A Retrospective Study with 2 to 6 Years of Follow-up
Immediate loading of dental implants is a protocol that has become increasingly widespread since it began to be used in the 1990s1-3 and today has success rates similar to those of implants inserted using the “conventional” loading protocol (98.2% for immediate loading versus 99.6% for conventional loading).4
In 2002, the Spanish Society of Implantology issued a consensus document for immediate and early loading dental implants, recommending a series of specifications for its implementation: adequate primary stability (30-50 Ncm), bone density type I, II and III, soft occlusion in full arch and nonocclusal loading in bridges or unitary teeth.5 A systematic review that has been published in 2007, has maintained the aforementioned recommendations, although it has been clarified that the insertion torque should be higher for single-unit prostheses (30-45 Ncm) than for multiple prostheses (20 Ncm) and a minimum recommended implant length of 11 mm was established for unitary prosthesis.6 This review has also indicated the importance of the insertion torque for the success of immediately-loaded implants. It is not until 2009 that immediate loading prostheses are considered, the suitability of their removal after placement and the way in which this should be carried out, as well as whether their handling affects the success of the treatment. 7 The first study published on this subject concludes that removing the prostheses up to 10 days after the insertion of the implants does not affect their survival and removing them after this period of time does not reduce the survival of the implants studied. 7 The maximum response within the 10-day period becomes more significant from the third day.Nowadays, according to current protocols, it is known that to achieve a successful treatment with immediate loading a series of parameters must be followed: to increase the diameter of the implant (which improves the prognosis of survival), the insertion torque must be at least 20 Ncm for multiple prostheses and between 20 and 45 Ncm for single-unit prostheses (evaluating each case individually) and it is recommended that immediate loading implants should not be used together with other surgical techniques (ridge split, grafts or restoration).4,8-11
Short and extra short implants have joined the trend of immediate loading, although there are few publications on this topic, showing implants ‘survival rates between 87 and 96.6%.12-18
Although the available evidence is encouraging, more clinical studies are needed. In one study, immediate loading of extra short implants, placed in the molar and premolar areas in the maxilla and mandible, has not increased the risk of implant failure scoring a has achieved survival rate for the implants studied of 100%.19 In another study, only one 6.5 mm implant with immediate loading of the 29 studied failed during the follow-up period.20
In the present work, a retrospective study of 6.5 mm long implants with immediate loading is presented to evaluate the long-term behavior of these implants (between two and six years) together with the surgical and prosthetic complications.
Material and Methods
An anonymized database was reviewed to select extra-short implants with a length of 6.5 mm rehabilitated with immediate loading inserted in patients from a single clinic in Vitoria, Spain during the time period of January 2012 to January 2017. The main outcome studied was the survival of extra short implants with immediate loading and the secondary variables were crestal bone stability, prosthetic complications and prosthesis survival.
All patients were evaluated before implants placement by means of diagnostic models, intraoral exploration and a dental CT (Cone-beam) analyzed later by means of a specific software (BTI-Scan II). Before insertion of the implants an orally antibiotic was used consisting of amoxicillin 2 g one hour before the intervention and paracetamol 1 g (as an analgesic). Subsequently patients continued with amoxicillin 500-750 mg every 8 hours (according to weight) for 5 days.
The procedure was performed under local anesthesia and drilling was performed at low speed (biological drilling). Immeditaely after surgery, the defenitive abutment ( Multi-Im abutment, BTI Biotechnology Institute, Vitoria, Spain)) were connected to the implants at a torque of 30-35 Ncm. The one-abutment one-time concept was employed during the prosthodontic phase.
All implants were loaded between 24 and 48 hours after surgery, splinted by resin-metal prosthesis. Pre-articulated titanium bars were used to fabricate the metallic framework of the prosthesis at the time of surgery.
To estimate the marginal bone loss, a known length on the radiographs (implant length) was taken as a reference to calibrate the measurements made on these radiographs. Based on the calibration, the software used calculates the exact measurements (Sidexis XG; Sirona Dental Systems, Bensheim, Germany). The marginal crestal bone loss was calculated by measuring from the implant margin to the first point where the bone to implant contact was evident. The reference for comparing the radiographic records and thus estimating the bone loss occurred in each patient was the x-ray taken at the time of the prosthesis placement. This X-ray was therefore used as the starting point for all the subsequent measurements. Biological and prosthetic complications were identified by reviewing patient history records. Loss of retention (screwed prosthesis), fracture of one of the components of the prosthesis, implant or prosthesis fracture and breakage of the ceramic were considered as criteria for failure of the prosthesis.
The implant was the unit of analysis for descriptive statistics regarding location, implant dimensions, and radiographic measurements. The patient was taken as the unit of measurement for the analysis of age, sex and medical history.
A Shapiro-Wilk test was performed to determine the normal distribution of the sample.
The qualitative variables were described by means of a frequency analysis. Quantitative variables were described by means of the mean and standard deviation. Implant survival was calculated using the Kaplan-Meier method. All analyses were performed with SPSS v15.0 (SPSS Inc. Chicago, IL, USA) and the significance level was set at 5% (p<0.05).
Results
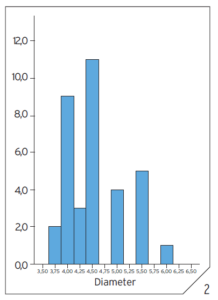
Twenty-seven patients were included, in which 35 immediately loaded 6.5 mm implants were inserted. The mean age of the patients was 66.94 +/- 7.3 years (range 55-72 years). The average insertion torque was 47 Ncm (+/- 13.31), and the Hu values for densitometry measured in the diagnostic CT scan was of 770 Hu (+/- 316.99). The minimum and maximum follow-up time for the implants was 24 and 72 months, with the mean follow-up time being 49 months (+/- 6.3). The 74.3% of the implants were placed in the mandible, the most frequent locations being pieces 37, 45 and 47. The positions of the implants analyzed are shown in Figure 1. All implants were 6.5 mm long. The most common diameter of the implants inserted was 4.5 mm (31.4%), followed by 4 mm (25.7%). The diameters of the implants are shown in Figure 2. 97.1% of the implants were restored with bridges, while only 2.9% of the cases were part of a complete rehabilitation with immediate loading. All implants were restored with screw-retained metal-resin prostheses in the immediate loading phase and splinted to other short or conventional length implants.
Fig. 1
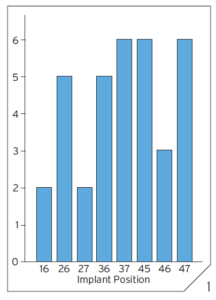
Fig. 2
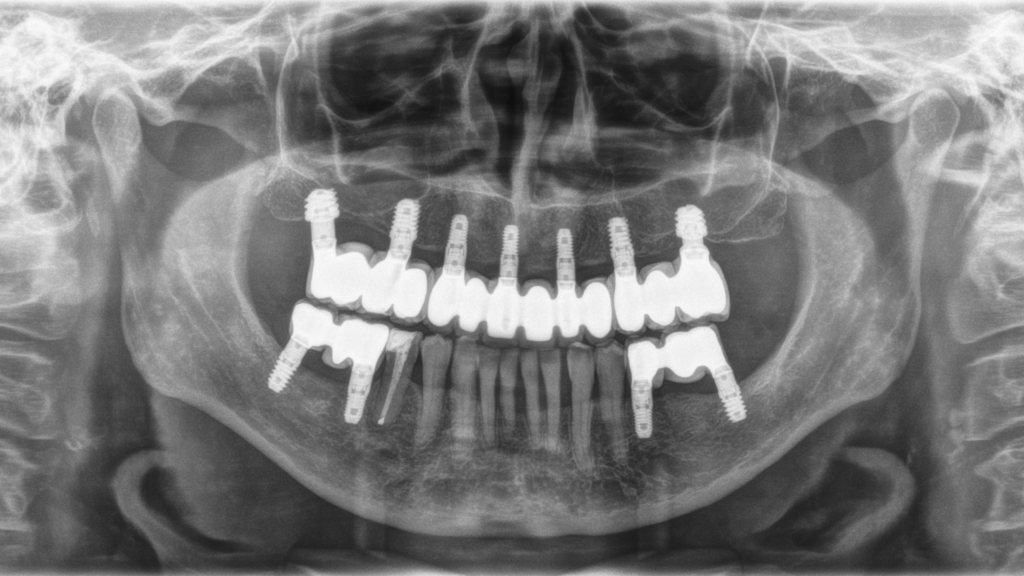
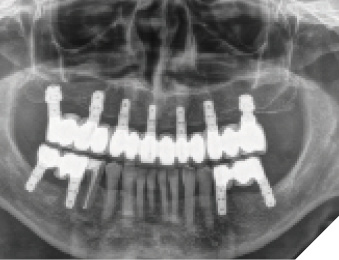
Mean mesial and distal bone loss was 0.6 mm (+/- 0.80) and 0.5 mm (+/- 0.58) respectively. The mean crestal bone loss was 0.4 mm (+/- 0.33). During the follow-up time 1 implant failed, meaning this failure a cumulative survival of 97.1% (Kaplan-Meier). The implant failure occurred in a patient with probable bruxism. No prosthetic complications were registered in the definitive prosthesis phase. One of the cases in the study is shown in Figures 3-20.
Fig. 3
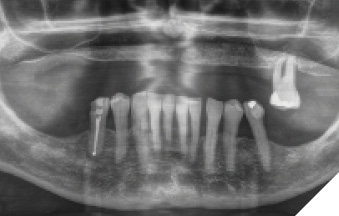
Fig. 4

Fig. 5

Fig. 6
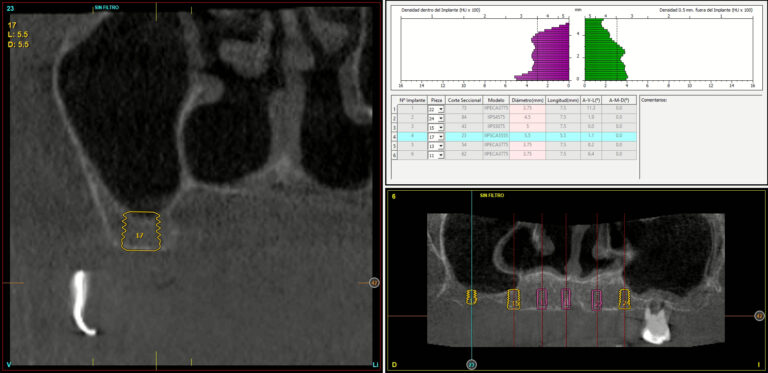
Fig.7
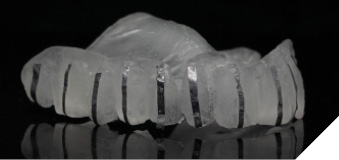
Fig.8

Fig. 9
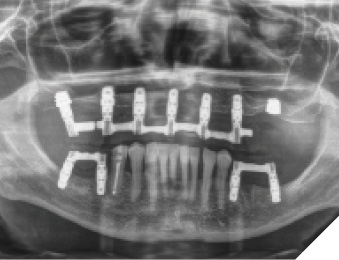
Fig. 10

Fig. 11

Fig. 12

Fig.13

Fig.14
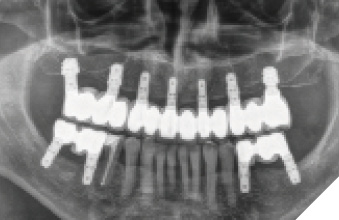
Fig.15

Fig. 16

Fig.17

Fig.18

Fig.19
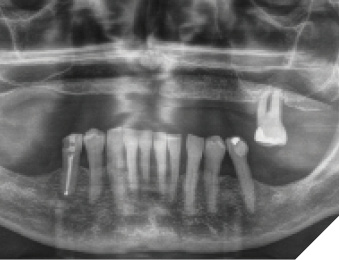
Fig.20
Discussion
Immediate loading of 6.5 mm-long implants has not been a risk factor for implant survival or the marginal bone stability. This study is in agreement with other studies that indicated a high survival rate for immediately-loaded dental implants.15,17
The marginal bone loss of the implants (0.39 mm) is similar to that found in other published studies with similar implants, where values of 0.4-0.5 mm at one year of follow-up has been reported.12,13 At 3-year follow-up, the MBL of 1.25 mm +/- 0.99 mm has been reported.16 When comparing the marginal bone loss of immediately loaded short implants with those of “conventional” length implants, the bone loss and survival figures of short implants are similar. In a randomized clinical trial published by Cannizzaro et al,20 extra-short implants (5 mm) and conventional length implants (11.5 mm) were compared. A mean bone loss of 0.15 mm of crestal bone was observed for extra-short implants after one year of follow-up while conventional length implants showed a mean bone loss of 0.62 mm, these differences being statistically significant. Splinting of short and extra short implants would minimize the stress at the first threads of the implant, and improve the distribution of the loads and minimize lateral loads.21,22 Another important factor when evaluating immediate loading is the initial stability of the implant and quality of the alveolar bone. In this study, all implants has been placed in bone type I,II or III, which allowed the insertion torque to be sufficient (45 Ncm) to avoid micro-movements during the osseointegration period.23,24
Conclusions
Immediate loading of 6.5 mm-long implants, with a adequate primary stability and splinted by the prosthesis, may not be a risk for the survival of the implant or marginal bone stability. However, new studies with larger samples and longer follow-up times are needed to support the results of the study. 
Oral Health welcomes this original article.
References
- Lefkove MD, Beals RP. Immediate loading of cylinder implants with overdentures in the mandibular symphysis: the titanium plasma-sprayed screw technique. J Oral Implantol. 1990;16(4):265–271.
- Hruska AR, Borelli P. Intra-oral welding of implants for an immediate load with overdentures. J Oral Implantol. 1993;19(1):34–38.
- Rosenlicht JL. Advanced surgical techniques in implant dentistry: contemporary applications of early techniques. J Dent Symp. 1993;1:16–19.
- Sanz-Sánchez I, Sanz-Martín I, Figuero E, Sanz M. Clinical efficacy of immediate implant loading protocols compared to conventional loading depending on the type of the restoration: a systematic review. Clin Oral Implants Res. 2015;26(8):964–982.
- Aparicio C, Rangert B, Sennerby L. Immediate/early loading of dental implants: a report from the Sociedad Española de Implantes World Congress consensus meeting in Barcelona, Spain, 2002. Clin Implant Dent Relat Res. 2003;5(1):57–60. doi:10.1111/j.1708-8208.2003.tb00183.x
- Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22(6):893–904.
- Borges AF, Dias Pereira LA, Thomé G, Melo AC, de Mattias Sartori IA. Prostheses removal for suture removal after immediate load: success of implants. Clin Implant Dent Relat Res. 2010;12(3):244–248. doi:10.1111/j.1708-8208.2009.00157.x
- Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22(6):893–904
- Su M, Shi B, Zhu Y, et al. Comparison of implant success rates with different loading protocols: a meta-analysis. Int J Oral Maxillofac Implants. 2014;29(2):344–352.
- Benic GI, Mir-Mari J, Hämmerle CH. Loading protocols for single-implant crowns: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2014;29 Suppl:222–238.
- Huynh-Ba G, Oates TW, Williams MAH. Immediate loading vs. early/conventional loading of immediately placed implants in partially edentulous patients from the patients’ perspective: A systematic review. Clin Oral Implants Res. 2018;29 Suppl 16:255–269.
- Anitua E. Immediate Loading of Short Implants in Posterior Maxillae: Case Series. Acta Stomatol Croat. 2017;51:157-162
- Anitua E, Flores J, Flores C, Alkhraisat MH. Long-term Outcomes of Immediate Loading of Short Implants: A Controlled Retrospective Cohort Study. Int J Oral Maxillofac Implants. 2016;31:1360-1366.
- Alvira-González J, Díaz-Campos E, Sánchez-Garcés MA, Gay-Escoda C. Survival of immediately versus delayed loaded short implants: A prospective case series study. Med Oral Patol Oral Cir Bucal. 2015;20:e480-8.
- Maló P, de Araújo Nobre MA, Lopes AV, Rodrigues R. Immediate loading short implants inserted on low bone quantity for the rehabilitation of the edentulous maxilla using an All-on-4 design. J Oral Rehabil. 2015;42:615-23.
- Rossi F, Lang NP, Ricci E, Ferraioli L, Marchetti C, Botticelli D. Early loading of 6-mm-short implants with a moderately rough surface supporting single crowns–a prospective 5-year cohort study. Clin Oral Implants Res. 2015;26:471-477.
- Cannizzaro G, Leone M, Torchio C, Viola P, Esposito M. Immediate versus early loading of 7-mm-long flapless-placed single implants: a split-mouth randomised controlled clinical trial. Eur J Oral Implantol. 2008;1:277-92.
- Degidi M, Piattelli A, Iezzi G, Carinci F. Immediately loaded short implants: analysis of a case series of 133 implants. Quintessence Int. 2007;38:193-201.
- Anitua E, Flores C, Flores J, Alkhraisat MH. Clinical Effectiveness of 6.5-mm-Long Implants to Support Two-Implant Fixed Prostheses in Premolar-Molar Region: The Influence of Immediate Loading and the Length of Splinting Implant. J Prosthodont. 2019;28:e688-e693.
- Cannizzaro G, Felice P, Leone M, Ferri V, Viola P, Esposito M. Immediate versus early loading of 6.5 mm-long flapless-placed single implants: a 4-year after loading report of a split-mouth randomised controlled trial. Eur J Oral Implantol. 2012;5(2):111–121.
- Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent 2010; 30: 89-95.
- Pierrisnard L, Renouard F, Renault P, Barquins M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res 2003; 5: 254-262.
- Gapski R, Wang HL, Mascarenhas P, Lang NP. Critical review of immediate implant loading. Clin Oral Implants Res 2003; 14: 515-527.
- Barewal RM, Stanford C, Weesner TC. A randomized controlled clinical trial comparing the effects of three loading protocols on dental implant stability. Int J Oral Maxillofac Implants 2012; 27: 945-956.
About the Author

Dr. Anitua has a Degree in Medicine and Surgery from the University of Salamanca, Doctor of Medicine from the University of Valencia, Specialist in Stomatology from the University of the Basque Country (UPV/EHU) and Diploma in Prosthetics and Occlusion from the Pankey Institute (Florida, USA). He is a visiting professor at more than 20 universities in the USA (Harvard, Boston, Tufts, Pennsylvania, New Orleans), Germany (Berlin), England (Bristol), Italy (Milan, Torino), India, Mexico, Brazil, Portugal, Argentina, Colombia, Venezuela, Uruguay, Spain (Seville, Madrid, Barcelona, Murcia, Oviedo…).