
Abstract
Over the past few decades, there has been an increase in managing oral implant and periodontal soft tissue deficiencies in the form of recession and tissue contour defects. Some of these phenotypic presentations are a result of tissue trauma around natural teeth and oral implants placed in areas of available anatomical tissue rather than rebuilding and engineering the deficient tissue topography. Guided Tissue Rejuvenation procedures around natural teeth to correct recession defects and oral implants can be utilized with the advent of novel surgical tissue management approaches combined with advanced tissue replacements to aid in correcting natural tissue recession as well as deficient soft and hard tissue topography for the long term preservation and augmentation of natural teeth and oral endosseous implants.
Gingival recession refers to the exposure of the roots of the teeth caused by a loss of gingival tissue and/ or retraction of the gingival margin from the crown of the teeth.
One of the main etiologic factors for the development of recession for patients is tissue trauma caused by vigorous toothbrushing.3 Among other factors that have been associated with recession are: alveolar bone dehiscence, inadequate gingival dimension, periodontitis and orthodontic therapy.3 In addition, anatomical deficiencies such as thin levels of keratinized tissue, thin gingival phenotypes, teeth malpositions, iatrogenic therapy for both natural teeth and implants can predispose patients and sites to the loss of tissue architecture.6
In 1985, P.D. Miller proposed a classification of recession which allows for a reliable prediction of the outcome of treatment regardless of the selected procedure.7 Some of these traditional techniques include the utilization of full access flap approaches with papillary elevation with or without vertical releasing incisions followed by coronal or lateral advancement. These procedures also utilized various types of graft materials which includes autogenous intra/ extra oral subepithelial connective tissue grafts, human derived soft tissue allografts, and soft tissue xenografts.
Over the past few decades, there has been more discussions on the effectiveness and techniques of various modified soft tissue procedures to help correct anatomical deficiencies in the form of gingival recession around natural teeth and oral implants.
Currently, there is a trend in recreating a more natural tissue contour along with phenotypic modification around implants and natural teeth. This modification aids in the correction of gingival recession, contour deficiencies around oral endosseous implants, as well as enhancing tissue contours in full mouth rehabilitation.
Coronal Rotational Advanced Flap Technique (CRAFT)
The Coronal Rotational Advanced Flap Technique (CRAFT) was initially described by Sy, IP in 201210 and utilized in maxillofacial plastic surgery to address a variety of soft and hard tissue deficiencies around natural teeth and oral endosseous implants. The concept of CRAFT is based on oral plastic surgical principles that offers surgical advantages including: 1) ease of tissue release for tension-free mobilization of mucosa to be repositioned along with continued perfusion and maintenance of vascularity to the surgical wound, 2) access for placement of a variety of soft and hard tissue grafting materials directly over anatomical deficient sites, 3) stabilization of tissues utilizing novel suturing techniques for primary wound apposition, stability, and closure.
The technique is initiated with microsulcular incisions with a papillary release followed by a full to partial thickness flap access. Furthermore, the surgical flap is prepared to allow passiveness by a periosteal release that encompasses a vertical, oblique, and circumferential planes of the within the underlying surgical flap access.
Indications for this technique was initially described for treating Miller Class I, II, and III defects using biological mediators in enamel matrix derivatives and natural subepithelial connective tissue.10 Currently, this technique has been further modified with the advent of advanced biological materials in the form of specialized cross/non- cross linked xenogeneic collagen materials. These materials have been shown to be effective in conjunction with the S2 Stack Technique (S2ST) in phenotypic oral tissue modification over natural teeth for recession defects. In addition, these materials have been utilized in edentulous ridges to harmonize, enhance the dimensional volume, and rehabilitate natural physiologic tissue contours.
Patient No. 1 – CRAFT example
The patient is a 52 year old female who presents with gingival recession ~4-5mm at teeth 11 and 21. Clinically, the patient reports chronic root sensitivity. Keratinized tissue levels range from 3-5mm while probing depths present with 2-3mm probings. In addition, there was mild to moderate alveolar bone loss noted proximally. No other complications were noted or reported.
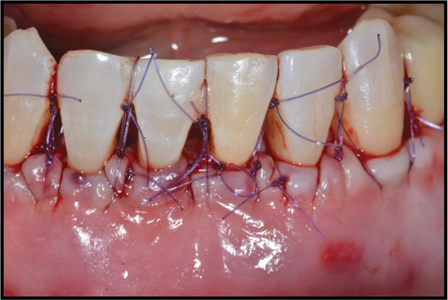
The treatment plan presented to the patient was to achieve root coverage for teeth 11/21. Clinically, one of the concerns was to preserve the mid papilla between these teeth due to the existing proximal bone loss. My surgical treatment plan would be a combination of the coronal rotational advanced flap technique (CRAFT) with inlaid margins at the proximal tissues. Additionally, soft tissue tunnelling was performed thru the mid proximal papilla to aid in the mobility of the surgical area. This coronal rotational advancement was performed and the papillae were positioned within the inlaid margins proximally. This area was stabilized with 5.0 sutures utilizing a combination of interrupted loop sutures and single slings at teeth 11/ 21.
Overall, tissue healing went well and the patient did not have any complications throughout the healing phase. As noted in the final follow up presentations at 1 year, tissue maturation and root coverage were achieved for teeth 11/21.
Patient No. 1 – Root Coverage with CRAFT (Coronal Rotational Advanced Flap Technique) and Inlaid Margins
Fig. 1

Fig. 2

Fig. 3

Fig. 4

Fig. 5

Fig. 6

Fig. 7

S2 Stack Technique (S2ST)
The S2 Stack Technique (S2ST) was first described by Sy IP in 202118 for the treatment of localized moderate to advanced gingival recession (Class I-III Miller Classification) defects along with tissue rejuvenation, and phenotypic modification 15 to rehabilitate the tissue contours for natural teeth and oral implants.
The S2 Stack technique (S2ST) involves the placement of two collagen layers in proximity stacked overlying the involved teeth, implants, or edentulous areas.
Clinically, after initial surgical flap elevation and debridement, the first collagen layer is placed apically as the base. This base layer of collagen tissue is placed on the alveolar bone within 2-3mm of the base of the overlying flap.
A second collagen layer is then stacked in proximity to the initial collagen base layer and is generally positioned on the partially exposed residual roots and in proximity of the CEJ of the anatomical crown.
This coronal (secondary) collagen graft position is a more standard placement location for utilizing connective tissue graft treatments for periodontal recession defects as described in traditional soft tissue coronal advanced flap techniques as well as various tunnelling and modified tunnelling procedures.19-20
The scientific and biologic rational for the apical base layer of collagen (placed over the alveolar bone) is: 1) to provide dimensional anatomic support for the coronal collagen layer (placed over the exposed roots/ proximal areas) and surrounding surgical area, 2) act as a potential conduit to channel blood supply which increases vascularity, perfusion, and nourishment to the underlying collagen grafts, and 3) create an environment to allow for phenotypic modification and engineering of the natural physiologic tissue contours. With the significant increase in tissue volume, a passive surgical wound closure is critical and can be achieved by the coronal rotational advanced flap technique (CRAFT) which encompasses a circumferential, vertical and oblique periosteal release to facilitate tissue movement, transport of vascularity, passive wound closure, and stability.
S2 Stack Technique (S2ST)
Fig. 1
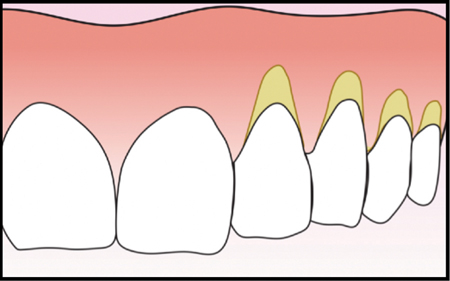
Fig. 2
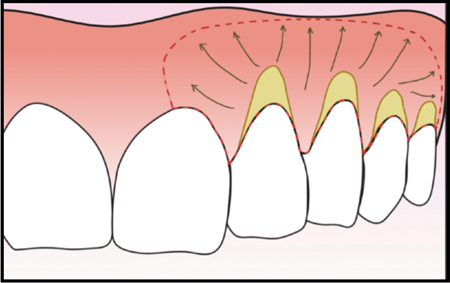
Fig. 3
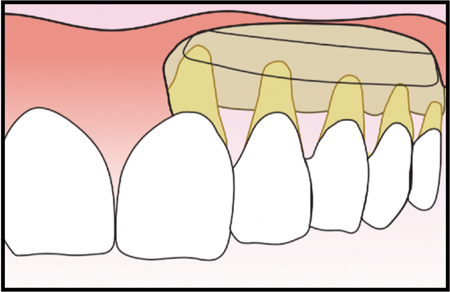
Fig. 4

Fig. 5

Fig. 6

Fig. 7

Fig. 8

Fig. 9
Patient No. 2 – S2 Canine Recession
The patient is a 48 year old male who had presented with a free autogenous graft at the apical aspect for tooth 23 with clinical recession ~4-5mm and ~1mm recession at tooth 24/25. Clinically, the proximal area presented with probing depths ranging from 3-7mm with bleeding on probing at the facial proximal areas of tooth 23. There were no other symptoms reported by the patient. His chief concern was the recession areas as he had occasional thermal sensitivity.
This area was treated with a periodontal flap elevation and bevelled vertical releasing incisions at the outer line angles of tooth 23. Degranulation and debridement of the site were performed. Clinically, there were proximal bone defects noted at tooth 23 which were treated with a bone replacement material. Thereafter, a cross linked expanding collagen was placed over the residual root and alveolar bone of 23 as described in the S2 Stack technique. Periosteal release of the overlying facial flap at 23 and soft tissue tunnelling at the adjacent teeth of 22 and 24/25 were performed. The facial flap was coronally advanced and stabilized with a combination of interrupted loops and single slings at the 23 site.
Overall, the healing and tissue maturation appeared to be going well. Root coverage and natural tissue stabilization for teeth 23/24/25 were achieved as noted in the follow up clinical presentation at 3 years following surgical correction.
Patient No. 2 – Tissue Rejuvenation and Root Coverage with Craft and S2ST
Fig. 1

Fig. 2

Fig. 3
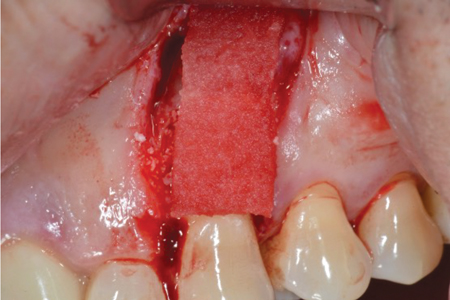
Fig. 4

Fig. 5

Fig. 6

Patient No. 3 – S2ST Papilla Rejuvenation
The patient is a 45 year old female who presents with individual oral implants at sites 11/21/22. Clinically, the proximal papilla between 21 and 22 was not present and presented with a significant hard and soft tissue deficiency. The patient reported chronic food impaction, speech impediment, and air escape within this area.
The proposed treatment plan was to rebuild the lost tissues along with rehabilitating the overall physiologic tissue contours. The area was treated with the S2 Stack technique with two layers of Type 1/3 cross linked xenogeneic collagen. The surgical wound was stabilized utilizing a coronal rotational advanced flap technique.
Overall, the tissue healing, provisionalization, and tissue rehabilitation has been stable for the past 2 years as shown in the follow up views.
Patient No. 3 S2ST Papilla Rejuvenation
Fig. 1

Fig. 2
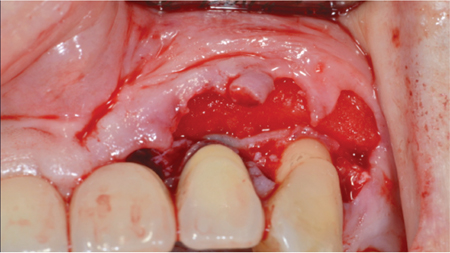
Fig. 3

Fig. 4

Fig. 5

Fig. 6

Patient No. 4 – S2ST Multiple Recession UR Sextant
The patient is a 45 year old male who was undergoing orthodontic invisalign therapy. Full mouth clinical recession were diagnosed along with moderate to advanced periodontal bone loss within the posterior sextants.
The proposed treatment plan was to treat the chronic periodontal disease followed by soft tissue rehabilitation of the recession defects. These recession defects were treated with the S2 stack technique utilizing a specialized cross linked Type I/III xenogeneic collagen matrix. This surgical field was prepared using a coronal rotational advanced flap technique and further stabilized with a combination of D2 slings and S-loop for wound stability and maintenance.
Patient No. 4 – Multiple Recession Therapy with Gingival Rejuvenation utilizing CRAFT and S2ST-Class II/III Defects
Fig. 1

Fig. 2

Fig. 3
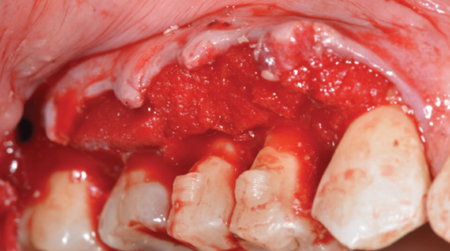
Fig. 4
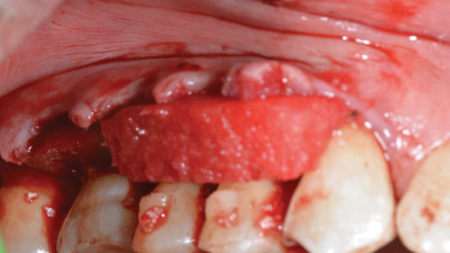
Fig. 5

Fig. 6

Fig. 7

Fig. 8

Patient No. 5 – Full Maxillary Rehabilitation
Patient No. 5-The patient is a 67 year old female who presented with an edentulous maxillary arch. She reported a history of full mouth extractions with no bone or any additional tissue augmentation. According to the patient and the specialist who removed the teeth, the surgical plan was to place 4-5 implants into the existing bone as an all-on-4 treatment. In the interim, she was given an immediate maxillary denture with full palatal coverage. The patient also reported that she was not comfortable with the current interim prosthesis.
Clinically, the remaining maxillary arch topography presented with facial and crestal tissue deficiencies. Radiographically, there appeared to be adequate hard tissue for ideal restorative implant placement but would require tissue augmentation to reinforce and create a natural tissue contour for her future prosthetic therapy. No other complications were noted or reported.
The treatment plan presented to the patient was to rebuild the existing tissue anatomy which included the utilization of bone replacement, growth factor therapy, and collagen matrices to aid in modifying the overall tissue architecture. The maxillary sinuses had pneumatized and would require surgical tissue augmentation prior to endosseous implantation. In addition, the prosthetic plan was to create a maxillary fixed prosthesis (FP) supported by 8 endosseous oral impants.
With the significant planned tissue volumetric change, my surgical treatment plan would be a combination of the coronal rotational advanced flap technique (CRAFT) with a stacked collagen echnique over the bone replacement and growth factor therapy. These surgical releases would allow for passive flap management and primary wound apposition. Overall, tissue healing went well and the patient did not have any complications throughout the healing phase.
Patient No. 5 – Full Maxillary Rehabilitation with (8) endosseous implants & guided Tissue Rejuvenation with xenogeneic hard tissue replacement, amnion chorion placental membrane, and acellular collagen matrices utilizing the S2 Stack and CRAFT release.
Fig. 1

Fig. 2

Fig. 3
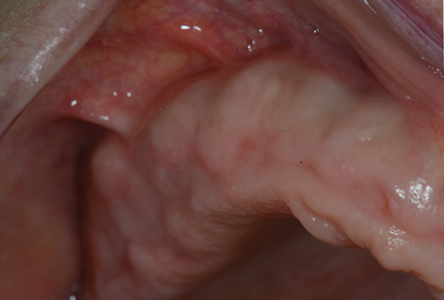
Fig. 4

Fig. 5
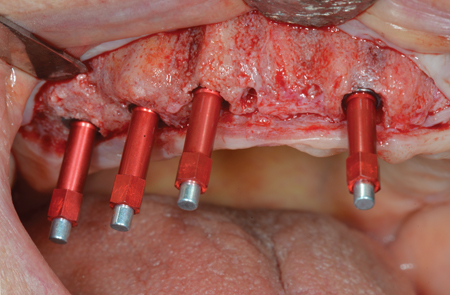
Fig. 6

Fig. 7

Fig. 8
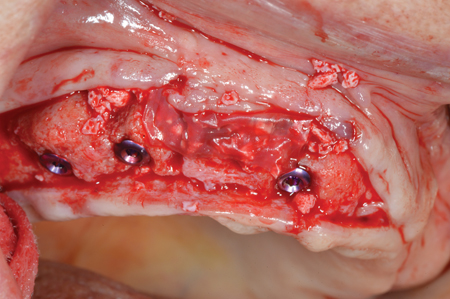
Fig. 9

Fig. 10
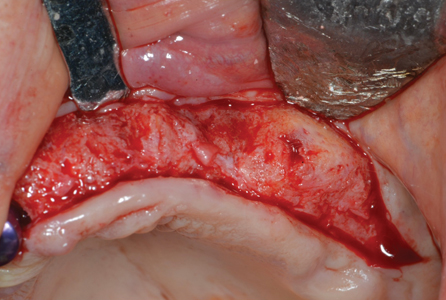
Fig. 11
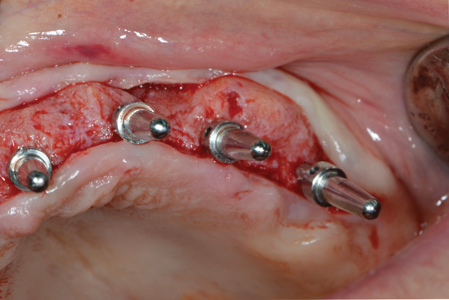
Fig. 12
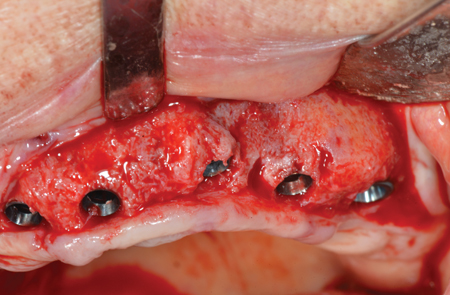
Fig. 13

Fig. 14
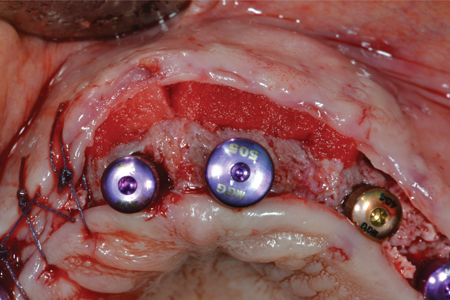
Fig. 15
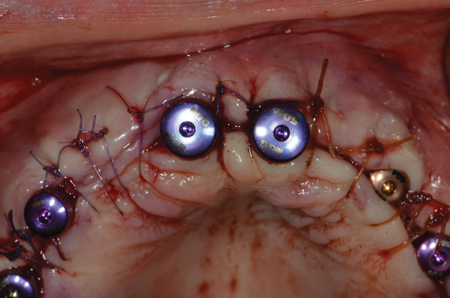
Fig. 16

Fig. 17

Fig. 18
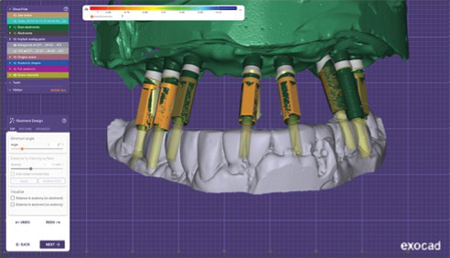
Fig. 19
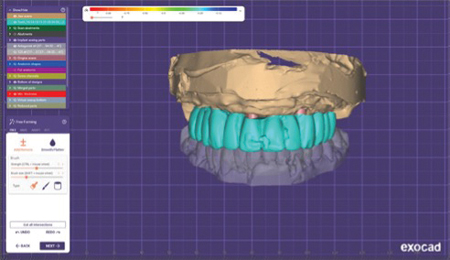
Fig. 20

Fig. 21

Fig. 22
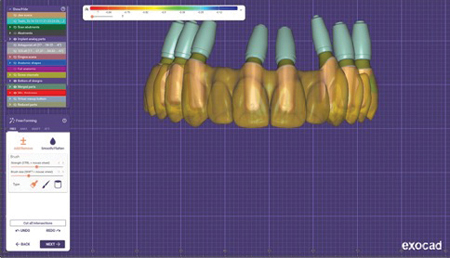
Fig. 23
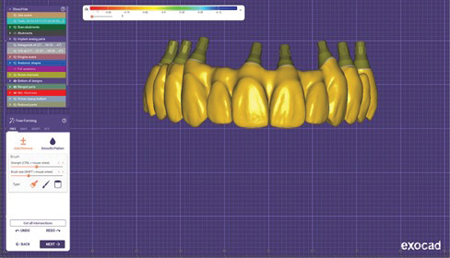
Fig. 24
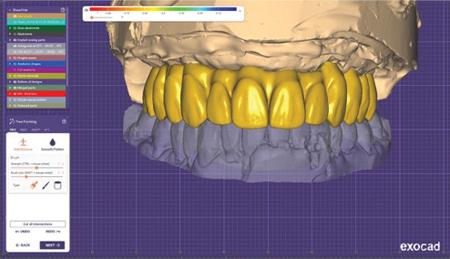
Fig. 25

Fig. 26

Fig. 27

Fig. 28

Fig. 29

Fig. 30

Oral Health welcomes this original article.
Acknowledgements: I would like to take this opportunity to recognize and thank Ms. Fariba Dian for her imagination, design, and dedication in creating these special illustrations for this article. To my late chairman and program director, Dr. Ray C. Williams, thank you for having the vision to believe in me and always encouraging me to be humble, work hard, and strive to be the best you can be. I would also like to recognize my dear friend and mentor, Dr. Gil Montoya for his constant dedication, devotion, and encouragement throughout my career and allowing me to continue to grow and foster in this special field of oral rehabilitation in Implantology and periodontology. To my family, my wife Tammy and daughters Carissa and Rebecca, you have been an inspiration and am so proud of what you do each and everyday. Thank you for always being patient, encouraging, and supporting me in my goals professionally and personally. And to my late mother, without you many things in my life would not be possible. I would not be able to do and live my dreams on a daily basis. I am truly grateful for the opportunities that you have provided and the lessons you have given me.
References
- Brustein D. Cosmetic Periodontics. Coronally positioned pedicle graft Dental Survey 1970 46:22-25.
- Bernimoulin JP et al. Coronally repositioned periodontal flap J Clin Perio. 1975 2:1-1-13.
- Lindhe J, Karring, T, Lang NP Clinical Periodontology and Implant Dentistry, 4th edition 579-586.
- Allen P and Miller PD.“Coronal Positioning of existing gingiva Class 1/2 Recession Defects (1989) J Periodontol 60:316-319 Lindhe J, Karring T, Lang NP periodontology and implant dentistry, 4th edition, 579-586.
- Harris R (1994) Int J Periodont Rest Dent 25:229-241 “The Coronally Positioned Pedicle Graft with Inlaid Margins” Cl. 1/2.
- Kim DM, Bassir SH, Nguyen TT Effect of gingival phenotype on the maintenance of periodontal health: American Academy of Periodontology best evidence review. J P. Periodontal. 2020; 91(3):311-338.
- Miller PD. A classification of marginal tissue recession. Int J Periodontal Rest Dent. 1985; 5, 8-13.
- Cairo F, Pagliaru U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: a systematic review. J Clin Periodontal. 2008; 35 (Suppl. 8): 136-162.
- Zucchelli G, Mele M, Mazzotti C, Marcatori M, Montebugnoli L, and De Sanctis M. Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: A comparative controlled randomized clinical trial. Journal of Periodontology. July 2009, Vol. 80, No. 7, 1083-1094.
- Sy, IP. Growth in Recession-An Esthetic Case Selection for Straumann Emdogain 30-31, 2012.
- Bittencourt S, Del Peloso Ribeiro E, Sllum EA, et al. Semilunar Coronally positioned flap or subepithelial connective tissue graft for the treatment of gingival recession: a 30 month follow-up study. J Periodontal, 2009:80(7): 1076-1082.
- Sculean A, Cosgarea R, Stähli A, et al. Treatment of multiple adjacent maxillary Miller Class I, II, and III gingival recessions with the modified coronally advanced tunnel, enamel matrix derivative, and subepithelial connective tissue graft: a report of 12 cases. Quintessence Int. 2016;47(8):653-659.
- Cortellini P, Bissada NF. Mucogingival conditions in the natural dentition: narrative review, case definitions, and diagnostic considerations. J Periodontol. 2018; 89 suppl 1:S204-S231.
- Vallecillo C, Toledano-Osorio M, Vallecillo-Rivas M, Toledano M, Rodriguez-Archilla A, Osorio R. Collagen Matrix vs. Autogenous Connective Tissue Graft for Soft Tissue Augmentation: A Systematic Review and Meta-Analysis Polymers 2021, 13, 1810.
- Levine R. Phenotype Conversion Using Geistlich Fibro-Gide® for Immediate Implants in the Esthetic Zone. A Case Report. June 2021 Biobrief.
- Thoma D, Zeltner M, Hilbe M, Hammerle C, Jung R. Random controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites June 2016 J. Clin. Periodontol.
- Zeltner M, Jung R, Hammerle, C, Husler J, Thoma, D Randomized controlled clinical study comparing a volume-stable collagen matrix to autogenous connective tissue grafts for soft tissue augmentation at implant sites: linear volumetric soft tissue changes up to 3 months.
- Sy, IP Natural Tissue Rejuvenation utilizing CRAFT and S2ST-A Palate Free Approach June 2022-Vancouver British Columbia Canada.
- Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994;14(3):216-227.
- Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage Dent Clin North Am. 1993 Apr;37(2):243-64.
- Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent. 2011;31(6):653-660.
About the Author

Dr. Ira Paul Sy is the former Director of Oral Implantology and Periodontology at the University of British Columbia. He is also a visiting professor at the University of North Carolina, and the Director of Vancouver Institute of Osseointegration and Oral Tissue Rehabilitation. He owns a private practice, Pacific Periodontal and Implant Centre, in Vancouver.









