As dentists, we all understand that good teeth and a beautiful smile are more than just symbols of health and success. The direct and indirect relationships between oral health and general health have been extensively investigated. There is now compelling evidence that a full and functional dentition is closely linked to multiple quality of life dimensions including physical health, psycho-social health and emotional well-being.1 We are slowly becoming aware of how integrated the oral cavity microbiology and biochemistry are with systemic health. However, we (healthcare providers with good teeth) take for granted the benefits of a fully dentate mouth. It has been shown that an individual’s perceived inability to smile or laugh due to ‘bad’ or missing teeth is a strong predictor of clinical depression.2 Measures of diet and nutritional sufficiency are also directly tied to the number of functional teeth an individual has. As would be expected the ability to chew dictates dietary choices which positively correlate with BMI (body mass index), nutrient levels and ultimately an individual’s longevity.3,4,5 The time honoured treatment of edentulism with full or removable partial dentures may not actually improve quality of life in older adults.6 When considering the significance of all these relationships, particularly in circumstances where the retention of the natural dentition is no longer a viable option, implant supported fixed prosthetic rehabilitation takes on an extremely important role.
Replacement of missing teeth with ‘implants’ has been attempted for thousands of years. Archeologic evidence from China dating back to 4000BC reveals the use of bamboo pegs as dental replacements in tooth sockets.7,8 However, it was not until 1965 that Per-Ingvar Branemark placed the first modern titanium endosteal dental implant in a patient.9 Despite their unequalled potential for treating the failing dentition, osseointegrated implants have not been a panacea. Long-term success has been shown to be dependent on not only the engineering of the dental implant but also on technique. ‘Success’ is more than just having an implant integrate. Contemporary implantology is unequivocally prostheticallly driven. The widespread placement of dental implants by dental providers has clearly shown that treatment success is directly related to operator experience and an in-depth understanding of how a final restoration must be designed and ultimately function. Furthermore, multiple implants supporting multi-unit prosthesis which are placed by clinicians that do not have the advantages of ‘real-time’ prosthodontic and laboratory support may have excellent implant integration yet have poor long-term survival and early prosthetic failure.10-13
The progression from single tooth replacement to multiple-unit or full arch reconstruction has demonstrated a need for innovative approaches. Many practitioners still consider multi-unit implant supported prostheses as a simple extension of a single unit replacement. Although superficially similar, multi-unit implant supported prostheses are fundamentally different and defined by a unique set of protocols.
Over the past 25 years, the concept of replacing an entire failing dentition with immediately loaded implant supported fixed hybrid prostheses has been gaining wide clinical acceptance. Supporting a full arch fixed prosthesis on as few as four implants was introduced by Branemark in 1977.14 By the early 1990’s the technique became known as ‘All on 4®’, which included tilting implants and immediate loading them with an all acrylic hybrid transitional full arch prosthesis.15,16 The clinical advantages of this approach became immediately apparent. Patients with a significantly failing dentition could have their remaining teeth removed and replaced with a fixed prosthesis in one appointment. Long-term data shows excellent success (99.2%) despite individual implant survival being only 95% to 97%.17 Patient acceptance and satisfaction are high, as conversion to a full and functional dentition is immediate, which positively impacts quality of life. Conventional alternatives such as piecemeal extraction combined with extensive periodontal, endodontic and prosthetic rehabilitation are still routinely provided by many clinicians. However, the long-term cost in terms of time commitment, financial burden and unreliability are often greater than immediate full arch or full mouth rehabilitation with implants and fixed immediately loaded prostheses. All-on-4® became a registered trademark of NobelBiocare but since then other implant companies such as Straumann introduced Pro Arch which supports a similar concept in terms of technique and components.
Rehabilitating a complete arch is by necessity a well-choreographed and resource intensive process. Long-term success and patient satisfaction depend on careful case planning involving the surgical team, prosthodontic team and well coordinated laboratory support . The development of angled screw retained corrective abutments (Fig. 1A) allowed exact implant position to become secondary to providing a stable, functionally well balanced and an aesthetically pleasing occlusion (Figs. 1B & C). Once the implants are placed, a screw retained acrylic transitional prosthesis is fabricated and fixed in place. The transitional prosthesis is replaced by a permanent prosthesis once osseointegration is complete. The key to success in full arch cases is the ability to be able to make both surgical and prosthetic changes in real time to accommodate nuances in individual anatomy and function. Most manufacturers incorporate a variety of design characteristics in their lines of implants which can be exploited to achieve initial stability which is imperative for immediate function. Similarly, the prosthodontic team and lab must be able to modify the provisional prosthesis and abutment hardware to accommodate any necessary tilting of an implant.
Fig. 1A

Fig. 1B

Fig. 1C

Despite extensive planning using advanced modalities which include CBCT, digital scanning, 3D printed models integrated with clinical photography, a functional occlusal analysis and an extensive oro-facial exam, there are unpredictable factors that can adversely affect outcomes. One of these is excessive masticatory forces which can be difficult to predict and challenging to mitigate.
The midface is composed of multiple thin bones which are reinforced with vertical septae to resist deformation. However, despite being calcified, bone is inherently flexible (Fig. 2). The maxilla in particular undergoes a small degree of deformation in multiple planes under masticatory loading.18,19 This subtle ‘flexing’ becomes evident when a full arch restoration is placed on implants. Prostheses which are supported by natural teeth are protected by the stress-breaking properties of dental ligaments. In the case of All-on-4® arches, there is no such protective mechanism. When acrylic prostheses are placed, repeated small deformations can result in their fracture (Fig. 3A). In the case of stronger prosthetic materials like Zirconia, interface hardware failure such as retention screw breakage may result (Fig. 3B). Biomechanical factors that commonly exacerbate these types of failures include design problems such as excessive cantilevering or more commonly diurnal and nocturnal parafunctional activities such as clenching or bruxing.
Fig. 2

Fig. 3A

Fig. 3B

Initial overloading of new dental implants and their associated transitional restorations in full arch reconstruction has always been a concern, however, in most patients it has caused fewer setbacks than one would expect. Difficulties, however, can arise from both the mechanics and dynamics of the masticatory system as well as complex parafunctional behaviours. From a mechanical perspective, any individual who has been functioning without posterior support will compensate through some degree of masticatory muscle hypertrophy. The jaw is a class 3 lever. This means that the further the occlusal or incisal surfaces are from the fulcrum (the jaw joints) the more force the masticatory muscles must produce to effectively chew. The natural adaptation for the muscles, predominantly Masseter and Temporalis, is to hypertrophy, allowing for more power to be generated. Once posterior occlusion has been restored with a full arch implant supported prosthesis, the lever arm is effectively shortened, allowing excessive forces to be generated strictly based on the geometry of the lever. Without periodontal ligaments to sense and indirectly regulate muscle forces, prosthetic damage can easily occur.
A more complex problem is that of bite forces generated through clenching or bruxing. A review of the literature by Manfredini21 reports a prevalence of 30% in the adult population for daytime parafunction and 15% for nighttime parafunction. Most dentists have seen first-hand the fractures that result from off-axis or oblique loading on tooth cusps as well as the wear on both natural conventionally restored dentition caused by parafunction (Fig. 4). Full arch implant supported restorations can fracture if the parafunctional forces are high and the modulus of elasticity of the midface is low. In a study of composite density in the maxilla, Seong and colleagues found that the posterior maxilla is less dense and therefore more compressible than the anterior.22 Clinically this would explain why prosthetic breakage is commonly seen in the anterior or in the cantilevered area.23,24,25
Fig. 4

Another difficult to measure and transient aberration in a balanced occlusion is that of temporomandibular joint inflammation. Most clinically symptomatic cases of TMD are unilateral. Joint overloading on one side will lead to inflammatory changes within the joint as well as disc position changes. As such, posterior vertical dimension on the affected side will change, altering the contacts on the contralateral side. Although not yet studied in full arch implant supported restorations, the mechanism is one that must be considered when unexplained dynamic occlusal changes occur.
Until recently mitigation of parafunctional forces has been challenging. Conventional therapies such as intra-oral orthotic appliances provide very limited control in cases that are fully implant restored. In the patient with natural dentition, orthotics such as night guards, regardless of the design, reduce or eliminate parafunction in approximately 50% of cases.26 The remaining 50% of patients are unchanged or have increased parafunction (the ‘chew toy’ phenomenon). Why this occurs has not been thoroughly elucidated but the mechanism appears to involve both positive and negative feedback from sensory receptors in the periodontal ligaments, jaw joints and muscles. Altering the relative input from these sources can either down-regulate (majority of cases) or up-regulate muscle activity which is initiated in the trigeminal nucleus. When all teeth have been removed, any input from the periodontal ligaments is also removed. It should be noted, however, that the prevalence of TMD in full denture wearers is similar to the dentate population.27,28 It has been suggested that the psychological stress of being edentulous and an unstable occlusion are significant causative factors in edentulous parafunction.29 Treatment of patients with full arch implant supported prosthesis in many cases effectively “cures” TMD-related parafunction, likely through a combination of dynamic functional changes as well as psychological changes. However, in those cases which do not respond, appliance therapy is almost universally ineffective. Until recently this proved to be a dilemma. With increasing clinical acceptance of Botulinum toxins such as Botox® (Allergan Inc) in dental practice, a unique opportunity has presented itself.
Botulinum toxin (BTX), a potent pre-synaptic neurotoxin30 is produced by the anaerobic organism Clostridium botulinum.31 Botox® (Allergan Inc. Irvine, CA) is the most well-known, but not the only toxin product in North America. The primary effect of BTX is a dose-dependent weakness or paralysis in skeletal muscle achieved by blocking the release of acetylcholine (Ach) from motor nerve endings.30 The main effect in muscle is on the alpha motor neurons reducing contractile effort. However, BTX may also affect the gamma motor neurons in the muscle spindles32 resulting in lower muscle resting tone. Reversal of local paralysis occurs initially by neural sprouting with re-innervation of the muscle and ultimately by regeneration of the Ach vesicle docking proteins.33 Full function is typically restored in one to five months depending on the muscles treated, dose used and injection location within a muscle.
Parafunctional conditions such as clenching and bruxing respond well to the relaxing effects of Botulinum toxins.34-38 Injecting the major clenching muscles, specifically Masseter and Temporalis with a modest dose of Botox® will reduce the frequency, intensity and duration of clenching without significantly affecting a patient’s ability to chew. The clinical effects of the toxin are dose dependant and duration of a single treatment in the masticatory muscles is in the order of two to three months. The drug is well tolerated with contraindications generally limited to pregnancy, lactation and concomitant muscle wasting diseases.
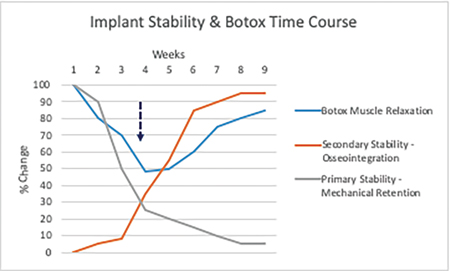
Botox® has been used successfully in the treatment of TMD and pain by the primary author for more than 20 years. Its ease of use, predictable outcome and minimal side effects have allowed it to gain widespread clinical acceptance in implantology.39 Single and multiple implants which are immediately restored and loaded may not osseointegrate if subjected to forces, which cause off-axis loading (i.e. net perpendicular forces overcome primary stability). Full arch restorations have the advantage of cross-arch stabilization and therefore a lower risk of non-integration of implants but as previously noted are more susceptible to cantilever forces and subsequent prosthetic fracture. Botox can be used at the time of implant placement as a single treatment to mitigate overloading during the ‘stability dip’ phase of integration or on a cyclical basis (two or three times per year) to protect full arch prosthesis in bruxers (Fig. 5).
Fig. 5
Treatment with Botox takes less than 15 minutes in the hands of an experienced clinician and adds a nominal amount to the overall cost of treatment, which is modest when compared to the cost of a failed implant case. Although this therapy has been very successful based on clinical observation we do not yet have enough hard data to support a specific treatment protocol. We are presently designing a randomized controlled trial to validate our protocols for full arch immediately loaded implant supported prosthetic rehabilitation.
Oral Health welcomes this original article.
References
- Settineri S., Rizzo A., Liotta M., Mento C., Clinical Psychology of Oral Health: The Link Between Teeth and Emotions, SAGE Open, July-September 2017: 1–7
- Shamrany M., Is depression associated with edentulism in Canadian adults?, Thesis for Master of Science in Dental Public Health, Graduate Department of Dentistry, University of Toronto, 2008: 1-113
- Nowjack-Raymer RE, Sheiham A., Association of edentulism and diet and nutrition in US adults. J Dent Res.2003 Feb;82(2):123-6.
- Andreeva V., Kesse-Guyot E., Galan P., et. al. Adherence to National Dietary Guidelines in Association with Oral Health Impact on Quality of Life, Nutrients 2018, 10(5), 527-38
- Koodaryan R., Hafezeqoran A.,, Nourizadeh A., et al., The Relationship between dental status, body mass index and nutrient intake, Advances in Bioscience & Clinical Medicine, Vol.2(2): 24-33
- Weyant RJ, Pandav RS, Plowman JL, Ganguli M. Medical and cognitive correlates of denture wearing in older community-dwelling adults. J Am Geriatr Soc.2004 Apr;52(4):596-600
- Balaji, S., Textbook of Oral and Maxillofacial Surgery. New Delhi: Elsevier India. (2007) pp. 301–302.
- Misch, Carl E. Contemporary Implant Dentistry. St. Louis, Missouri: Mosby Elsevier. (2007)
- NobelBiocare History https://www.nobelbiocare.com/international/en/our-story
- Shatkin T., Petrotto C., Mini dental implants: a retrospective analysis of 5640 implants placed over a 12-year period. Compend Contin Educ Dent.2012; 33 Spec 3:2-9
- Arlin, M.L. Surgical risk factors in Implant dentistry: Effect on failures and bone loss, Oral Health, August 2015, pp 32-38
- Porter J., von Fraunhofer J., Success or Failure of Dental Implants? A literature review with treatment considerations. J. Acad. Of General Dentistry Nov/Dec 2005: 26-35
- Sadid-Zadeh R, Kutkut A, Kim H., Prosthetic failure in implant dentistry. Dent Clin North Am. 2015 Jan;59(1):195-214
- Branemark, Per-Ingvar (1977). Osseointegrated Implants in the Treatment of the Edentulous Jaw. Sweden: Almquivist & Weksell International. pp. 79, 81, 83
- Kallus T,. Clinical evaluation of angulated abutments for the Brånemark system: a pilot study. Int J Oral Maxillofac Implants. Spring 19905: 39–45
- Lefkove, MD (1990). Immediate loading of cylinder implants with overdentures in the mandibular symphysis: the titanium plasma-sprayed screw technique. J Oral Implantol. 16: 265–71
- Maló P., Rangert B., Nobre M., All-on-Four’ Immediate-Function Concept with Brånemark System Implants for Completely Edentulous Mandibles: A Retrospective Clinical Study. Clinical Implant Dentistry and Related Research. 2003;5: 2–9
- Rafferty K., Herring S., Marshall C., Biomechanics of the Rostrum and the Role of Facial Sutures, J Morphol. 2003 Jul; 257(1): 33
- Stansfield E., Parker J., A sensitivity study of human mandibular biting simulations using finite element analysis Journal of Archaeological Science: Reports, 2018(22):420-432
- The Physics of Chewing, http://ffden-2.phys.uaf.edu/104_2012_web_projects/kjersten_williams/Page_3_Physics_of_Chewing.html
- Manfredini D., Winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F. Epidemiology of bruxism in adults: a systematic review of the literature. J Orofac Pain. 2013 Spring;27(2):99-110.
- Seong W., Kim U., SwiftJ., et. al. Elastic properties and apparent density of human edentulous maxilla and mandibleInt J Oral Maxillofac Surg. 2009 October; 38(10): 1088–1093
- Gowd M., Shankar T., Ranjan R., Sin A. Prosthetic Consideration in Implant-supported Prosthesis: A Review of Literature, J Int Soc Prev Community Dent. 2017 Jun; 7(Suppl 1): S1–S7.
- Tinsley D., Watson C., Preston A., Implant Complications and Failures: The Fixed Prosthesis, Dental Update November 2002:456-60
- Falk H., On occlusal forces in dentitions with implant-supported fixed cantilever prostheses. Swed Dent J Suppl. 1990;69:1-40
- Dao TT. Lavigne GJ. Oral splints: the crutches for temporomandibular disorders and bruxism? Critical Reviews in Oral Biology & Medicine. 9(3):345-61, 1998.
- Patil S., Prasanna R.,, Sreeharsha T., et. al. Prevalence of Temporomandibular Disorders in Patients Wearing Complete Dentures Visiting A Medical College in South India, International Journal of Contemporary Medical Research Volume 3(7) July 2016:1954-7
- Dallanora A., Grasel CE, Heine CP, et. al. Prevalence of temporomandibular disorders in a population of complete denture wearers. Gerodontology. 2012 Jun;29(2):865-9.
- Alzarea B., Temporomandibular Disorders (TMD) in Edentulous Patients: A Review and Proposed Classification (Dr. Bader’s Classification). J Clin Diagn Res. 2015 Apr; 9(4): ZE06–ZE09.
- Simpson LL. The origin, structure, and pharmacological activity of botulinum toxin. Pharmacol Rev 1981;33:155-188.
- Melling J, Hambleton P, Shone CC. Clostridium botulinum toxins: nature and preparation for clinical use. Eye 1988;216-23.
- Filippi GM, Errico P, Santarelli R, Bagolini B, Manni E. Botulinum A toxin effects on rat jaw muscle spindles. Acta Oto-Laryngologica 1993 May;113(3) 400-4.
- Holds JB, Alderson K, Fogg SG. Anderson, RL., Motor nerve sprouting in human orbicularis muscle following botulinum toxin A injection. Invest. Ophthalmol. Vis. Res1990;31:964-7.
- Tan EK, Jankovic J. Treating severe bruxism with botulinum toxin. J Am Dent Assoc. 2000;131:211–6.
- Freund B, Schwartz M. Botulinum Toxin in the Treatment of TMD: A Pilot Study, Oral Health 1998;88(2):32-7.
- Freund B, Schwartz M, Symington J. The Use of Botulinum Toxin for the Treatment of Temporomandibular Disorders: Preliminary Findings. Journal of Oral and Maxillofacial Surgery 1999;(57)8:916-921
- Freund B, Schwartz M. A New Treatment for Temporomandibular Disorders Using Botulinum Toxin. British Journal of Oral Surgery 2000 38(5) 466-471.
- Schwartz M, Freund B. Treatment of temporomandibular disorders with botulinum toxin. Clin J Pain. 2002 Nov-Dec;18(6 Suppl):S198-203. Review.
- Ihde S. Prophylactic use of botulinum toxin in dental implantlogy. Cranio-maxillofacial Implant Dir. 2007;2:3–8.
About the Author
 Dr. Steven Bongard is the founder and clinical head of Chrysalis Dental Centre in Toronto, a dental implant only facility focused on “same day” dental implant solutions. Dr. Bongard has extensive experience in implant placement, bone grafting procedures, as well as the prosthetic component of implant restoration.
Dr. Steven Bongard is the founder and clinical head of Chrysalis Dental Centre in Toronto, a dental implant only facility focused on “same day” dental implant solutions. Dr. Bongard has extensive experience in implant placement, bone grafting procedures, as well as the prosthetic component of implant restoration.
 Dr. Freund received his medical degree from McMaster University and received his dental and specialist training at the University of Toronto. He practices as an Oral and Maxillofacial Surgeon at the Chrysalis Dental Centre in Toronto with special interests in immediately loaded implant rehabilitation, neuromuscular dysfunction of the head and neck and minimally invasive facial rejuvenation. He is a co-founder and a director of the Canadian Society of Neurotoxins in Pain and the Pinnacle Academy of Learning.
Dr. Freund received his medical degree from McMaster University and received his dental and specialist training at the University of Toronto. He practices as an Oral and Maxillofacial Surgeon at the Chrysalis Dental Centre in Toronto with special interests in immediately loaded implant rehabilitation, neuromuscular dysfunction of the head and neck and minimally invasive facial rejuvenation. He is a co-founder and a director of the Canadian Society of Neurotoxins in Pain and the Pinnacle Academy of Learning.
 Dr. John P. Zarb is a staff prosthodontist in the Graduate Prosthodontic Department at the University of Toronto and at Mt Sinai Hospital in Toronto, and a Clinical Assistant Professor at the University of Rochester, Eastman Institute for Oral Health. Dr. Zarb joined Barrie Dental Specialists in 2003. He is a Fellow, examiner and Director of the Royal College of Dentists of Canada, a Fellow in the Academy of Dentistry International, and Fellow in the Academy of Prosthodontics and a former Director of the American College of Prosthodontists.
Dr. John P. Zarb is a staff prosthodontist in the Graduate Prosthodontic Department at the University of Toronto and at Mt Sinai Hospital in Toronto, and a Clinical Assistant Professor at the University of Rochester, Eastman Institute for Oral Health. Dr. Zarb joined Barrie Dental Specialists in 2003. He is a Fellow, examiner and Director of the Royal College of Dentists of Canada, a Fellow in the Academy of Dentistry International, and Fellow in the Academy of Prosthodontics and a former Director of the American College of Prosthodontists.
RELATED ARTICLE: Full Arch Immediate Fixed Implant Rehabilitation: A Case Demonstration












