
The management of MB2 canals in maxillary molars can be challenging1 considering the complexity of the canal anatomy and the presence of calcifications.2,3
The first step in the management of a calcified MB2 canal is the initial scouting with small stainless-steel (SS) hand instruments sizes 6 to 10, which is considered as the most challenging part of the canal preparation procedure. The use of small hand files was associated with a higher incidence of procedural errors, such as inability to reach length, blockage, canal transportation and instrument fracture.4, 5 The outcome of the endodontic treatment may be adversely affected because of the inability of the clinician to properly disinfect and obturate the root canal.
In calcified MB2 canals, initial scouting is frequently preceded by preflaring to facilitate the use of the small SS hand files.6, 7 After scouting and securing the path of the canal, establishing a glide path and shaping the canal should become relatively easy with a low risk of procedural errors.
Many years ago, the use of a single F2 ProTaper (Dentsply, Ballaigues, Switzerland) instrument in asymmetrical reciprocation was introduced for the management of curved canals.8 However, in many canals, scouting with size 8 and 10 hand files, the most challenging procedure, was still required. Reciproc® (VDW Gmbh, Munich, Germany) was later developed with the specific objective of shaping the majority of calcified and curved canals with only one instrument used in asymmetrical reciprocation without scouting and without glide path.
The present article describes the management (canal preparation) of MB2 canals with only one Reciproc® R25 blue instrument used in asymmetrical reciprocation, without initial scouting and without glide path.
Reciproc® blue R25 instrument
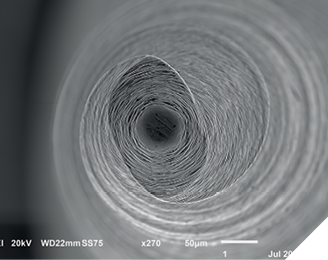
Originally, Reciproc® was made from a nickel-titanium M-wire. Later, Reciproc® blue instruments were introduced. These instruments are made from a heat-treated nickel-titanium wire which enhances their physical properties in comparison to Reciproc M-wire.9, 10 The Reciproc® blue system includes 3 instruments (Reciproc® blue 25, Reciproc® blue 40 and Reciproc® blue 50), matching paper points, matching gutta-percha cones, and matching gutta-percha obturators (GuttaFusion®) (Fig. 1). However, only Reciproc® blue R25 (R25B), which is used for the management of calcified, curved, and MB2 canals is described in this article. The design and the dimensions of R25B are similar to the M-Wire Reciproc® 25 (R25). It has an S-shaped cross-section and a non-cutting tip (Fig. 2). It has a diameter of 0.25 mm at the tip and an 8% (0.08 mm/mm) taper over the first 3 mm from the tip. The instrument tapers off from D3 to D16 to increase its flexibility. At D16, the diameter is 1.05mm. The overall taper is 5%.
Fig. 1A

Fig. 1B

Fig. 1C

Fig. 1D
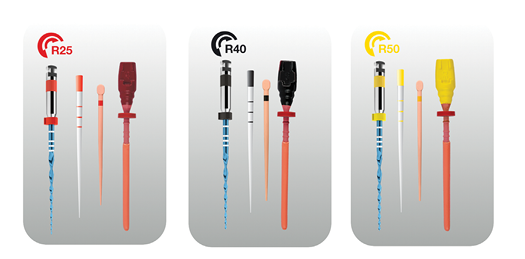
Fig. 1E

Fig. 1F

Fig. 1G

Fig. 2A

Fig. 2B
The instrument is used in conjunction with a motor (Fig. 3) at 10 cycles of reciprocation per second. The values of the forward and reverse rotations are different. When the instrument rotates in the cutting counterclockwise direction (forward rotation) it will advance in the canal and engage dentine to cut it. When it rotates in the opposite clockwise direction, the reverse rotation (smaller than the forward rotation) the instrument will be immediately disengaged. The end result, related to the forward and reverse rotations, is an advancement of the instrument in the canal. The angles set on the reciprocating motor are specific to the Reciproc® blue instruments.
Fig. 3

Clinical procedure
The access cavity is made and the MB2 canal orifice is located. The use of fine ultrasonic tips may be required for this purpose. R25B is not used to locate the orifice. Straight line access to the canal is obtained. The irrigation protocol remains the same.
Canal length is estimated from one or 2 adequately exposed and angulated pre-operative radiographs or from a CBCT image, if available. A silicone stopper is set on R25B at that length.
The guidelines for using R25B for initial endodontic treatments in MB2 canals with different degrees of calcification and curvature are the same. In the majority of the canals, only the R25B is used in reciprocation to complete the canal preparation without the need for initial scouting or creating a glide path. The use of an orifice opener is not required prior to starting the canal preparation with R25B.
Separate MB2 and MB1 canals (Figs. 4, 5)
Fig. 4: Maxillary 1st molar with severe canal calcification and independent MB2 canal. Only one R25B was used in all of the canals of the 1st maxillary molar, including the MB2 canal. R25B is shown in the MB2 canal. Each canal was instrumented with R25B without any prior instrumentation, without initial negotiation and without glide path. Another R25B was used to manage the calcified canals in the 2nd maxillary molar, also without any prior instrumentation.
Fig. 4A
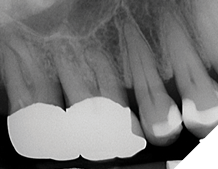
Fig. 4B

Fig. 4C
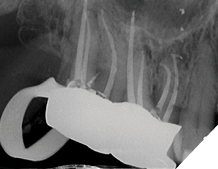
Fig. 5: Maxillary 1st molar with severe canal calcification and independent MB2 canal. Only one R25B was used in all of the canals of the 1st maxillary molar, including the MB2 canal. Each canal was instrumented with R25B without any prior instrumentation, without initial negotiation and without glide path. R25B shown in the DB curved canal.
Fig. 5A

Fig. 5B

Fig. 5C
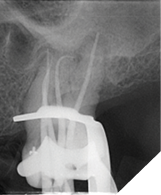
Fig. 5D

The tip of the R25B instrument is placed at the orifice of the canal; the clinician feels that the tip is catching in the orifice. The R25B is then activated in reciprocation to advance into the coronal third of the MB2 canal. The R25B will always be able to advance into the coronal third of the canal regardless of the width of the canal and the severity of the calcification at the orifice of the canal or in its coronal third. The progression may be slow, but progressive, if the canal is calcified or in the presence of a coronal curvature. The R25B will act as an orifice opener due to its enhanced cutting efficiency, which is attributed to its S-shaped cross-section, and the relative strength at its tip.
Once the calcification at the orifice and the coronal third of the MB2 canal is overcome, the apical progression of R25B becomes easier. The instrument is used in the canal with a slow in-and-out pecking motion without pulling the instrument completely out of the canal. The amplitude of the in- and out-movements should not exceed 3-4 mm. Only very light pressure should be applied. The instrument continues advancing in an apical direction. After 3 in- and out-movements, or if resistance is encountered, the instrument is pulled out of the canal to clean the flutes. Canal patency is verified by placing a # 10 file at 1 mm beyond the length reached by R25B. The canal is copiously irrigated. R25B is then re-used in the same manner until the working length has been reached. The progression of R25B is automatically and continuously controlled by the motor’s integrated apex locator. As soon as the working length has been reached, R25B is withdrawn from the canal. The canal is copiously irrigated. An R25B matching cone is fitted at length.
In some canals, R25B will not reach length or its advancement may become difficult. A glide path should then be created. This scenario will be addressed in the Discussion.
Confluent MB1 and MB2 canals (Fig. 6)
Fig. 6: Maxillary 1st molar with severe canal calcification and confluent MB1 and MB2 canals. Only one R25B was used in all of the canals of the 1st maxillary molar, including the MB2 canal. R25B is shown in the MB2 canal. Each canal was instrumented with R25B without any prior instrumentation, without initial negotiation and without glide path. Courtesy of Dr. Mahmoud Shurrab.
Fig. 6A
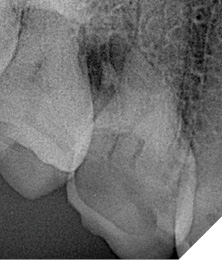
Fig. 6B

Fig. 6C

The above clinical procedure applies to an MB2 canal that is separate from the MB1 canal. However, MB1 and MB2 canals frequently join (Weine’s type II canal configuration).7 Before commencing the canal preparation, the clinician will not be aware if those 2 canals are confluent, unless confirmed by a CBCT image. Therefore, the MB1 canal should be managed first. R25B is used in the same manner as described above. The management of the MB2 canal is started after the MB1 is completely shaped. During the management of the MB2 canal, the MB1 canal should be frequently irrigated and its patency checked with a #10 file to avoid blockage with debris in case both canals join. If the 2 canals join, the irrigant will flow into the other canal and the clinician will have a confirmation that both canals join. The MB2 canal is then shaped with R25B only to the point of confluence with the MB1 canal. The procedure becomes easier and faster. An R25B master cone is fitted to length in the MB1 canal. The cone is kept in the MB1 canal and a second gutta-percha cone is fitted in the MB2 canal to the point of confluence of the 2 canals.
Discussion
Initial scouting with small SS hand files is required for the management of calcified / MB2 canals.7, 11 It can be a challenging procedure associated with an increased risk of procedural errors.
The presence of calcifications at the orifice of the canal and its coronal third represent the first challenge to the progress of small instruments in the canals. These calcifications occur in a coronal-apical direction.3 Removing these obstacles facilitates and makes safer the apical progression of smaller instrument.12 Small hand files with enhanced rigidity (e.g. C Pilot, VDW Dentsply, Germany, and C+ files, Maillefer Dentsply, Switzerland) were developed to enhance the initial scouting through the calcified canals. However, the efficacy of these files remains questionable.13 Moreover, many clinicians pre-enlarge the coronal third of a canal prior to scouting it to length with smaller files. However, scouting can remain challenging and the smaller hand files may not reach working length easily or at all despite the removal of the calcifications present in the coronal and middle thirds of the canal.6
A study assessed the ability of R25 to reach length in calcified MB2 canals, without initial scouting and without glide path.6 The authors labelled a canal as calcified when a size 6 hand file could not easily reach length easily after coronal pre-enlargement. Those were canals in which initial scouting with a size 10 file would likely be difficult , given that even a size 6 file did not advance smoothly to length. The findings showed that R25 reached length in 77% (39/51 canals) of the calcified MB2 canals in first maxillary molars, without scouting with SS files size 8 and 10, and without a glide path. Interestingly, R25 was able to reach the full working length easily in 85.9% (67/78 canals) and 100% (23/23 canals) of MB2 canals that were classified as not calcified (i.e. where a size 6 hand file could reach length easily) in first and second maxillary molars, respectively. These findings were consistent with the clinical results from a previous study.14
Heat treatment of Reciproc® blue files enhanced their torsional and flexural fatigue resistance in comparison to Reciproc® M-wire.9, 10 Consequently, the findings of 2 previous studies on Reciproc M-wire can be extrapolated to Reciproc® blue.6, 14 The validity of the extrapolation was confirmed by the results of a recent ex-vivo study performed by undergraduate students: R25B was able to reach length without an initial scouting and without glide path in 86.67% of MB2 canals.15
A path of least resistance exists in all canals even in those that appear completely calcified radiographically.16-19 The relatively rigid tip (no buckling) of the instrument and the enhanced cutting ability associated with an S-shape cross section allow the instrument to progress through the coronal calcifications by following the path of least resistance. It will not ledge or transport the canal because it is made of a heat-treated nickel titanium wire which increases its flexibility. The pecking motion reduces instrument binding, which is the main reason for instrument fracture.20 Even if R25B binds, which is possible in a calcified canal, the risk of fracture is very low despite the repeated high stresses to which R25B will be subjected to during its progression in a calcified canal without any prior instrumentation. The angles set on the motor are safe with regards to preventing / minimizing instrument fracture.21-23 For example, in a total of 152 MB2 canals (including 51 calcified canals), only one R25 instrument fractured.6
It is important to emphasize that only motors and contra-angles from the manufacturer of R25B should be used. Studies showed that the use of motors from other manufacturers resulted in a variation of the angles of reciprocation which would affect efficiency and safety.24-27 Moreover, one study showed that R25 resulted in canal transportation.28 This was in contrast to other studies showing the safety of Reciproc® R25 and R25B in the management of severely curved canals.29-34 In that study, a contra-angle with a gear ratio higher than the one recommended by the manufacturer was used.28 A higher gear ratio results in a slower speed of reciprocation and, consequently, less cutting efficiency. The advancement of the instrument would be affected and the clinician would tend to apply pressure on the instrument to compensate for the loss of cutting efficiency. Canal transportation would subsequently occur.
Creating a glide path: indication and management
R25B is able reach working length without any prior instrumentation in the majority of canals, including calcified MB2 canals. In some cases, the apical progression of R25B may become difficult or the instrument may cease to advance. In similar situations, apical pressure should not be exerted on R25B. Instead, a glide path should be created. A reciprocating glide path instrument, R-Pilot®, is used for this purpose (Fig 7). The R-Pilot has a diameter of 0.125mm at the tip and a 4% taper. It is used with the same reciprocating motor and settings as R25B, with a light and short pecking motion similar to the use of R25B. After 2-3 pecks, R-Pilot® is removed and the canal is copiously irrigated. The sequence of pecking and irrigation is repeated until R-Pilot® reaches length. Then, the canal preparation to working length is completed with R25B (Fig 8, 9). Before using the R-Pilot®, the canal should be scouted to length with sizes 8 and 10 hand files. These files should be passive at working length; i.e. the clinician should be able to perform 4-5 mm up- and down-movements with minimal resistance.
Fig. 7

Fig. 8: Glide path with R-Pilot after R25B was unable to reach length. Courtesy of Dr. Laura Andriukaitiene
Fig. 8A

Fig. 8B

Fig. 8C
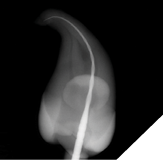
Fig. 8D
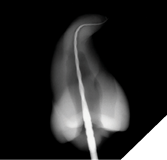
Fig. 9: Glide path in MB2 with R-Pilot after R25B was unable to reach length
Fig. 9A

Fig. 9B
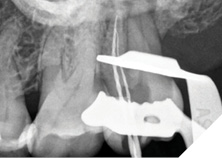
Fig. 9C

The use of the R-Pilot® to create a glide path is based on a crown-down approach: The R-Pilot®, smaller than R25B, will advance easily in an apical considering that R25B pre-enlarged at least the coronal third of the canal before it stopped from advancing.
Conclusions
Reciproc blue R25 can be used safely for the management of the majority of MB2 canals regardless of the degree of calcification, without any prior instrumentation (without initial negotiation and without glide path). It simplifies the procedure considering that only one instrument is used. It helps to overcome the challenges and reduces procedural errors associated with the use of small SS hand files for initial scouting of calcified canals. 
Oral Health welcomes this original article.
References
- Ibarrola JL, Knowles KI, Ludlow MO, McKinley IB Jr. Factors affecting the negotiability of second mesiobuccal canals in maxillary molars. J Endod 1997;23: 236–8.
- Verma P, Love RM. A Micro CT study of the mesiobuccal root canal morphology of the maxillary first molar tooth. Int Endod J 2011; 44: 210-7.
- McCabe PS, Dummer PM. Pulp canal obliteration: an endodontic diagnosis and treatment challenge. Int Endod J 2012; 45: 177-97.
- Jafarzadeh H, Abbott PV. Ledge formation: review of a great challenge in endodontics. J Endod 2007 ;33: 1155-62.
- Ungerechts C, Bardsen Å, Fristad E. Instrument fracture in root canals – where, why, when and what? A study from a student clinic. Int Endod J 2014; 47: 183-90.
- Bartols A, Robra B-P, Walther W. The ability of Reciproc instruments to reach full working length without glide path preparation: a clinical retrospective study. Peer J 2017; Jul 19:5:e3583.
- Kharouf N, Mancino D. An In Vivo Study: Location and instrumentation of the second mesiobuccal canal of the maxillary second molar. J Cont Dent Prac 2019; 20: 131-5.
- Yared G. Canal preparation using only one Ni-Ti rotary instrument: preliminary observations. 2008; 41: 339-44.
- De-Deus G, Silva EJNL, Vieira VTL, Belladonna FG, Elias CN, Plotino G, Grande NM. Blue Thermomechanical Treatment Optimizes Fatigue Resistance and Flexibility of the Reciproc Files. J Endod 2017; 43: 462-6.
- Cîrligeriu L-E, Nica L-M, Pușcu-Boscornea SA, Horhat R-M, Pancotti S, Stoia D-L, Marinescu A-G. Mechanicall Strength evaluation of two single file systems: Reciproc versus Reciproc blue. Rom J Oral Reehab 2020, 12: 109-15.
- Haas M. The notorious MB2 canal: How to find and treat It. Oral Health 2024, May issue.
- Amir FA, Gutmann JL, Witherspoon DE. 2001. Calcific metamorphosis: a challenge in endodontic diagnosis and treatment. Quintessence International 32:447–455.
- Allen MJ, Glickman GN, Griggs JA. Comparative analysis of endodontic pathfinders. J Endod 2007; 33: 723–6.
- Zuolo ML, Carvalho MC, De-Deus G. Negotiability of Second Mesiobuccal Canals in Maxillary Molars Using a Reciprocating System. J Endod 2015; 41: 1913-7.
- Atav Ateş A, Arıcan B, Çiftçioğlu E, Küçükay ES. Negotiating the second mesiobuccal canal: A comparison of nickel titanium files through the experience of undergraduate dental students. J Dent Educ 2023; 87: 694-701.
- Patersson SS, Mitchell DF. Calcific metamorphosis of the dental pulp. OOOOE 1965; 20, 94–101.
- Schindler WG, Gullickson DC. Rationale for the management of calcific metamorphosis secondary to traumatic injuries. J Endod 1988; 14, 408–12.
- Torneck C. The clinical significance and management of calcific pulp obliteration. Alpha Omegan 1990; 83: 50–3.
- Kuyk JK, Walton RE. Comparison of the radiographic appearance of root canal size to its actual diameter. Journal of Endodontics 1990; 16: 28–33.
- Varela-Patiño P, Ibañez-Párraga A, Rivas-Mundiña B, Cantatore G, Otero XL, Martin-Biedma B. Alternating versus continuous rotation: a comparative study of the effect on instrument life. J Endod. 2010; 36: 157-9.
- Kim JW, Ha JH, Cheung GS, Versluis A, Kwak SW, Kim HC. Safety of the factory preset rotation angle of reciprocating instruments. J Endod 2014; 40: 1671-5.
- Ha JH, Kim SR, Versluis A, Cheung GS, Kim JW, Kim HC. Elastic limits in torsion of reciprocating nickel-titanium instruments. J Endod 2015; 41: 715-9.
- Ha JH, De-Deus G, Versluis A, Kwak SW, Kim HC. Safe pseudoelastic limit range under torsional loading with Reciproc Blue. Int Endod J 2019; 52: 244-249.
- Rodrigues EA, Costa DG, Junior F, Dantas LTBL, De-Deus G, Simões-Carvalho M, Silva EJNL. A computer-assisted approach to assess the precision of the reciprocating angles and the rotation speeds of endodontic motors. Appl. Syst. Innov. 2022; 5: 1-14
- Braambati D, Monteiro Netto RC, Coelho MS, Soares AJ, Frozoni M. Reciprocating Kinematics of X-Smart Plus, VDW Silver and, iRoot Endodontic Motors: A Comparison Between Real and Set Values. Braz Dent J 2022; 33: 28-35.
- Monteiro-Netto RC, Braambati D, Arruda-Vasconcelos R, Soares AD, Frozoni M. Evaluation of the rotary kinematics between actual and set speeds of X-Smart Plus, VDW.Silver and iRoot motors. Braz Dent J 2023; 34: s21-26.
- Reynette C, Giess R, Davril J, Martrette JM, Mortier É, Balthazard R, Vincent M. Influence of endodontic motors on the behaviour of root canal shaping instruments: an in vitro comparative study. BDJ Open. 2023 Nov 29;9(1):51.
- Fidler A. Kinematics of 2 reciprocating motors: the difference between actual and set values. J Endod 2014; 40: 990-4.
- Bürklein S, Hinschitza K, Dammaschke T, Schäfer E. Shaping ability and cleaning effectiveness of two single-file systems in severely curved root canals of extracted teeth: Reciproc and WaveOne versus Mtwo and ProTaper. Int Endod J 2012; 45: 449-61.
- Bürklein S, Benten S, Schäfer E. Shaping ability of different single-file systems in severely curved root canals of extracted teeth. Int Endod J 2013; 46: 590-7.
- Bürklein S, Flüch S, Schäfer E. Shaping ability of reciprocating single-file systems in severely curved canals: WaveOne and Reciproc versus WaveOne Gold and Reciproc blue. Odontology 2019;107: 96-102.
- Bane K, Faye B, Sarr M, Niang SO, Ndiaye D, Machtou P. Root canal shaping by single-file systems and rotary instruments: a laboratory study. Iran Endod J 2015; 10: 135-9.
- Saber SE, Nagy MM, Schäfer E. Comparative evaluation of the shaping ability of WaveOne, Reciproc and OneShape single-file systems in severely curved root canals of extracted teeth. Int Endod J 2015; 48: 109-14.
- Filizola de Oliveira DJ, Leoni GB, da Silva Goulart R, Sousa-Neto MD, Silva Sousa YTC, Silva RG. Changes in Geometry and Transportation of Root Canals with Severe Curvature Prepared by Different Heat-treated Nickel-titanium Instruments: A Micro-computed Tomographic Study. J Endod 2019; 45: 768-73.
About the authors

Professor Ghassan Yared completed his endodontic training at University Paris VII (France) and obtained his M.Sc. from the Lebanese University (Lebanon). He has given numerous lectures and continuous education courses worldwide. He is the inventor of single file endodontics and asymmetrical mechanical reciprocation, the basis of modern reciprocation.

Dr. Gary Glassman lectures globally on endodontics, is on staff at the University of Toronto, Faculty of Dentistry in the graduate department of endodontics. He maintains a private practice, Endodontic Specialists in Toronto, Ontario, Canada. His personal/professional website is www.drgaryglassman.com and his office website is www.rootcanals.ca.











