Introduction
Looking at online forums that discuss dental implants, one cannot help but notice a heavy emphasis on the surgical aspect of implant prosthodontics with the prosthodontic phase often overlooked or barely discussed. It is our opinion that this line of thinking often results in multiple (sometimes unnecessary) surgical procedures that may yield outcomes that are more expensive, take a longer time to complete and are not necessarily always patient friendly. We feel very strongly that the provision of dental implants for our patients is a prosthodontic solution with a surgical component, emphasizing the importance of prosthetically determined surgical placement.
The intent of this article is to present two case histories where the definitive prosthodontic plan dictated the surgical protocol. It highlights that proper planning and the use of today’s available technology, allows clinicians to provide efficient, non-invasive, retrievable and predictable results. We recognize that some of the ideas presented in this article will illicit some debate and encourage our readers to keep an open mind.
Clinical Cases
Case #1
The first patient, a 56-year-old healthy female, was referred to our practice for the management of her fractured and decayed tooth #24. Upon clinical examination, this tooth was determined to be nonrestorable owing to its lack of ferrule. The patient was not interested in any heroic attempts to salvage this tooth. The removal of tooth # 24 and replacement with a dental implant was recommended.
A small field cone beam CT scan was obtained to examine the surrounding anatomical limitations (especially the sinus), plan the final prosthodontic outcome and determine the surgical plan that would be required. In the authors’ opinion, this planning approach allows the clinician to determine the most efficient, non-invasive and predictable approach for the patient’s treatment.
The results of this scan demonstrated that the apex of tooth #24 was positioned approximately 2 mm away from the floor of the sinus. However, palatal bone of adequate thickness (5 mm) was noted medial to the sinus. NobelClinician™ software was used to plan the intended position of the implant and the intended final abutment for the definitive restoration on that implant. As depicted in Figure 2, the implant was planned with an intentional palatal orientation that would allow for a screw-retained, angulated-screw channel® definitive restoration (25 degrees of angle correction are possible). This plan would allow for predictable implant primary stability at the time of extraction, increasing the likelihood that an immediate provisional restoration could be placed and reducing the need for surgical involvement of the sinus floor.
Fig. 1

Fig. 2
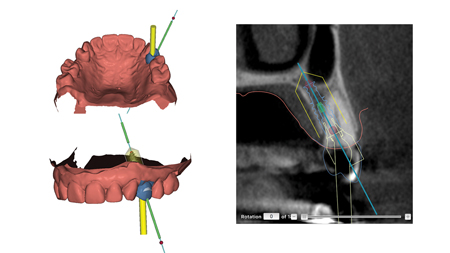
represents the long axis of the planned implant. The yellow line represents the prescribed 25-degree correction of the screw access channel for the planned restoration (blue).
The surgical procedure was carried out exactly as planned using a tooth-supported, printed, guided surgical stent, NobelGuide.™ The following procedure was carried out: Tooth #24 was atraumatically removed without raising a mucoperiosteal flap. The surgical guide was placed and complete seating was confirmed. A sequential drilling protocol with copious irrigation was used to place a NobelActive 4.3 x 11.5 mm RP implant at the prescribed position and depth. The primary stability achieved was between 35 and 70 Ncm. Particulate osseous allograft (RAPTOS, citagenix) was placed in the surrounding vacant extraction socket. A radiolucent, nylon, temporary cylinder was used to pick-up a prefabricated transitional restoration made of Radica (Dentsply) composite. The cervical contours of the transitional restoration were created with a flowable composite restoration and highly polished on a dental lathe with a soft ragwheel and a progressively finer pumice slurry. The temporary restoration was immediately placed, but completely relieved from occlusion. Of course, there was an expected access hole on the buccal aspect of the crown that was closed with protective polytetrafluoroethylene (Teflon) tape and composite. A single 4-0 chromic gut sutured was placed with the simple interrupted technique. The procedure ran smoothly without any surgical complications (Fig. 3).
Fig. 3

Note the use of a radiolucent nylon cylinder for the transitional restoration. The facial access hole is also not very apparent because it was closed with a composite restoration.
After a healing period of four months, the patient returned for the assessment of osseointegration and to initiate the definitive prosthodontic phase of care. The implant was asymptomatic, immobile and there was radiographic evidence of an intact bone-implant interface. Resonance frequency analysis (Penguin™) was also carried out and the measured implant stability quotient was 70. With osseointegration confirmed, an open-tray, PVS impression was taken, along with an opposing alginate impression, a PVS interocclusal record and the shade was selected. As planned prior to surgery, the case was sent to the dental lab (Image Dental Laboratory, Barrie, ON) for the fabrication of a full-contour zirconia crown with an angulated screw channel abutment (ASC) with 25-degree correction. This design would allow the final crown to be screw-retained despite the palatal angulation of the implant. The design was then sent to the NobelProcera milling facility for manufacturing (Fig. 4).
Fig. 4
At the next visit, the transitional restoration was removed and the definitive restoration was inserted. The contours, interproximal contacts, occlusal contacts required only minor adjustment. The abutment screw was torqued to 35 Ncm and the access channel was closed with telfon tape and composite. The patient was pleased with the overall feel and appearance of the restoration (Fig. 5).
Fig. 5

Case #2
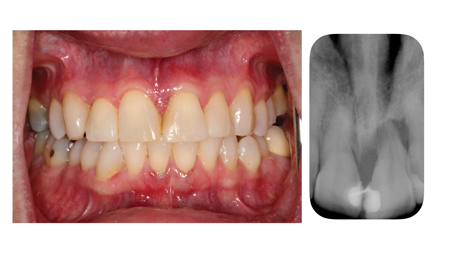
The second patient, a 64-year-old healthy female, was referred to our practice for the management of her severely periodontal compromised tooth 21. Upon clinical examination, this tooth was vital but had class III mobility. It was splinted to the adjacent central incisor and there was granulation tissue in the midline papilla, extending lingually (Fig. 6). Based on its clinical presentation, its long-term prognosis was guarded/hopeless and therefore, its removal and replacement with a dental implant was recommended.
Fig. 6
Similarily to the first case, a small field cone beam CT scan was obtained to investigate the anatomical limitations (especially the floor of the nose) and plan the prosthodontic-surgical procedure.
The results of this scan demonstrated complete destruction of the buccal plate and a proximity of the apex to the floor of the nose. However, thick palatal bone was also noted. Once again, NobelClinician™ software was used to plan the intended position of the implant and the intended final abutment for the definitive restoration. As depicted in Figure 7, the implant was planned with an intentional palatal orientation that would allow for a screw-retained, angulated-screw channel® definitive restoration. This plan would increase the likelihood of achieving implant primary stability at the time of extraction and thereby allowing for an immediate provisional restoration.
Fig. 7
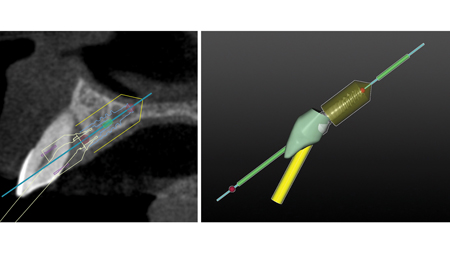
The surgical procedure was carried out exactly as planned using a tooth-supported, printed, guided surgical stent, NobelGuide.™ The following procedure was carried out: Tooth #21 was atraumatically removed without raising a mucoperiosteal flap. The surgical guide was placed and complete seating was confirmed. A sequential drilling protocol with copious irrigation was used to place a NobelActive 3.5 x 11.5 mm NP implant at the prescribed position and depth. The primary stability achieved was greater than 35 Ncm. Particulate osseous allograft (RAPTOS, citagenix) was placed in the surrounding vacant extraction socket. A prefabricated PMMA provisional restoration designed in the NobelClinician software, named TempShell™ was used to pick-up a temporary nylon sleeve. The cervical contours of the transitional restoration were created and highly polished. The temporary restoration was immediately placed, but completely relieved from occlusion. Again, just as with the previous case, there was an expected access hole on the buccal aspect of the crown that was closed with Teflon tape and composite resin (Fig. 8).
Fig. 8

After a healing period of four months, the patient returned for the prosthodontic phase of treatment. The implant was asymptomatic, immobile and there was radiographic evidence of an intact bone-implant interface. Resonance frequency analysis (Penguin™) was also carried out and the measured implant stability quotient was 65. Most interestingly, despite the absence of a buccal plate and a severe pre-operative bone defect, the soft tissues were well preserved. However, the loss of the granulation tissue from the midline papilla did result in a small midline “black triangle” (Fig. 9).
Fig. 9

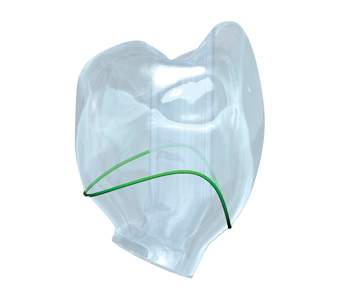
With osseointegration confirmed, an open-tray, PVS impression was taken (Fig. 10). As planned prior to surgery, the case was sent to IDL (Image Dental Laboratory, Barrie, ON) for the fabrication an implant crown made using the angulated screw channel abutment (ASC) with 25-degree correction. In this case, due to the aesthetic demands of the anterior zone, a zirconia abutment was made with an overlying lithium disilicate (e-max, Ivoclar) crown that had a lingual access hole to maintain screw-retention. The abutment was manufactured with NobelProcera and the crown was milled at IDL (Fig. 11).
Fig. 10

Fig. 11

At the next visit, the transitional restoration was removed and the definitive restoration was inserted. The contours, interproximal contacts, occlusal contacts required only minor adjustment. The e-max crown was extra-orally cemented with resin cement and the crown was seated and torqued to 35 Ncm. The access channel was closed with Teflon tape and composite. The patient was pleased with the overall feel and appearance of the restoration (Fig. 6).
Discussion
These two case histories describe the management of two non-restorable teeth that were replaced with implant-retained restorations. The implant prosthodontic protocols highlighted here differ from the traditional approach of tooth replacement. Historically, these patients would have been managed with a stage-wise approach involving multiple procedures including:
1. Extraction with ridge preservation
2. Possible soft tissue augmentation
3. Implant placement with possible sinus augmentation (one or two-stage)
4. Delayed healing with a removable appliance
5. Definitive restoration with a cemented restoration
The solutions provided for these patients were conducted in an efficient, accurate, non-invasive and retrievable fashion by making use of new technologies and concepts, including:
1. Atraumatic extraction with immediate implant placement
2. Computer guided implant placement with strategic angulation to circumvent anatomical structures while providing primary stability and avoiding the need for grafting procedures
3. Immediate provisionalization for
a. Optimal soft tissue shape and contour
b. Soft tissue tenting in the absence of a bony buccal plate
c. Patient convenience and comfort during the healing phase
4. Prosthetic design for longevity, retrievability and aesthetics
Conclusion
The case histories presented in this article underscore the importance of prosthetically-driven implant treatment. They were chosen to illustrate that a planned prosthodontic result can actually dictate the steps involved for the surgical intervention. Digital diagnostic and planning tools like NobelClinician™ and design innovations like the Angulated Screw Channel abutment, can be strategically used to provide safe, predictable, effective and efficient implant treatment. OH
Oral Health welcomes this original article.
Acknowledgement
We would like to thank the laboratory support from Image Dental Laboratory in Barrie, Ontario. We would also like to thank Dr. Steven Bongard for championing the importance of the patient experience.
References
- Chen ST, Wilson TG Jr, Hämmerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19 Suppl:12-25. Review.
- Chen ST, Buser D. Clinical and Aesthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009;24 Suppl:186-217
- Funato A, Salama MA, Ishikawa T, Garber DA, Salama H. Timing, positioning, and sequential staging in Aesthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007 Aug;27(4):313-23
About the Authors
 Dr. David Powell received his DMD degree from McGill University in 2011 and then completed a General Practice Residency at the Jewish General Hospital in Montreal. After practicing as a general dentist at the same hospital for a year, he pursued his Prosthodontics specialty training and Masters of Sciences at the University of Toronto. He currently practices at Barrie Dental Specialists and is a member of the prosthodontics division at Chrysalis Dental Implant Centres. He is also a lecturer and assistant professor of Prosthodontics at University of Toronto. In addition, he is a fellow of the Royal College
of Dentists of Canada, member of the Association of Prosthodontists of Canada and member of the American College of Prosthodontists.
Dr. David Powell received his DMD degree from McGill University in 2011 and then completed a General Practice Residency at the Jewish General Hospital in Montreal. After practicing as a general dentist at the same hospital for a year, he pursued his Prosthodontics specialty training and Masters of Sciences at the University of Toronto. He currently practices at Barrie Dental Specialists and is a member of the prosthodontics division at Chrysalis Dental Implant Centres. He is also a lecturer and assistant professor of Prosthodontics at University of Toronto. In addition, he is a fellow of the Royal College
of Dentists of Canada, member of the Association of Prosthodontists of Canada and member of the American College of Prosthodontists.
 Dr. John P. Zarb earned his DDS at the University of Detroit Mercy in 1995. Upon graduation, he completed a one year General Practice Residency at the VA Hospital in Ann Arbor, MI, followed by graduate prosthodontic training at the University of Toronto, earning his MSc in 2002. Dr. Zarb is a staff prosthodontist in the Graduate Prosthodontic Department at the University of Toronto and at Mt Sinai Hospital in Toronto, and a Clinical Assistant Professor at the University of Rochester, Eastman Institute for Oral Health. He has been involved with surgical and prosthetic implant
Dr. John P. Zarb earned his DDS at the University of Detroit Mercy in 1995. Upon graduation, he completed a one year General Practice Residency at the VA Hospital in Ann Arbor, MI, followed by graduate prosthodontic training at the University of Toronto, earning his MSc in 2002. Dr. Zarb is a staff prosthodontist in the Graduate Prosthodontic Department at the University of Toronto and at Mt Sinai Hospital in Toronto, and a Clinical Assistant Professor at the University of Rochester, Eastman Institute for Oral Health. He has been involved with surgical and prosthetic implant
dentistry education at both the undergraduate and graduate level. Dr. Zarb joined Barrie Dental Specialists in 2003. He is a Fellow and examiner of the Royal College of Dentists of Canada, a Fellow in the Academy of Dentistry International, and Fellow in the Academy of Prosthodontics and a former Director of the American College of Prosthodontists.
 Dr. Steven Bongard obtained his DDS degree from The University of Toronto Faculty of Dentistry in 1986. He is the founder and clinical head of Chrysalis Dental Centre in Toronto, a dental implant only facility focused on “same day” dental implant solutions. Dr. Bongard has extensive experience in implant placement, bone grafting procedures, as well as the prosthetic component of implant restoration. He has published and lectured both nationally and internationally on implant placement, All-on-4®, “Guided” implant surgery, single tooth, and alternative implant solutions. Clinically, his recent focus has been on developing innovative implant solutions for predictable same-day treatment of the severely atrophic edentulous patient as well as integrating the digital work flow into everyday implant prosthodontics.
Dr. Steven Bongard obtained his DDS degree from The University of Toronto Faculty of Dentistry in 1986. He is the founder and clinical head of Chrysalis Dental Centre in Toronto, a dental implant only facility focused on “same day” dental implant solutions. Dr. Bongard has extensive experience in implant placement, bone grafting procedures, as well as the prosthetic component of implant restoration. He has published and lectured both nationally and internationally on implant placement, All-on-4®, “Guided” implant surgery, single tooth, and alternative implant solutions. Clinically, his recent focus has been on developing innovative implant solutions for predictable same-day treatment of the severely atrophic edentulous patient as well as integrating the digital work flow into everyday implant prosthodontics.












