Abstract
When difficulty in obtaining adequate mandibular anesthesia is encountered a systematic approach incorporating the evaluation of patient factors and operator technique will substantially improve outcomes.
Even for the most experienced dental practitioners, consistent, profound mandibular anesthesia remains difficult to achieve 100 percent of the time. This can be stressful for both dentist and patient and is often disruptive to a busy office schedule. All too often dentistry must be performed when local anesthesia is incomplete and there is some degree of patient discomfort compromising both the quality of dental treatment and patient confidence.
There is a wide variance in reported rates of failure of mandibular anesthesia with numbers as uncomfortably high as 48%1 appearing in the literature. The clinical reality is that from time to time mandibular anesthesia will be problematic for every practising dentist regardless of experience.2
There are multiple factors contributing to inadequate mandibular anesthesia but even though several of these factors are out of our control there is still much that can be done to improve success rates. Bear in mind that not all local anaesthetic failures are related to operator technique. Factors such as patient cooperation, facial morphology, preoperative pain,3 patient anxiety, insufficient volumes of local anaesthetic solution, inflammation and infection4 can greatly affect the efficacy of local anaesthetic technique. Furthermore some variations in anatomy5 preclude obtaining good local anesthesia in the mandible and alternative techniques are required.
The following review will address some of the issues related to mandibular anesthesia and provide the clinician with an approach for troubleshooting materials and technique as well as various aspects of patient management.
Factors Contributing to Inadequate Mandibular Local Anesthesia
Anatomy
The goal of all mandibular local anesthesia techniques is to bathe a sufficient length of the inferior alveolar nerve in local anaesthetic to temporarily block the transmission of pain signals. This is achieved by applying a volume of local anaesthetic large enough to cover three nodes of Ranvier (myelin sheath gaps) on the target nerve6 with the average distance between nodes at up to 1.5 millimetres. For a predicable adequate mandibular block local anaesthetic solution must contact the nerve at least 5 millimetres above the lingula where the nerve enters the ramus of the mandible.
Anatomic factors such as the flare of the mandibular ramus, inter-incisal opening, tongue size and posture and the height of the lingula where the inferior alveolar nerve enters the mandible all contribute to the ease or difficulty of achieving adequate local anesthesia. An intra and extra oral evaluation of the patient can provide clues as to how to modify technique for greater success.
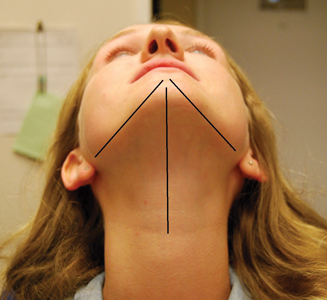
Extra-oral analysis should include palpation of the anterior and posterior borders of the mandibular ramus (Figs. 1 & 2) and the flare of the ramus relative to the mid sagittal plane (Fig. 3). These two approximations will help to determine where theinferior alveolar nerve enters the ramus of the mandible, which has typically been described as at a point 1.0 to 1.5 centimetres above the mandibular occlusal plane and an average of 16.5 millimetres from the anterior border of the ramus.7
Fig. 1
Fig. 2
Fig. 3
When performing a conventional mandibular block the flare of the ramus determines how far posteriorly the barrel of the syringe should be to get as close as possible to a right angle to the medial aspect of the ramus, this approach usually results in a solid contact with the ramus providing a definitive landmark for injection (Fig. 4).
Fig. 4
Introral examination should include inter-incisal distance at maximal mouth opening, the prominence or relative absence of the pterygo-mandibular raphe, the location of the mandibular notch, the anterior border of the ramus, the height of the mandibular occlusal plane relative to the medial aspect of the mandibular ramus and tongue posture.
In many patients the standard point of injection is too low resulting in deposition of local anaesthetic solution at or below the level of the mandibular lingula and thus missing the inferior alveolar nerve. Using a higher injection point (1.5 to 2.0 centimetres above the mandibular occlusal plane and closer to the mandibular notch) will increase success. This is one of the reasons that the Gow-Gates and Vazirani-Akinosi approaches yield a higher success rate than the standard mandibular block technique.8
There is much written in the literature regarding accessory innervation on mandibular teeth as well as rare phenomenon like multiple lingulae and bifid mandibular canals. The significance of these anatomic variances to mandibular anesthesia is difficult to determine.9 The reported failure rate of mandibular block anesthesia exceeds the incidence of accessory innervation of the mandibular molars.10
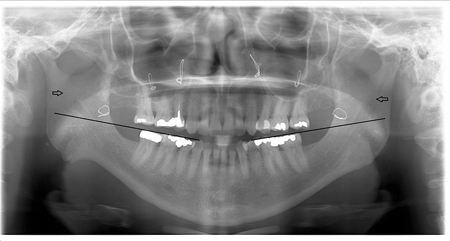
Other less common relevant complicating anatomic factors include severe retrognathia, facial deformities, a history of facial trauma and a history of mandibular surgery. Note the height of the lingula relative to the mandibular plane in the panoramic radiograph in Figure 5. In this post mandibular surgery patient a mandibular block technique placed high on the medial aspect of the ramus was successful in achieving profound local anesthesia while previous attempts using a standard mandibular block technique proved unsuccessful due to the local anaesthetic being injected below the lingula thus missing the inferior alveolar nerve. The high standard block technique is described below.
Fig. 5
Infection and Pre-operative Pain
It has always proven more difficult to adequately anaesthetize patients who are in pain11 or those patients that have an existing infection.12 The presence of preoperative pain and infection are significantly associated with inadequate local anesthesia in both the mandible and the maxilla. The approach to these situations is often patient specific and if dental treatment is urgently required due to pain or infection other modalities such as sedation and general anesthesia may be necessary.
Anxiety
Anxious patients are more sensitive to pain and are less likely to fully cooperate when receiving an injection which can result in a much lower incidence of success. Mandibular anesthesia requires a significant amount of skill and accuracy which mandates good patient cooperation.
Prior to administering local anaesthetic discuss local anesthesia with the patient to improve cooperation during the injection with respect to opening wide enough, proper tongue position and not moving during the injection.
Anxiety also sensitizes patients to pain and anxious patients react more profoundly to discomfort.12 When it proves difficult to anaesthetize an anxious patient and they feel pain their anxiety increases further compounding the problem. Patients who have experienced difficulty with ineffective local anesthesia in the past often present with a higher than average level of anxiety. This information can be elicited in a thorough dental history.
Needle Gauge
There has been a trend toward using smaller gauge needles for local anesthesia in the belief that a smaller needle will result in less injection pain. Although this has been disproved14 this practice persists.
Needle gauges such as 27 and 30 will easily deflect on entry into tissue thus depositing local anaesthetic in an area that was not intended resulting in anaesthetic inadequacy or failure. When performing a mandibular block the accuracy of the final injection of local anaesthetic solution determines the success of that block. Larger needles such as 25 gauge deflect minimally when injecting producing a higher degree of precision. Using a 25 gauge needle produces no more perceptible pain on injection than a smaller gauge needle yet greatly increases the chances of successful mandibular anesthesia.
In addition 25 gauge needles rarely break during injection while 99% of broken needles are found to be 30 gauge.15
Local Anaesthetic Volume
As mentioned above an adequate volume of local anaesthetic must be present at a sufficient length of the inferior alveolar nerve prior to it’s entry into the mandible in order to provide effective anesthesia. In some cases 1.8 millilitres of local anaesthetic (one cartridge) may not be sufficient to achieve adequate local anesthesia. When a patient presents with a clinical history of inadequate mandibular anesthesia it may be of benefit to use 3.6 millilitres (two cartridges) of local anaesthetic by injecting the patient with the same technique twice.
Local Anaesthetic Agents
Studies have failed to show any significant advantage for one local anaesthetic agent over others with respect to mandibular blocks. Anecdotal reports of the superior effectiveness of articaine over lidocaine in mandibular block anesthesia abound but these are not supported by the literature.16 Articaine is available in a four percent solution which has been shown to increase the risk of neurotoxicity and the long term impairment of sensation after mandibular block injection.17 Other local anaesthetics that are available in higher concentrations such 4% prilocaine solution have also been associated with neurotoxicity while 2% lidocaine appears to have a low risk for neurotoxicity.
When Local Anesthesia Fails: A Systematic Approach
When a mandibular block technique has failed to achieve adequate local anesthesia take the following steps:
- Stop and reassess: Review the patient’s history, has this happened to the patient before during previous dental treatments? If so was successful anesthesia eventually achieved? Can previous treatment records be obtained. What are the results of the extra and intra oral examinations, is there a variance from normal such as an extreme flare of the ramus or a limited interincisal opening?
- When re-injecting, repeating the same technique is unlikely to yield good results. Employ a different technique than the first attempt or modify the same technique to deposit local anaesthetic in a different location (for example use a higher point on the medial aspect of the mandibular ramus). Far better success is achieved by employing a modification of the original technique or by using an alternate mandibular block technique such as the Gow-Gates or Vazirani-Akinosi techniques (see technique section).
- Resist the temptation to use vestibular infiltration or a mental block; this only serves to obscure the signs of a successful mandibular block and rarely results in adequate operative local anesthesia. There are reports of greater success using articaine as opposed to lidocaine for mandibular infiltration in teeth with irreversible pulpitis.18,19 One study on patients with irreversible pulpitis found a success rate for the buccal infiltration of of articaine to be 62% and that for lidocaine 37%. If anesthesia is obtained using infiltration for mandibular molars the duration of pulpal anesthesia can be shorter with limited treatment time.20
- Wait enough time to allow for the block to work. Latency for complete anesthesia of the inferior alveolar nerve has been reported to be as long as 20 to 30 minutes. When a successful block is achieved, record your technique approach in detail in order to repeat local anesthesia for the patient in the future. It is at times useful in difficult cases to draw a diagram of the injection point so that the technique can be repeated at subsequent appointments.
Alternative Techniques
Two alternative approaches which do not require a high degree of skill to master are detailed here both for obtaining adequate mandibular anesthesia both in the event of failure and for regular use to increase overall success rates.
Vazirani-Akinosi Mandibular Block Technique
This technique uses a closed mouth approach with the mandible in a resting position. The advantages of this approach include less need for patient cooperation with respect to opening wide enough for a standard or Gow-Gates mandibular block approach. The use of a closed mouth approach also makes this a preferred method for patients with a strong gag reflex.
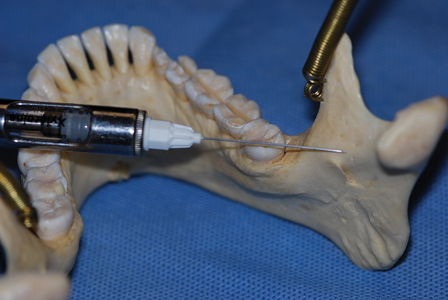
This injection is performed so that local anaesthetic solution is deposited slightly above the area where a standard mandibular block technique would normally deposit local anaesthetic solution (Fig. 6). The third division of the trigeminal nerve has a more consistent course in this area resulting in an improved success rate with the Vazirani-Akinosi technique. With the Vazirani-Akinosi technique the mandibular nerve, buccal, lingual and mylohyoid nerves are anaesthetized.
Fig. 6
Technique
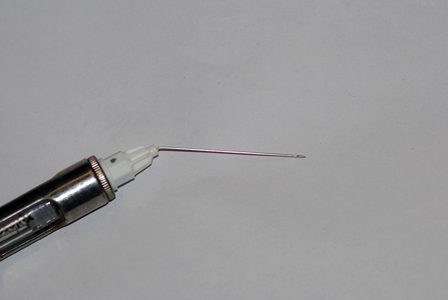
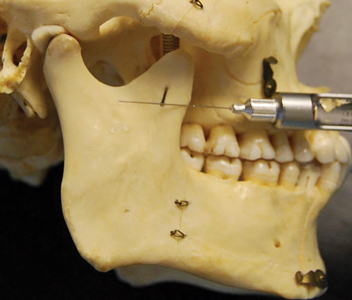
Success with this technique can be improved by placing a small bend in a 25 gauge needle to better access the medial aspect of the mandibular ramus. It is possible to gauge the flare of the ramus of the mandible by extraorally palpating the lower border of the mandible. The angle of the ramus to the midline is the approximate angle the needle should be bent in order to accomplish this injection and this is usually an angle of 10 to 15 degrees (Fig. 7). The needle should be bent at the hub with a firm single action avoiding multiple applications of force which can increase the risk of needle fracture. The needle cap can be used to create the bend which keeps the needle sterile. It is also useful to determine the anterior posterior width of the mandibular ramus as half this distance is the ideal depth of penetration of the needle.
Fig. 7
The patient should keep the teeth in light contact with the masseter muscle relaxed. Clenching will obscure the anatomy and reduces the potential space where local anaesthetic needs to be
deposited.
- Locate the anterior border of the coronoid process, retracting the soft tissue for better visualization. Palpate the anterior and posterior borders of the ramus to determine the midpoint. Using the capped needle extraorally estimate the position of the needle tip at the midpoint of the ramus relative to the upper maxillary molars, this is the depth of insertion required (Fig. 8).
- The point of insertion is parallel to the maxillary occlusal plane at the level of the mucogingival junction of the second maxillary molar. The bend on the needle should be directed laterally toward the ramus with the bevel facing to the midline to aid in deflecting the needle toward the medial aspect of the ramus.
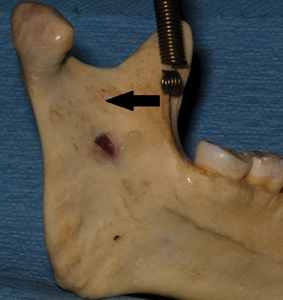
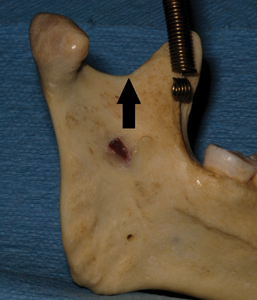
- If bone is contacted during needle insertion it is usually the anterior border of the ramus (Fig. 9) and the needle should be redirected medially by a few millimetres.
- There are no bony landmarks as this injection is in soft tissue only so the depth of insertion is best estimated according to the midpoint of the ramus. In general the hub of a standard long needle (35 millimetres) should be at the mesial aspect of the maxillary second molar. Although it is important to aspirate before injection the incidence of positive aspiration and hematoma is low with this technique.
Fig. 8
Fig. 9
The most common reasons for failure with the Vazirani-Akinosi technique are injecting too far medially thus missing the pterygomandibular space, injecting too high or low by not keeping parallel
to the maxillary occlusal plane and not having the patient relax the masseter and medial pterygoid muscles thus deflecting the needle tip or obscuring the injection point.
The onset and duration of anesthesia with this injection is comparable to that with a standard mandibular block.
High Standard Block Technique
This is a simple technique that requires a slight alteration to the standard mandibular block approach and as such is very easy to employ for increasing success in obtaining mandibular anesthesia.
The advantages of this approach are its ease of use and the deposition of local anaesthetic higher in the pterygomandibular space allowing for better effectiveness of the local anaesthetic.
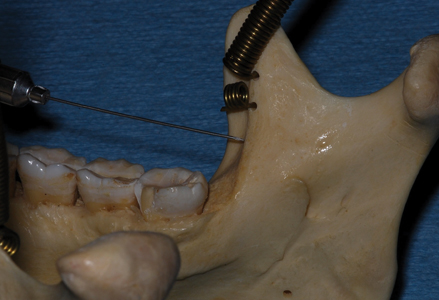
- This technique uses all the same landmarks as a standard mandibular block including the coronoid notch, the contralateral premolars and pterygomandibular raphe. In addition, palpate the mandibular notch intraorally (Fig. 10) to determine the maximum height of injection.
- Similar to the standard mandibular block use the contralateral premolars to determine the angle of insertion of the needle. Instead of injecting local anaesthetic solution at the level of the coronoid notch which is approximately 1.0 centimetre above the mandibular occlusal plane insert the needle so that it contacts the medial aspect of the ramus just below the mandibular notch, a point that is 1.5 to 2.0 centimetres above the mandibular occlusal plane (Fig. 11). This approach has been shown to increase success rates considerably.22
- It is important to aspirate when performing this injection as there are several blood vessels in the region. There should be minimal resistance to injection of local anaesthetic as one is injecting into the potential space of the medial aspect of the mandibular ramus.
Fig. 10
Fig. 11
Onset of anesthesia is similar to that of the standard approach to mandibular block but this technique is more likely to be successful.
Conclusion
Studies have shown that the administration of local anaesthetic injections is stressful for dentists with 18 percent of dentists reporting that this issue caused them to consider a career change.23
Dentist stress during injection is particularly common in mandibular anesthesia due to the precision required for the technique and the ever present possibility of an inadequate mandibular block. Steps taken to improve technique and the rate of success can greatly reduce this stress and create a better experience for patient and dentist alike.
When treating a patient with a history of failed mandibular blocks or when faced with inadequate mandibular anesthesia during treatment a measured simple approach is advocated. Evaluation and reassessment of each individual patient is required at times in order to achieve success.
Paying particular attention to the intra and extra oral anatomy, patient history and patient anxiety can help to improve results. Two alternative techniques are described to help improve outcomes and increase success in obtaining mandibular anesthesia. While there is no one single answer to methods of increasing the success of mandibular local anesthesia there are a number of ways to improve the chances of providing good operative anesthesia.
Oral Health welcomes this original article.
Photographs:
Figures 1, 2, 3: Brian Waters;
Figures 4,5,6,7,8,9,10,11: Sejaan Arora.
References
- Kaufman E, Weinstein P, Milgrom P. Difficulties in achieving local anesthesia. J.A.D.A. 108:205-208, 1984.
- Wong MK, Jacobsen PL. Reasons for local anesthesia failures. J Am Dent Assoc.1992;123(1):69–73.
- Aggarwal V, Singla M, Subbiya A, Viyekanandhan P, Sharma V, Sharma R, Prakash V, Geethapriya N. Effect of preoperative pain on alveolar nerve block. Anesth. Progress 62:135-139, 2015.
- Fleury AA. Local anesthesia failure in endodontic therapy: the acute inflammation factor. Compendium 11: 210-214, 1990.
- Wolf K, Brokaw E, Bell A, Joy A. Variant inferior alveolar nerves and implications for local anesthesia. Anesth. Progress 63:84-90, 2016.
- Raymond SA, Steffenson SC, Gugino LD, Strichartz GR. Anesth. Analg. 1989 May;68(5):563-70.
- Lasemi E, Motamedi MHK, Talaeipour AR, Shafaeifard S, Fard MJK, Navi F, Lasemi R, Zardi Z, Alipanah F. Panoramic Radiographic Relationship of the Mandibular Foramen to the Anterior Border of the Ramus and Occlusal Plane as an Aid in Inferior Alveolar Nerve Block. Anesth Prog. Spring 2019; Vol. 66(1):20-23.
- Watson JE. Appendix: Some anatomic aspects of the Gow-Gates technique for mandibular anaesthesia. Oral Sur Oral Med Oral Path. 1973; 36:328-330.
- Anil A, Peker T, Turgut HB, Gulekon IN, Liman F. Variations in the anatomy of the inferior alveolar nerve. Br. J. Oral Maxillofac Surg. 2003;41:236-239.
- Sillnappa M, Vuori V, Lehtinen R. The mylohyoid nerve and mandibular anesthesia. Int. J. Oral Maxillofac Surg 1988;17:206-207.
- Hargreaves KM, Keiser K, Local anesthetic failure in endodontics: mechanisms and management. Endo Topics. 2002;1:26-39.
- NajjarT. Why can’t you achieve adequate regional anesthesia in the presence of infection? Oral Surg Oral Med Oral Path 1977; 44:7-13.
- Schumacher R, Velden M. Effects of anxiety on experimental pain using SDT. Pain 1981; 7:(Suppl): 512.
- Fuller NP, Menke RA, Meyers WJ,. Perception of pain to three different intraoral penetrations of needles. J.A.D.A. 1979;99:822-824.
- Malamed S, Reed K, Poorsattar S. Needle breakage: incidence and prevention. Dent Clin North Am. 2010; 54: 745-756.
- Brandt RG, Anderson PF, McDonald NJ, Sohn W, Peters MC. The pulpal anesthetic efficacy of articaine versus lidocaine in dentistry: a meta analysis. JADA 2011; 142:493-504.
- Garisto GA, Gaffen AS, Lawrence HP, Tenenbaum HC, Haas DA. JADA 2010;141:836-844.
- Foster W. Drum M, Reader A. Beck M. Anesthetic eficacy of buccal and lingual infiltrations of lidocaine following an inferior alveolar nerve block in mandibular posterior teeth. AnesthProg. 2007; 54:163-169.
- Rogers BS, Botero TM, McDonald NJ, Gardner RJ, Peters MC. Efficacy of Articaine versus Lidocaine as a Supplemental Buccal Infiltration in Mandibular Molars with Irreversible Pulpitis: A Prospective, Randomized, Double-blind Study. J. Of Endo. 2014; (40)6:753–758.
- Robertson D, Nusstein J et al. The anesthetic efficacy of articaine in buccal infiltration of mandibular posterior teeth. JADA 2007;138:1104-1112.
- Agren E, Danielsson K. Conduction block analgesia in the mandible. A comparative investigation of the techniques of fischer and gow-gates. Swed Dent J. 1981;5:81–9.
- Reed KL Advanced techniques of local anesthetic injection. Gen. Dent. 1994;42:248-251.
- Simon JF, Peltier B, Chambers D, Dower J. Quint. October 1994;25(9):641-6.
About the Author
 Dr. Waters is a dental anesthesiologist practicing in Toronto. He is a graduate of the Faculty of Dentistry, University of Toronto and completed his anesthesia residency at Tufts New England Medical Center, Boston.
Dr. Waters is a dental anesthesiologist practicing in Toronto. He is a graduate of the Faculty of Dentistry, University of Toronto and completed his anesthesia residency at Tufts New England Medical Center, Boston.
Don’t forget to sign up to receive the Oral Health Group’s weekly e-newsletter!