Temporomandibular disorders (TMDs) are the most common non tooth-related reasons for chronic orofacial pain, affecting 5-12% of the population with 75% of the population presenting at least one sign and 35% presenting at least one symptom of TMD. Women are twice as likely to experience pain symptoms due to hormonal, biological and psychosocial factors. A number of clinical signs and symptoms include muscle tenderness, limited mouth opening and lower jaw mobility, deep and continuous pain triggered by mastication or parafunction, referred pain to ears, face, head, neck and shoulders with hyperalgesia due to inflammatory changes. The condition involves the muscles of mastication (masseter, temporalis, pterygoids, temporomandibular joints (TMJs) and associated structures (teeth, eyes, ears). In younger patients, functional disorders present with symptoms such as clicking, subluxation and dislocation. Eventually, in 30 to 50-year-old group, arthritis and limited mandibular movement follows. Osteoarthritis (OA) is the most common type of arthritis affecting the TMJ, same as any other functioning joint over time, it is characterised by deterioration of articular tissues and remodelling of the underlying subchondral bone.1 The etiology of TMDs is multifactorial and not very well understood, the factors could be subdivided into those causing the onset (malocclusion, trauma) and those interfering with healing (parafunctional habits, stress, depression, occlusal interferences). TMD is the second most common pain condition of the musculoskeletal system after chronic low-back pain, it can affect the quality of life, cause depression, result in loss of work and income due to disability and psychosocial isolation. In the U.S., the annual TMD management costs have doubled in the last 10 years to over 4 billion dollars.2 The treatment of TMD involves multidisciplinary approach and collaboration between the dentist, medical doctor, psychologist and physiotherapist. Conservative and reversible treatment modalities such as behaviour modification, medications, physiotherapy, orthopedic appliances are preferred.3 The nonsteroidal anti-inflammatory drugs (NSAIDs) are the first choice of pharmacologic intervention because the inflammatory disorders are considered to be the main reason for TMJ pain.4 These drugs may reduce the inflammation, but long-term use may carry a risk of gastric ulcer and nephrotoxicity. Amitriptyline, a tricyclic anti-depressant (TCA), is routinely used in the treatment of depression associated with chronic pain but carries its own side-effects such as drug-induced xerostomia. In recent years, photo-bio-modulation (PBM) has been suggested as an alternative anti-inflammatory, analgesic, physiotherapeutic and muscle relaxant treatment, without any risks or side-effects associated with TCA and NSAID therapy.
New Classification based on Diagnostic Criteria
According to Schiffman et al. (2014)2, diagnostic criteria for TMD are divided into three main groups:
- Myalgia
a. Local myalgia
b. Myofascial pain
c. Myofascial pain with referral - Arthralgia
- Headache
Myalgia is described as pain of muscle origin affected by jaw movement, mastication and parafunction. Clinical examination should confirm pain in temporalis and/or masseter extra-orally and pterygoids intra-orally. Local myalgia pain is localized to the site of palpation, myofascial pain is reported to spread beyond the site of palpation but within the muscle boundary, myofascial pain with referral can go beyond the muscle boundary.
Arthralgia is described as pain of joint origin affected by jaw movement, function or parafunction. The patient would present with chief complaint of pain in the jaw, temple, ear or in front of the ear exacerbated by jaw movement, eating, clenching or grinding. Clinical examination should confirm pain localized to TMJ during palpation around the lateral pole, pain upon maximum opening and right or left lateral or protrusive movements of the mandible.
TMJ Headache is described as headache in the temple area affected or precipitated by the jaw movement, function or parafunction, could be replicated clinically by palpation of the temporalis muscle and lateral or protrusive movements of the mandible.2
TMD diagnosis must be provisional upon 30-day time frame of patient reporting the pain, identification of all relevant anatomical locations by the clinician by palpation tests and elimination of other possible causes of pain, such as odontogenic pain referring to TMJ as well as headaches of other origins. Collaboration with other healthcare professionals is essential for correct diagnosis of TMD. Magnetic Resonance Imaging (MRI) and CBCT are very valuable in confirming dislocations, stretched or torn ligaments, arthritic changes or rare anatomic malformations.
Photo-Bio-Modulation (PBM) Therapy
Historically, many names have been given to this non-pharmaceutical treatment modality: light photo therapy, laser photo therapy, low level laser therapy (LLLT), cold laser therapy, soft laser therapy, laser bio-stimulation and inhibition. All these terms are now grouped together as Photo-Bio-Modulation. Stimulating and analgesic properties of light have been known for hundreds of years from Heliotherapy provided in sunrooms to aid in post-surgical recovery in hospitals and sanatoriums in 1900s; Nobel prize in Medicine in 1903 awarded to Niels Ryberg Finsen (1860-1904) for the treatment of Lupus Vulgaris with Carbon Arc Lamp to Actinotherapy using UV light to treat skin conditions in 1920-30s. More recently, the invention of first ruby laser by Theodore Maiman and Gordon Gould in 1960 and the discovery of Biostimulation properties of He-Ne laser in 1964 by Endre Mester in communist Hungary, reminded us of the healing power of light.
Even though, there is no consensus in scientific literature on the effectiveness of any particular laser wavelength or protocol in the treatment of TMD, many clinicians see the benefit of PBM as a treatment modality in the management of TMD. The only fact systematic reviews of literature can agree on is that it’s impossible to confirm or deny the benefit due to varying protocols described (number and duration of laser applications, wavelengths of the laser or LED (light emitting diode) devices used, power output, mode of delivery, energy density) and poor reporting of all the parameters. If a successful study did not completely disclose all the parameters, right down to contact or non-contact mode of application and the speed of movement of the delivery attachment, the results cannot be replicated; and if they cannot be replicated, they cannot be trusted. Depending on the study, laser applications varied from 3 (1/week for 3 weeks) to 20 (2-3/week for 8 weeks), duration varied from 10 seconds to 10 minutes, wavelengths varied from 632 to 910nm, power varied from 17mW to 27W, mode varied from continuous wave to 1500 pulses per second (repetition rate) and energy density (dose delivered) varied between 1J/cm2 to 105J/cm2. How can anyone look at all this variation of parameters and expect to find one protocol that works in all circumstances? It is not possible! And this lack of consensus is all that is required by sceptics to dismiss this non-invasive and inexpensive treatment option as an alternative to the more conventional and proven pharmaceutical management. The only indication currently supported by a systematic review is the use of PBM in the treatment of arthritic TMD, which is more effective than in the treatment of masticatory muscle disorders.5
Investigations supporting the use of PBM in the treatment of TMD
PBM works by stimulating electron transport chain within the mitochondria, increasing vascularization and fibroblast activation. Improved cellular respiration leads to an increase in ATP production, which is the energy currency of the cell necessary to repair itself. Anti-inflammatory effects are due to the decrease in histamine and acetylcholine release and reduction of the synthesis of bradykinin. Improvement in microcirculation and lymphatic drainage, reduction of prostaglandin E2 (PGE2) and cyclooxygenase-2 (COX2) levels cause reduction in edema. Analgesic effects are due to the increase in the ß-endorphin production and increase in urinary excretion of glucocorticoids (inhibitors of ß-endorphin synthesis), reduction in the production of substance P as well as increase in the pressure pain threshold through an electrolytic nerve fiber blocking mechanism.
A couple of recent animal studies have shed some light on the specifics of the Why? and How? of PBM action and I would like to discuss the results of four such studies:
Carvalho CM et al. (2011)6 suggested that inflammatory response in TMJ may vary from other synovial joints, like a knee joint, due to the presence of dense fibrous tissue covering compared to just hyaline cartilage. Denser innervation of TMJ leads to higher concentration of Substance P (SP) and peptide related to calcitonin and neuropeptide Y in patients suffering from TMD. A polysaccharide called Carrageenan was used in this blind randomized control trial to induce experimental inflammation in TMJ of rats. Twin Laser (MMoptics, Brazil) with 780nm and 660nm wavelengths was used. (Fig. 1) PBM protocol was started 24 hours after induction of inflammation and was repeated every 48 hours for 3 or 7 days, spot size of 0.04cm2 was irradiated in continuous wave mode (CW) with 50mW (780nm) power for 3 min, dose 225J/cm2 alone or for 1 minute, dose of 112J/cm2 plus 40mW (660nm) power for 2 min, dose 120J/cm2. The study compared infrared (780nm) laser (IR) alone with penetration depth of 3mm to IR + red (660nm) laser (R) with penetration depth of 1mm and showed statistically more significant reduction in the inflammation and the number of cell layers of the synovial membrane with IR (3 min) laser alone that with IR(1 min) + R(2min) combined. Irradiation 24 hours prior to induction of inflammation did not yield better results which suggests the concept of preconditioning with laser prior to surgical procedures to reduce post-op inflammation is not supported by evidence. The study concluded that PBM does cause positive effects by reducing the inflammatory reaction and accelerating the inflammatory process leading to faster resolution with the use of 780nm IR laser at 225J/cm2 dose.
Fig. 1

2. Lemos GA et al. (2016)7 induced TMJ arthritis in rats by intra-articular injection of CFA (Complete Freund’s Adjuvant) solution and compared the effect of PBM on the left TMJ versus the untreated right side TMJ. The experimental protocol was as follows: 830nm laser (LaserPulse, IBRAMED) (Fig. 2) at 30mW power, 0.116cm2 spot size, 0.25W/cm2 power density, 12 seconds exposure time, 3J/cm2 total dose, beginning 1 week after CFA injection over 7 sessions, 48 hours apart. The animals were sacrificed 28 days after arthritis induction. Histopathological analysis performed on the condyle, cartilage and articular disc in the PBM group revealed significantly less resorption in mandibular fossa and less chronic inflammatory infiltrate. There was a significant reduction in articular disc thickness in all three areas of the disc (anterior, middle and posterior). Birefringence analysis of collagen fibers showed better arrangement and compaction of the collagen fiber network compared to the untreated arthritis group (AG). The study also measured the concentration of sulfated GAGs (glycosaminoglycans) which was reduced in PBM group compared to control AG but not to a significant degree. Zymography for matrix metalloproteinases (MMPs) revealed a significant decrease in both active and latent MMP-2s and MMP-9s, which play a role in the degradation of the components of the extracellular matrix (ECM) in the disc and articular cartilage of the TMD patients with OA.
Fig. 2

This randomized control study suggests that PBM can increase the remodelling and enhance tissue repair in TMJ of rats with induced arthritis.
3. De Freitas RA et al. (2020)8 simulated traumatic compression injury to the articular disc in the rat TMJ and analyzed the nociceptive behaviour of animals and neuronal activity in the trigeminal nucleus in this acute pain model. The study was aimed at simulating clinical situation such as the acute displacement of the articular disc, when intense pain due to damaged nerve endings and inflammatory process from the acute trauma occur. In this single blind controlled randomized trial, the four groups were: control without TMJ exposure, control with TMJ exposure without injury with SHAM laser, TMJ exposure with injury (representing acute disc trauma) and TMJ exposure with injury and PBM. Laserpulse 904nm super-pulsed laser (IBRAMED, Brazil) was used for 20 days, starting 2 days after induced trauma to the disc for 10 sessions every second day. Laser parameters were 43mW average power with 75W peak power and 60ns pulse duration at 9500Hz repetition rate, spot size 0.13cm2, power density 334mW/cm2, dose delivered 5.95J/cm2 over 18 seconds exposure time. If we compare these laser parameters to the previously mentioned study by Lemos et al, 50% more energy was delivered using higher average power for longer application time, the laser device used was the same, but the dialed-in wavelengths were not (830nm vs. 904nm). Modern lasers can have multiple wavelengths built in which gives the operator choice to modulate the depth of energy penetration required. De Freitas et al. used allodynia test performed by a blinded observer to evaluate the appearance of pain symptoms. Pain onset was confirmed following induced trauma to the TMJ and complete reversal of nociceptive threshold was observed in the PBM group compared to SHAM. Acute pain behaviour reversal in PBM group was statistically significant from the second session and was maintained until the tenth and final session. Immunoblotting of the trigeminal ganglion was used to compare expression of Substance P (SP), vanilloid transient potential receptor 1 (TRPV-1) and peptide related to calcitonin gene (CGRP). These neurotransmitters are part of the trigeminal system used to transmit pain sensory information related to TMJ. PBM group showed statistically significant reduction in the expression of SP, TRPV-1 and CGRP compared to the group with induced acute disc trauma confirming that PBM downregulates the expression of neurotransmitters involved in trigeminal pain pathways and completely reverses nociceptive threshold due to the acute articular disc trauma.
4. Ferrara JI et al. (2019)9 simulated Myalgia component of TMD by injecting CFA solution into the masseter muscle of rats and evaluating nociceptive behaviour at different intervals following PBM therapy. The inflammatory infiltrate was evaluated by histology of the masseter muscle and expression of Fractalkine was evaluated by the immunohistochemistry of the trigeminal ganglia. Fractalkine (FKN) is an inflammatory and pronociceptive chemokine which has a unique connectivity to a receptor CX3CR1 present in microglia. Activation of microglial cells has been implicated in the modulation of orofacial inflammatory pain signalling pathways. (Fig. 3) Red laser (Photon Laser 3, DMC, Brazil) (Fig. 4) of wavelength 660nm with spot size of 0.2cm2 and 30mW of power operated in CW mode delivered a dose of energy of 1.6J/cm2 over 15 seconds of time exposure; this protocol was repeated daily for 7 or 14 consecutive days. A single PBM application was able to reverse the pain for up to 6 hours of evaluation and continued treatments maintained the antinociceptive effect for both 7 and 14 days. The masseter muscle histology demonstrated reversal of the intense inflammatory reaction produced by CFA injection, inhibition of the cellular degradation and regeneration of the muscle cells, as seen by the presence of muscular fibers with central nuclei indicating newly formed immature muscle cells. Immunohistochemistry analysis confirmed the significant reduction of FKN expression and slight decrease in microglial expression in the trigeminal ganglion. Without activation CX3CR1 receptor in microglia by FKN, the lack of activation of this facilitatory mechanism in the trigeminal nociceptive pathway, inflammation and hyperalgesia are inhibited.
Fig. 3
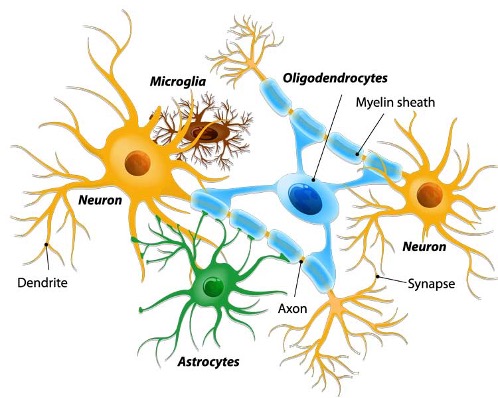
Fig. 4

The study concluded that PBM caused significant reversal of the mechanical hypersensitivity by inhibiting local inflammatory response, decreasing the inflammatory infiltrate in the muscle and central inhibition of fractalkine in the trigeminal ganglion.
I would now like to look at a couple of recent human randomized clinical trials which confirm PBM as a valid treatment modality for the management of TMD:
1. Herpich CM et al. (2019)10 conducted a randomized, sham-controlled, double blind clinical trial to examine efficacy of dual wavelength super-pulsed diode laser in reducing pain and improving function in 30 women suffering from myogenous TMD. The laser protocol combined IR super-pulsed 905nm laser with R 640nm/IR 875nm portable LED clusters from PainAway/PainCure unit by Multi Radiance Medical, Solon, OH, USA (Fig.5). The target of the study was intra-oral stimulation of the lateral pterygoid muscle exhibiting moderate to severe pain to palpation known to be involved in the chronic degenerative myogenous and/or mixed TMDs. The spot size of the intra-oral adapter was 0.4cm2, total energy delivered was 39J per point giving the total dose of 100J/cm2 over five minutes total exposure time. Six phototherapy sessions were conducted over a two-week period; pain and function assessments were performed by a blind examiner before, immediately after, 24 hours and 48 hours after each session. The pain was assessed using Visual Analog Scale (VAS) and the functioning using Patient-Specific Functional Scale (PSFS). The study found significant reduction in VAS pain score after 48 hours and after six sessions of PBM compared to SHAM, mandibular Range of Motion (ROM) measured by digital calipers improved following PBM therapy but was not statistically significant, PSFS analysis of functioning reported a significant improvement by the PBM group. Based on these finding, the activities chosen by the patients for PSFS analysis became substantially more comfortable without much improvement in ROM. Unlike other protocols described in the scientific literature, six sessions, 5 minutes in duration, over a 2-week period can be easily integrated into any dental practice to help with the TMD management.
Fig. 5A

Fig. 5B

Fig. 6

2. Budakoti A et al. (2019)11 prospective single-blind randomized clinical study compared effectiveness of PBM, ultrasound (US) and transcutaneous electric nerve stimulation (TENS) in the treatment of 45 TMD patients (16 males and 29 females) suffering from TMJ pain, joint sounds, limited mouth opening and TMJ locking. The PBM group, US group and TENS group were treated twice a week for 4 weeks for a total of 8 sessions. PBM session utilized 940nm IR diode laser (I-lase, Biolase, USA) for 3 cycles 60 seconds each at 0.5W of power with a thermal relaxation gap of 30-60 seconds in between. 400µm uninitiated tip defocused 1cm away from the tender points (found during clinical examination in the masseter, temporalis muscles and the TMJ area) delivered energy dose of 2J/cm2 to the TMJ and 1.5J/cm2 to the muscles. VAS change in pain and tenderness in TMJ and muscles was reported by the patients and mouth opening was measured with digital calipers by a blind examiner and then used to assess the effectiveness of each physiotherapy method. All three treatment modalities compared in this study are biologic, non-invasive and have no side effects. TENS applies controlled electric current to the surface of the skin which causes muscle relaxation and decreases pain. Therapeutic US is considered to be effective in accelerating healing, increasing the extendibility of collagen fibers, it decreases joint stiffness, improves mobility, reduces muscle spasm thus providing pain relief. PBM improves cellular respiration and ATP production, increases the release of certain growth factors and cytokines, stimulates fibroblasts, accelerates replication mechanisms resulting in the promotion of cell repair processes and reduction in oxidative stress; it improves blood flow, stimulates angiogenesis and lymphatic drainage. The study found significant reduction in the pain, joint tenderness, tenderness to palpation in the masseter and temporalis muscles and improvement in the mouth opening with all three methods compared to baseline. However, PBM group showed the greatest improvement in all the examined parameters, followed by US group, the least improvement was observed in the TENS group. What is very convenient about this particular protocol is that most dental offices already have a small surgical laser unit, such as I-lase (Biolase, USA), so no additional financial investment in the equipment is necessary to offer PBM as an alternative treatment modality to help treat TMD patient in every practice. Unfortunately, most surgical diode lasers come programmed with presets for surgical procedures, such as gingivectomy or troughing, and not with appropriate dosage for delivery of PBM therapy. This is where we need better consensus in the literature and better reporting of all the laser parameters leading to successful outcomes of this therapy. Additional training in the etiology, diagnosis and treatment of TMD and in laser applications is essential to the safe and successful treatment outcomes.
In my office, the protocol I find to be successful in the treatment of myogenous and/or mixed TMD, proven effective in the literature, is as follows:
- I have a surgical Epic X diode 940nm laser which comes with a pain management attachment (Fig.7).
- Safety goggles are mandatory for both the patient and the operator
- Specific trigger points, if palpated, are treated using the protocol of Budakoti et al.,11 0.5W, CW for 3 min defocused 1cm with 400 µm uninitiated tip per point
- In the absence of palpable trigger points, I use the pain management attachment in contact mode with slow massaging movement to cover the entire area of masseter and temporalis muscles, as well as TMJ by treating in front and behind the ear. 4W, CW, 5 min per side. That’s about 1200J of energy delivered to approximately 30 cm2 of the skin surface giving 40J/cm2 delivered dose on the surface.
- The total dosage may need to be adjusted up or down based on the size of the patient, skin color, presence and color of facial hair, thickness of fat layer separating the skin from the muscle and the joint. To understand all these parameters and laser-tissue interactions, I strongly recommend taking a diode laser certification course and hands on workshops in PBM.
Fig. 7A

Fig. 7B

Conclusion
TMD is the second most common cause of pain in the mouth, second only to dental pain of endodontic and periodontal origin. This chronic pain condition can affect over 10% of the population and is twice as common in women than men. Just like neck and back pain can lead to changes in lifestyle, social isolation, depression and cause a drain on economy and medical system, so can TMJ pain. Photo-Bio-Modulation (PBM) using red and infrared diode lasers offers a non-invasive, reversible, reasonably inexpensive treatment modality to help management of TMD without side-effects of traditional pharmaceuticals, superior to therapeutic ultrasound (US) and transcutaneous electric nerve stimulation (TENS). This treatment is slowly gaining support and proof in the scientific literature, but like anything new and innovative, it takes time to become accepted as the standard of treatment. As Arthur Schopenhauer once said: “All truth passes through three stages. First, it is ridiculed. Second, it is violently opposed. Third, it is accepted as being self-evident.”
Oral Health welcomes this original article.
References
- Okeson JP. Management of temporomandibular disorders and occlusion, 6th ed. 2008; The CV Mosby Company, St Louis.
- Schiffman E.et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications. J. Oral Facial Pain and Headache; 2014: 28(1):6-22
- De Lee uw R (ed). The American Academy of Orofacial Pain. Orofacial pain. Guidelines for assessment, diagnosis, and management, 4th ed. Chicago: Quintessence, 2008: 129-204.
- Takeda M et al. Temporomandibular joint inflammation potentiates the excitability trigeminal root ganglion neurons innervating the facial skin in rats. J. Neurophysiol. 2004; 93(5): 2723-2738.
- Melis M et al. Low Level Laser Therapy for the Treatment of Temporomandibular Disorders: A Systematic Review of Literature. J. Craniomand. Practice. 2012; 30(4):1-9.
- Carvalho CM et al. Evaluation of Laser Phototherapy in the Inflammatory Process of the Rat’s TMJ Induced by Carrageenan. Photomed Laser Surg. 2011;29(4):245-254.
- Lemos GA et al. Low-level laser therapy stimulates tissue repair and reduces the extracellular matrix degradation in rats with induced arthritis in the temporomandibular joint. Lasers Med Sci. 2016; 27(1):71-78
- De Freitas RA et al. The effectiveness of photobiomodulation in the management of temporomandibular pain sensitivity in rats: behavioral and neurochemical effects. Lasers Med Sci. 2020; 35(2):447-453
- Ferrara JI et al. Photobiomodulation-induced analgesia in experimental temporomandibular disorder involves central inhibition of fractalkine. Lasers Med Sci. 2019; 34(9):1841-1847.
- Herpich CM et al. Intraoral photobiomodulation diminishes pain and improves functioning in women with temporomandibular disorder: a randomized, sham-controlled, double-blind clinical trial. Lasers Med Sci. 2019; 35(2):439-445.
- Budakoti A et al. A comparative evaluation of the effectiveness of low-level laser therapy, ultrasound therapy, and transcutaneous electric nerve stimulation in the treatment of patients with TMDs: a prospective study. Lasers Dent Sci. 2019; 3:257-267.
About the Author
 Dr. Marina Polonsky graduated from the University of Toronto in 1999 with the Dean’s Gold Medal of Achievement. She is a member of Omega Kappa Upsilon Honour Dental Society and Alpha Omega International Dental Fraternity. Since 1999, Dr. Polonsky maintains a private general practice in Ottawa, with focus on multi-disciplinary treatment utilizing lasers of different wavelengths. Dr. Polonsky holds a Mastership with WCLI (World Clinical Laser Institute), Mastership with ALD (Academy of Laser Dentistry), Mastership in Diode and Erbium lasers from AALZ (Aachen Dental Laser Center), Master of Science degree in Lasers in Dentistry from RWTH University in Aachen, Germany. She is a founder of the Canadian Dental Laser Institute (CDLI.
Dr. Marina Polonsky graduated from the University of Toronto in 1999 with the Dean’s Gold Medal of Achievement. She is a member of Omega Kappa Upsilon Honour Dental Society and Alpha Omega International Dental Fraternity. Since 1999, Dr. Polonsky maintains a private general practice in Ottawa, with focus on multi-disciplinary treatment utilizing lasers of different wavelengths. Dr. Polonsky holds a Mastership with WCLI (World Clinical Laser Institute), Mastership with ALD (Academy of Laser Dentistry), Mastership in Diode and Erbium lasers from AALZ (Aachen Dental Laser Center), Master of Science degree in Lasers in Dentistry from RWTH University in Aachen, Germany. She is a founder of the Canadian Dental Laser Institute (CDLI.












