Tooth whitening is an integral part of cosmetic dentistry affecting patient satisfaction and profoundly impacting the clinical and business success of the dental practice. There are a multitude of hydrogen peroxide (HP) and carbamide peroxide (CP) based home-care whitening products available that rely on radical oxygen species to alter the tooth color. Unfortunately, they are often used without professional supervision, and these radical oxygen species can cause adverse soft and hard tissues effects such as tooth sensitivity and gum irritation in patients’ mouths. Recently, PAP (phthalimidoperoxycaproic acid) has been developed as an oxidant that avoids these radical oxygen species.
The following article presents a laboratory study that compares the safety (enamel erosion and enamel hardness) and the bleaching effectiveness (shades of color change) of various home-care whitening gels with PAP+ (phthalimidoperoxycaproic acid combined with nano-hydroxyapatite), 6% HP, 35% HP and 35% CP, and how dental professionals can benefit from a PAP+ whitening system.1
Traditional Bleaching Agents
Home-care tooth whitening represents a segment of dentistry where the chemistry has not changed significantly over the last few decades. Some possible negative effects may be better treated, and the patients more prepared to manage their expectations. Marketing techniques have tried to give a sense of clinical evolution, but the main whitening ingredients have remained the same: carbamide peroxide and hydrogen peroxide.
Carbamide peroxide has a buffered chemistry, slowly releasing hydrogen peroxide, making it suitable for overnight treatments for those seeking gradual, sustained whitening.
On the other hand, hydrogen peroxide offers a more immediate whitening effect, acting faster, breaking down stains quickly.
Multiple limitations disrupt the effectiveness of CP and HP in vital tooth bleaching. Prolonged or frequent use may result in oral mucosa irritation, dentinal hypersensitivity, and occasionally, morphological and chemical alterations in the enamel. These alterations can manifest as enamel erosion and decreased surface microhardness.2,3,4 While professional chair-side application techniques using gingival barriers and soft tissue isolation to minimize soft tissue irritation, they are less effective in preventing the detrimental hard tissue effects on enamel.
PAP And Its Mechanism of Action
PAP differs significantly from traditional HP or CP. PAP functions as a non-radical oxygen donor; it breaks down stains on the teeth without releasing potentially harmful free radicals. The chemical structure of PAP enables it to act effectively on extrinsic and intrinsic stains (food, beverages, tobacco, poor dental hygiene, chlorhexidine or cetylpyridinium-based mouthwashes), targeting the staining chromophores within the tooth structure. By breaking these down, PAP whitens the tooth enamel in a way that is both effective and gentle. The process involves epoxidation of molecules containing conjugated double bonds (Fig. 1). This non-radical approach is key to reducing the risk of tooth sensitivity and enamel demineralization.5
Fig. 1
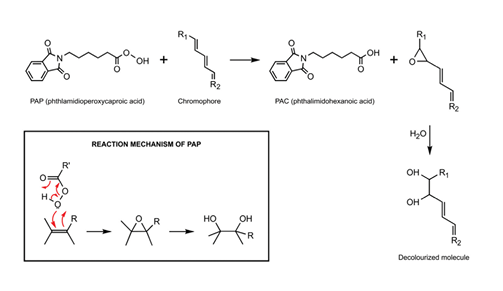
Fig. 2
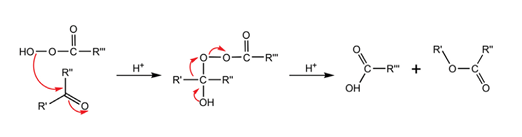
Furthermore, PAP can modify chromogens that cause intrinsic discoloration of vital teeth (stains occurring beneath the tooth surface where particles penetrate the tooth and accumulate within the enamel). For example, PAP interacts with ketones (via a Baeyer-Villiger oxidation reaction) to remove intrinsic stains.
Results of a Laboratory Study Comparing PAP+ Vs HP And CP
A 2017 study by Pascolutti & de Oliveira was a double-blind, placebo-controlled clinical trial that demonstrated significant bleaching effects after a single treatment, with no dental hypersensitivity or oral mucosal irritation.1 The study investigated the effectiveness and safety of a new PAP+ bleaching gel. This exploration was conducted through in vitro tests, which were designed to evaluate the potential for enamel erosion, the impact on surface microhardness, and the overall bleaching efficacy of the gel.
Safety: Enamel Erosion
The impact of six applications of bleaching gels, each lasting 10 minutes, on enamel erosion exhibited two different trends. No enamel erosion was observed with 35% CP and PAP+ treatments. In contrast, enamel surface loss due to erosion, identified as step defects, was noted in four out of the six samples in both the 6% HP and 35% HP group.
Safety: Hardness of the Enamel
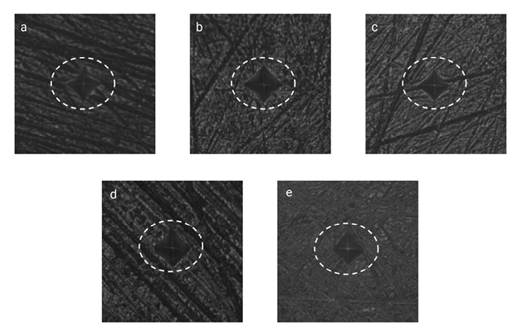
The analysis of microhardness after six 10-minute treatments revealed two distinct outcomes. In the case of the PAP group, there was an increase in Vickers surface microhardness (SMH) post-treatment (12.9 ± 11.7), a change significantly distinct from the other three groups (P < 0.001). Conversely, all three commercial bleaching products resulted in decreased surface microhardness. The 35% HP gel showed the most substantial reduction (−94.28 ± 27.09), followed by 6% HP (−62.22 ± 19.52) and then 35% CP (−55.3 ± 24.6), with the latter two showing no significant difference from each other. Figure 3 presents examples of baseline and post-treatment SMH VK indents for the four different types of treatments.
Fig. 3
Bleaching Effectiveness
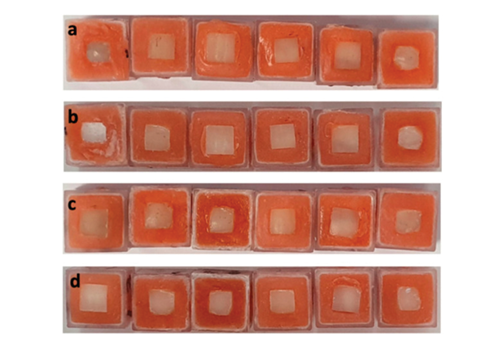
The 6% HP gel, serving as a positive control, resulted in a change of 4.86 ± 2.32 in shade guide units (DSGU), while the innovative PAP+ gel led to a more significant improvement of 8.13 ± 2.82, a difference that was statistically substantial (with a two-tailed p-value of 0.0110). All datasets followed Gaussian distributions. Upon comparison, the effectiveness of PAP+ exceeded that of 6% HP by 70%. This implies that six 10-minute treatments using 6% HP are required to achieve the same bleaching effect as two 10-minute applications of PAP+ gel. Figure 4 illustrates the whitening results achieved by these various treatments. Furthermore, see figure 7A and 7B for a before and after clinical case which indicates the shade improvement benefits of using tooth bleaching protocol over 14 days (Fig. 7).
Fig. 4
How Dental Professionals Can Benefit from a PAP+ Whitening System
Integrating PAP+ whitening gels (Figs. 5, 6) into dental practices offers several significant advantages:
1. PAP+’s safety profile makes it suitable for a broader range of patients, including those who might have been hesitant about teeth whitening due to concerns about sensitivity. This inclusivity can help expand the patient base for cosmetic dental services, making it more appealing to both dentists and patients.
2. The inclusion of hydroxyapatite and potassium citrate in PAP+ are essential to maintain a near-neutral pH during treatment and preserve the enamel surface.7
3. The ease of application of PAP+-based products.
4. Reduced risk of side effects.
Fig. 5

Fig. 6

As patient comfort and safety are paramount in dental treatments, PAP+ aligns perfectly with these priorities, increasing patient satisfaction and repeat business. This can enhance the competitive edge of a dental practice. In an industry where patients are increasingly informed and selective about their dental care options, practices that provide innovative, patient-friendly solutions are likely to stand out.
Fig. 7A

Fig. 7B

PAP+ Benefits
A recent breakthrough in home-care whitening, phthalimidoperoxycaproic acid (PAP), is revolutionizing home whitening comfort, offering superior safety and effectiveness.
The highlighted laboratory studies reveal that PAP+ tooth whitening gel does not cause enamel erosion or decreased surface microhardness, which is notably different from the enamel softening and degradation observed with Hydrogen Peroxide and Carbamide Peroxide bleaching gels. PAP+ gel’s efficacy in destaining polyphenol stains is clearly superior when compared to a 6% HP gel. PAP+ gel applications were able to whiten the tooth shade by about eight shades, according to the VITA® Bleachedguide scale. 
Oral Health welcomes this original article.
References
- Pascolutti, M.; de Oliveira, D. A Radical-Free Approach to Teeth Whitening. Dent. J. 2021, 9, 148. https://doi.org/10.3390/dj9120148
- Rodríguez-Martínez J., Valiente M., Sánchez-Martín M.J. Tooth whitening: From the established treatments to novel approaches to prevent side effects. J. Esthet. Rest. Dent. 2019;31:431–440. doi: 10.1111/jerd.12519.
- Tredwin C.J., Naik S., Lewis N.J., Scully C. Hydrogen peroxide tooth-whitening (bleaching) products: Review of adverse effects and safety issues. Br. Dent. J. 2006;200:371–376. doi: 10.1038/sj.bdj.4813423.
- Sulieman M.A.M. An overview of tooth-bleaching techniques: Chemistry, safety and efficacy. Periodontology 2000. 2008;48:148–169. doi: 10.1111/j.1600-0757.2008.00258.x.
- Kwon, S.R.; Wertz, P.W. Review of the mechanism of tooth whitening. J. Esthet. Rest. Dent. 2015, 27, 240–257. [CrossRef]
- Bizhang, M.; Domin, J.; Danesh, G.; Zimmer, S. Effectiveness of a new non-hydrogen peroxide bleaching agent after single use—A double-blind placebo-controlled short-term study. J. Appl. Oral Sci. 2017, 25, 575–584.
- Rodrigues, F.T.; Serro, A.P.; Polido, M.; Ramalho, A.; Figueiredo-Pina, C.G. Effect of bleaching teeth with hydrogen peroxide on the morphology, hydrophilicity, and mechanical and tribological properties of the enamel. Wear 2017, 374–375, 21–28.
About the Author

Martha Szczepulski is a professional educator with 19 years of dental hygiene practice. She is experienced in general and community dental practices, dental hygiene education, and mobile dental hygiene in long term care. Martha is the Professional Education Leader for Oral Science. Her vision is to help clinicians create a synergy between evidence-based practice and common sense practicality that is uncomplicated and implementable.