics is that any endodontically diseased treatment can be predictably successful if the root canal system can be nonsurgically or surgically sealed and is periodontally healthy or can be made healthy.” What matters is in the details of the proper knowledge of what to do, the skills to do it, and the willingness to know and do. Operating from this tenant changes 3 things:
- Who’s in control? There becomes a tenant of “accountability.” Endodontic predictability becomes a measure of how successful the dentist is in shaping, cleaning, and obturating the root canal system. Excuses such as “some lesions just don’t heal,” or “the lesion is too big,” or “the lesion is infected or a cyst” are no longer valid. Unlike most restorative dentistry, the quality of the lab’s results or the quality of personal oral hygiene are less significant in endodontic healing. The big variables are the clinician and the anatomy. As an endodontist, it is the best game in town. It is the dental discipline where I can affect the greatest control with the exception, perhaps, of extraction. Herein lies the good news and bad news. The good news is the dentist is responsible for the outcome. The bad news is the dentist is responsible for the outcome. The good news and the bad news are the same. To me, however, this is a terrific responsibility and cannot be delegated. To sit at chairside during the endodontic portion of your day and know that you are in control is priceless.
- What does it mean for me to be in control? It means that the details matter. Control means being in control of the details.2-7 It means details matter as prerequisite to endodontic predictability. It has been said that “the devil’s in the details.” What does this mean, and does this thought process apply to endodontics? It is a shift from “what can I get away with?” to “what can I get?” It means all root canal systems and their POEs have potential significance. It means that size and location do not matter; both are part of unraveling the formula for predictable endodontic success.
- How do you get in control? Many students and dentists ask me how to be efficient. What they really want to know is how to do endo faster. They want to know how to speed up? I teach them the way you speed up in endodontics is to slow down. When we slow down in endodontics, we actually do speed up because we avoid costly mechanical errors such as blocks, ledges, and foraminal transportations, either internal or external.
CASE EXAMPLES: WHEN DETAILS OF ANATOMY MATTERED
Endodontic Predictability: Detail Example No. 1
This example of a mandibular first molar LEO graphically details endodontic anatomy that we know matters in endodontic predictability but which exact details that mattered are not known. This patient presented 34 years ago at a time before endodontic microscopes, before rotary shaping, and before digital imaging. And yet technologies and techniques were available to eliminate POE often regardless of how they got there and regardless of their size or location. The pretreatment image demonstrates triangular furcal radiolucency (Fig. 1a). Periodontal probing was precipitous, although buccal mesial distal width of sinus tract was 3 mm. The root canal system was cleaned and shaped into a funnel form preparation using hand files, hand reamers, and Gates Glidden drills. Anatomy was obturated using vertical compaction of warm gutta-percha technique. Note obturation of distal resorptive defect, furcal canal (arrow), a mesial lateral canal, 2 distal foramina, and one mesial apical foramen (Fig. 1b). In total, the posttreatment and oblique radiographs (Fig. 1c) indicate 3 canals and 6 POEs sealed. Fig. 1d is 34 years posttreatment, revealing healed radiographic lamina dura and periodontal ligament. Tissue probes within normal limits and the patient is asymptomatic. Which POE mattered and which one or ones did not matter? To me, it does not matter. What matters are the significant potential details of sealed POEs, regardless of location or cause is cause in the matter. Long-term success validates that attention to detail matters in endodontic predictability.
Fig. 1A

Fig. 1B
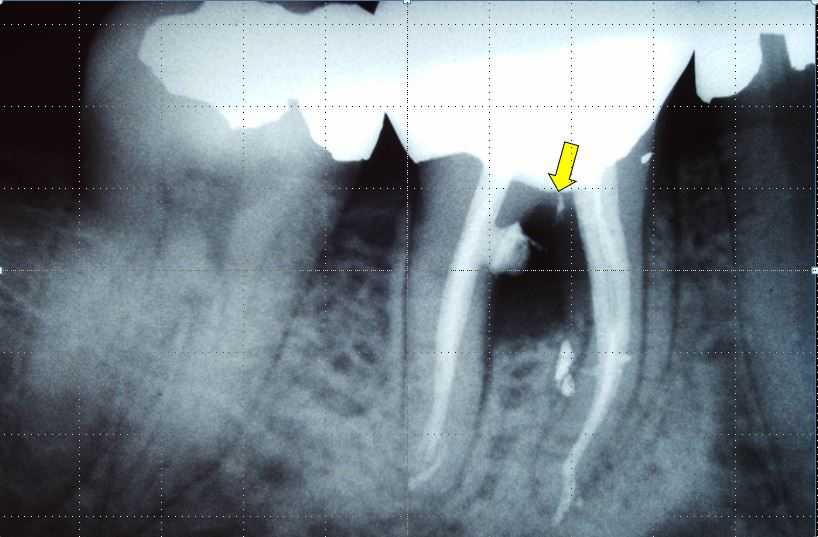
Fig. 1C

Fig. 1D

Endodontic Predictability: Detail Example No. 2
Example No. 1 demonstrates a “natural” furcal LEO due to root canal system necrosis and gangrene. Example No. 2, however, presents with iatrogenic furcal and apical lesions of endodontic origin. Example No. 2 has the same resulting disease as example No. 1 but different origins requiring endodontic retreatment. Interproximal furcal repair requiring a fairly invasive surgery was considered, but the choice on nonsurgical endodontic retreatment to produce the endodontic seal had a higher mechanical, biologic, structural, and aesthetic predictability. The patient presented with buccal swelling and radiographic furcal and apical lesions of endodontic origin (Fig.2a). On access, the chamber hemorrhaged significantly and only slowed after sodium irrigation and placement of epinephrine pellet and pressure (Fig.2b). Once bleeding was under control, MTA was trolled along mesial wall of distal canal strip perforation using small West spatula (Gary Carr). A modified bite-wing was used to measure accurate geography of radiographic perforation (Fig. 2c). Fig. 2d is the final periapical radiograph of finished MTA mesial wall furcal repair of the distal root. Two-year posttreatment validates furcal and apical healing after furcal healing and nonsurgical repair of the entire root canal system (plus the tooth has been successfully restored) (Fig. 2e). Fig. 2f to 2h confirm healthy periodontal probing from mesial distal location of original wide precipitous endodontic sinus tract. Tissue blanching indicates appropriate apical pressure used to challenge attachment apparatus.
Fig. 2A

Fig. 2B

Fig. 2C

Fig. 2D

Fig. 2E

Fig. 2F

Fig. 2G

Fig. 2H

Endodontic Predictability: Detail Example No. 3
Examples No. 1 and No. 2 are multirooted teeth with furcal disease caused by undersealed POEs. Example No. 3 shows endodontic predictably details that can occur anywhere along the coast-to-coast surface of the root itself. This detail can present in the form of an under-filled naturally occurring POE or due to a perforation from radicular preparation or, in this case, lateral root resorption. A pretreatment radiograph of maxillary left central incisor shows possible distal midroot radiolucency (Fig. 3a). A facial sinus tract distal to tooth No. 8 was observed and then traced with a gutta-percha cone (Fig. 3b). A periapical radiograph was taken to identify the mid distal root sinus tract source (Fig. 3c). Due to the patient’s high smile-line and delicate gingival tissues, a full surgical flap was avoided. An incision in the attached gingiva may have restricted access to midroot resorptive disease, and so the highest endodontic predictability to create the endodontic seal was considered the nonsurgical endodontic retreatment approach. Fig. 3d was taken after the previous gutta-percha was removed using heat and solvents. After proper shaping, a new gutta-percha conefit was made (Fig. 3e). The root canal system was then obturated using the multiwave vertical compaction of warm gutta-percha technique (Fig. 3f). The sinus tract readily closed (Fig. 3g) and 5-year posttreatment image shows healed radiographic attachment apparatus, restored crown, and asymptomatic patient (Fig. 3h).
Fig. 3A

Fig. 3B
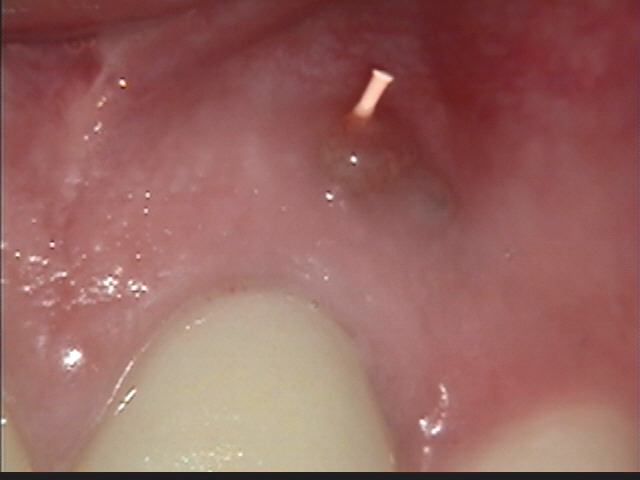
Fig. 3C

Fig. 3D

Fig. 3E

Fig. 3F

Fig. 3G

Fig. 3H

Endodontic Predictability: Detail Example No. 4
Endodontic predictability details can be seemingly insignificant. However, many endodontic clinicians have encountered endodontics that failed to heal due to even underfilled lateral canals branching off of lateral canals! This patient’s failure to heal maxillary left anterior is an example of the fact that even the smallest details can be the difference between success and failure. The pretreatment image suggests LEO is concentrated apically (Fig. 4a). A gutta-percha cone is traced apically (Fig. 4b). While preserving the ferrule, an access was designed that would allow for sufficient obturation hydraulics to seal the root canal system. Vertical compaction of a warm gutta-percha was obturation system and posttreatment image revealed both a wide and extremely narrow apical POEs (Fig. 4c). The lateral canal off lateral canal phenomenon has been shown to be present in ToothAtlas (Fig. 4d). A closeup of the actual posttreatment pack image demonstrates similar lateral canals pressed against root in 6-year posttreatment image (Fig. 4e). posttreatment clinical confirms healing of sinus tract (Fig. 4f).
Fig. 4A

Fig. 4B

Fig. 4C

Fig. 4D
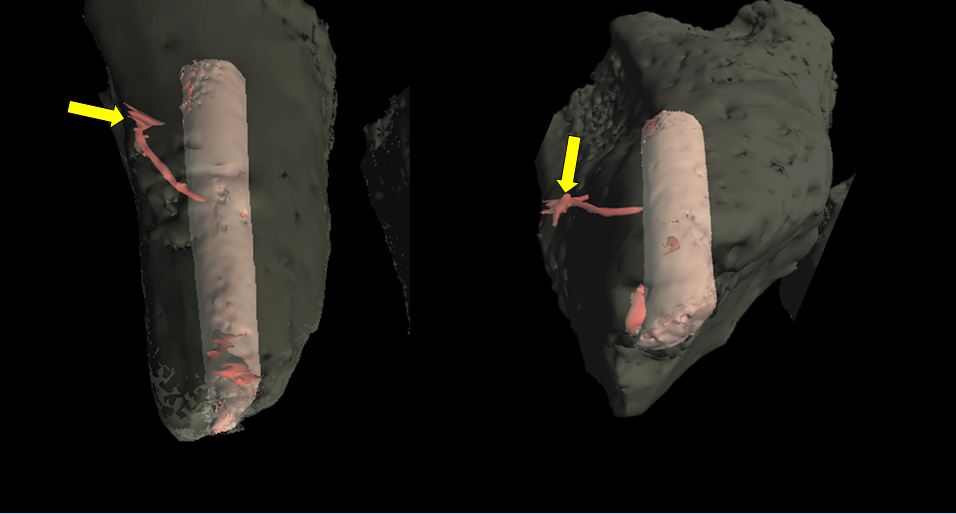
Fig. 4E
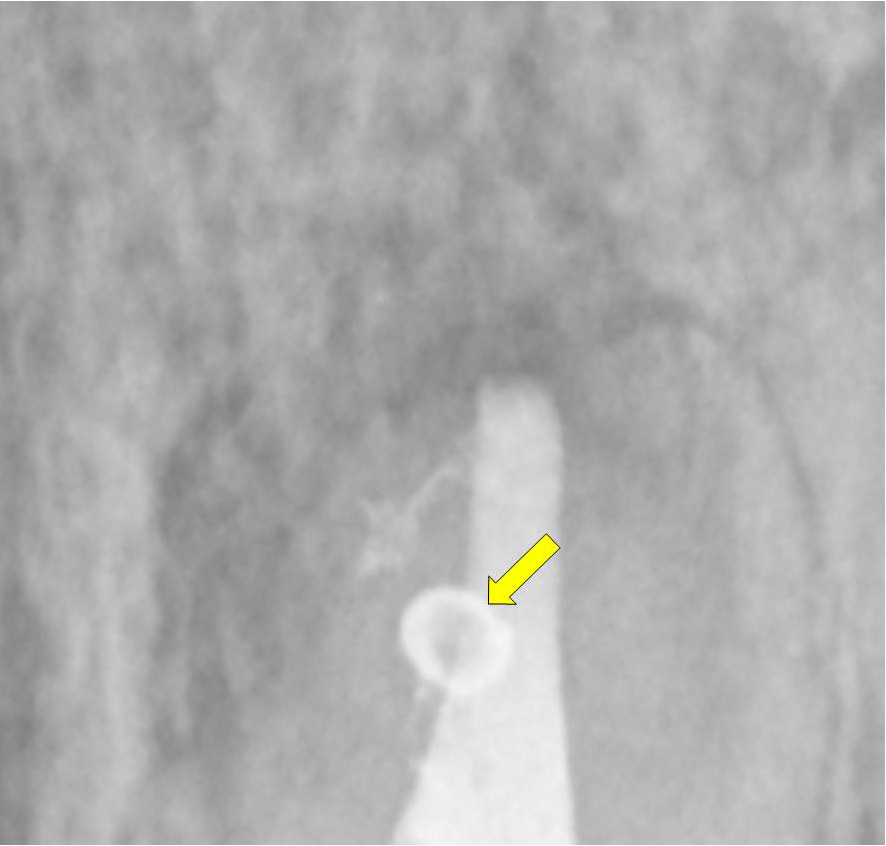
Fig. 4F

A TAKE HOME MESSAGE
Next time you are introduced to the “latest and greatest” endodontic tool, don’t ask, “How much faster can I do endo?” Ask, instead, “How much better can I do endo?” When you do it better, it becomes easier; and when you do it your best, and it is therefore easier, it can actually become fun. If you are having fun, you are doing endo right; and when you are doing endo right, the predictability will always follow. As dentists, predictability should be our No. 1 goal for our patient and for us. What matters? The secret is in the details. The secret to predictability is to learn skill sets that fulfill the rationale for endodontics. When we perform at our best, we are valued at our best. Society has a positive way of rewarding excellence: you will enjoy a dream practice that truly represents you, your skills, your mandate, and your purpose. Do it right!
This attitudinal shift changes everything in our endodontic purpose. Suddenly, we become as interested in the process and the product. Every mechanical move in the endodontic treatment takes on a new meaning. Performing exceptional endodontics requires being nimble, delicate, graceful, and patient. For some of us, this is not a natural skill. It must be practiced and developed. But the change and the learning curve always begins with awareness. Obturating all portals of exit requires restraint and intention together. This double and seemingly opposite simultaneous master skill set requires instruction, practice, surrender, intentionality, and being on the edge.8
Remember, endodontic predictability is in the details..
“Trifles make perfection, but perfection is no trifle.” –MichelangeloF
Disclosure: Dr. West is the coinventor of ProTaper and Wave One NiTi Systems and Calamus Obturation Systems (DENTSPLY Caulk)
Acknowledgement: *Originally published in Dentistry Today, Vol. 32, No. 9, pp. 108-113.
References
- West JD, Chivian N, Arens D, et al. Esthetic management of endodontically treated teeth. In: Goldstein RE, ed. Esthetics in Dentistry. 3rd ed. Shelton, CT: PMPH-USA; 2013:00-00. In press.
- West J. Anatomy matters. Endodontic Practice US. 2012;5:14-16.
- West J. Anatomy matters—part 2. Endodontic Practice US. 2012;5:26-27.
- West J. Anatomy matters—part 3. Furcal endodontic seal heals furcal lesion of endodontic origin. Endodontic Practice US. 2012;5:22-24.
- West J. Anatomy matters. Long-term case report. Endodontic Practice US. 2013;6:50-51.
- West J. Anatomy matters. Root canal system anatomy only matters when it matters. Endodontic Practice US. 2013;6:56-58.
- West J. Anatomy matters. Do lateral canals really matter? Part 6. Endodontic Practice US. 2013;6:52-53.
- Leonard G. Mastery: The Keys to Success and Long-Term Fulfillment. New York, NY: Plume; 1992.
About the Author

Dr. John West received his DDS degree from the University of Washington, where he is an affiliate professor, and his MSD degree in endodontics from Boston University, where he was honoured with the Distinguished Alumni Award. Dr. West is the founder and director of the Center for Endodontics in Tacoma, Wash, where he is also in private endodontic practice. He can be reached at (253) 377-2007 or via email at johnwest@centerforendodontics.com.










