Background:
Hypohidrotic ectodermal dysplasia (HED) is a genetic condition characterized by abnormal development of two or more structures of the ectoderm. HED is the most common form of ectodermal dysplasia, and is characterised by the cardinal features of hypohidrosis (due to hypoplasia of sweat glands), hypotrichosis (sparseness of scalp and body hair) and oligodontia. Four genes account for 90% of HED cases: heterozygous mutations in EDA, EDAR, EDARADD or WNT10A. These three forms of HED alter the same signal transduction pathway and have been correlated with certain dental phenotypes like conical teeth and specific craniofacial traits, whereas mutations in WNT10A usually display no facial dysmorphisms.1,2
As many of these patients present oligodontia (absence of 6 or more teeth) or anodontia (complete absence of teeth), prosthetic rehabilitation is usually desirable. Regardless of age, removable full, partial or overdentures present a frequently applied treatment modality in children. Many international consensus conferences have addressed the management of ectodermal dysplasia (ED) and the use of dental implants. These patients usually present a decrease of alveolar bone volume and alveolar ridge tapering due to congenitally missing teeth.3-5
The purpose of this report is to describe the prosthodontic treatment of an 18-year-old male patient diagnosed with HED who presented with oligodontia.
Case report
An 18-year-old male with diagnosis of HED presented for consultation at our office with the chief complaint of wanting to replace his existing dentures. He had completed orthodontic treatment a few years back to reposition his maxillary teeth. (Figs. 1A & 1B). Physical examination revealed sparsely distributed hair, dry skin, and frontal bossing of the skull. It was established that nobody in the family had a similar condition. The patient came to the consultation appointment accompanied by his parents. Aside from his diagnosis of HED his past medical history was non-significant. He denied taking any medications or having any drug allergies. At the time of consultation he lived with his parents and attended last year of high school.
Fig. 1A

Fig. 1B

There was complete anodontia in the mandible; however, the maxilla had teeth 16,13,11,21,23, and 26 present. (Figs. 2A-2E). He had been treated with a maxillary transitional denture and a mandibular complete denture. (Fig. 3) Teeth 11 and 21 had all ceramic crowns placed 2 years before the consultation appointment, by his dentist. Residual ridge in the mandible was severely resorbed and there was severe bucco-lingual deficiency in the maxillary edentulous regions.
Fig. 2A
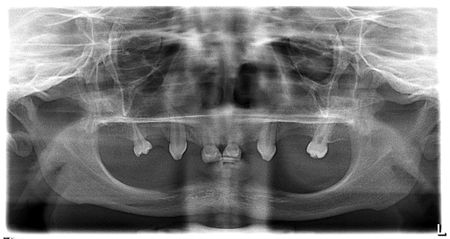
Fig. 2B

Fig. 2C

Fig. 2D

Fig. 2E
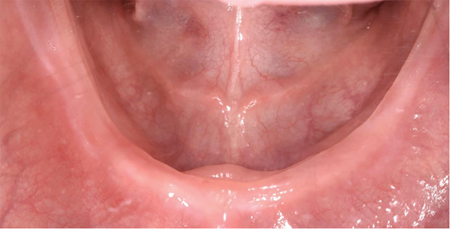
Fig. 3

Despite the severe ridge resorption in the mandibular arch, he was able to wear his complete denture with no problems. His previous dentist and orthodontist discussed the possibility of implants and it was decided to wait until he had completed his growth. The patient’s records from his dentist were forwarded to our office and we had a second consultation with his parents and the patient and presented with a few prosthodontic options for him. For the mandibular arch the options discussed were: 1) placement of 5 or 6 implants and fabrication of a mandibular fixed complete denture; 2) placement of 4 implants and fabrication of a bar-retained overdenture (BOD); 3) placement of 4 implants and fabrication of an overdenture with direct attachments. For the maxillary arch, we discussed the options of: 1) single crowns on all remaining teeth and fabrication of a removable partial denture (RPD), 2) single crowns for remaining teeth and replacing of missing teeth with dental implants and implant retained crowns, 3) RPD only, 4) fixed partial dentures. We discussed all the advantages and disadvantages of each option, including esthetics, comfort, additional surgical procedures such as bone grafting, cost and long term maintenance and possible complications.
The patient and parents decided that the best treatment for him would be full coverage restorations for the maxillary dentition and a RPD to replace missing teeth; and for the mandibular arch, he would have an overdenture retained by a bar overdenture.
All consent forms were reviewed and signed by the patient. A referral was sent to an oral surgeon for assessment and implant placement in the mandibular arch. Since the position of the teeth in his mandibular denture were in an appropriate position, we duplicated it in order to fabricate a surgical guide.
Four 4.1 mm X 12 mm (Straumann, RN Tissue level, SLActive) implants were placed in the mandible, anterior to the mental foramen. (Figs. 4A & 4B) His existing mandibular prosthesis was relined and used by the patient while implants osseo-integrated.
Fig. 4A
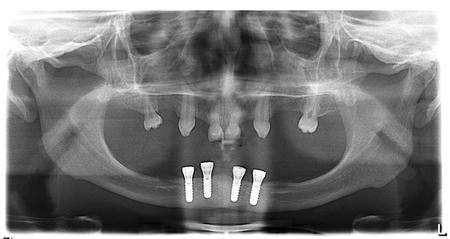
Fig. 4B

Once the implants were integrated, we proceeded to the restorative portion of the treatment.
First, all maxillary teeth were prepared in order to receive full coverage restorations. (Fig. 5) Using a template from a diagnostic wax up, we fabricate temporary restorations for his maxillary teeth. Three temporary fixed partial dentures (TFPD) were fabricated using composite material (Integrity, Dentsply Sirona). The first TFPD spanned from tooth 13 to 16, the second TFPD joined teeth 23 and 26; and the third TFPD joined teeth 11 and 21 with distal cantilevers for teeth 12 and 22. (Fig. 6) Proper occlusal and incisal planes were determined using conventional methods. Tooth length and angulation of anterior teeth were determined using speech and patient’s preferences. Provisional restorations were assessed when the patient smiled and when his lips were at rest. (Figs. 7A & 7B) Once the patient was satisfied with the maxillary interim restorations, the mandibular prosthesis was adjusted accordingly for proper occlusion.
Fig. 5

Fig. 6

Fig. 7A

Fig. 7B

Four abutments (Straumann, RN synOcta Abutments) were torqued to 35Ncm onto implants and an abutment level open-tray impression was taken using a custom tray. (Figs. 8A & 8B) Before taking impressions, all impressions posts (RN Impression posts for open tray, abutment level, synOcta) were splinted together with light-cured acrylic to maximize accuracy of the impression. A final impression of the maxillary arch was taken using a custom tray, where we captured all hard and soft tissues in order to fabricate all crowns and the RPD. Both impressions were taken using additional silicone material (Aquasil, Dentsply-Sirona). The mandibular master cast was used to fabricate a wax rim which was used to determine the proper vertical dimension of occlusion (VDO). The interocclusal record was recorded against the maxillary TFPD. During the following appointment, a wax try-in was done and the desired shade and teeth mould was verified with the patient. Also, during this wax try-in appointment, interocclusal records were taken between the maxillary prepared teeth and the mandibular teeth set in wax in order to maintain the already established VDO. First, we removed the TFPD of his right side, maintaining the other TFPD, and a rigid material was used to record the maxillomandibular relation. Then, the left TFPD was removed and a second record was taken for the left side, after we repositioned the right interocclusal record. Lastly, the anterior TFPD was removed and a third record was taken of the anterior segment after we repositioned the other 2 records. (Fig. 9) This technique maintains established VDO with the provisionals at all times.
Fig. 8A

Fig. 8B
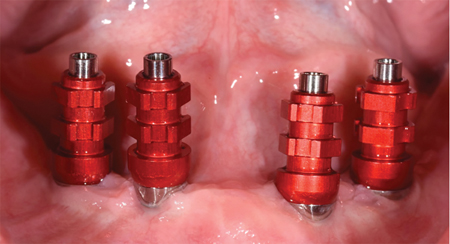
Fig. 9

The case was sent to the laboratory for completion, giving details in terms of crowns design and RPD design. The design for the maxillary RPD consisted of an anteroposterior palatal strap and cingulum rests on teeth 11,21,13,23; and ball attachments on mesio-occlusal of 13 and 23 and disto-occlusal of 16 and 26. The porcelain fused to metal crowns for 13 and 23 had ball abutments of the distal aspect and for 16 and 26 on the mesial aspect.
During the delivery appointment, all crowns were tried on to ensure marginal fit and ensure proper alignment with the RPD components. Then, the crowns were luted using glass ionomer cement (GC FujiCEM 2, GC). The RPD was seated onto the maxillary arch while the luting agent was setting. Then, the RPD was removed and the excess cement was removed.
We then moved on to mandibular arch: the healing caps were removed from abutments, and the Dolder bar was torqued to 15 Ncm onto abutments, and the overdenture was seated. Occlusion was checked and minor adjustments in occlusion were done. (Figs. 10A-10E). A panoramic radiograph was taken at the end of the treatment. (Fig. 11) The patient was very happy with the final result, and he practiced how to remove and insert both prosthesis. He had no issues during the follow-up appointment and he was placed on a 6-month recall visit.
Fig. 10A

Fig. 10B
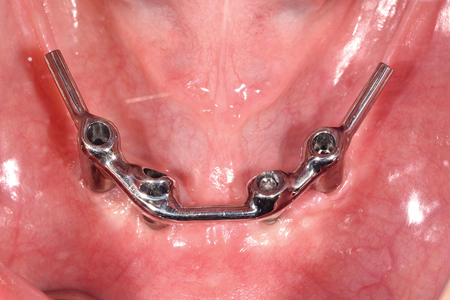
Fig. 10C
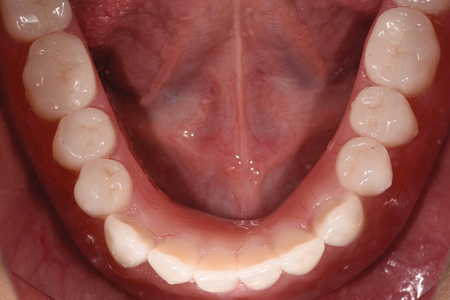
Fig. 10D

Fig. 10E

Fig. 11

The quality of life of this patient was greatly improved as both prostheses were more esthetic and had more retention. The patient was always able to eat foods of different consistencies with his removable dentures, however he was definitely able to notice a significant improvement with his new prosthesis. At the end of the treatment, he was pursuing post-secondary education and working part time at a restaurant. His treatment was briefly interrupted during the closure of dental offices in Ontario from March to June of 2020.
Discussion:
The degree of dentoalveolar tissue deficiency can make an implant-supported prosthesis an appropriate method of definitive occlusal restoration in patients with HED. However, as the absence of teeth is congenital, this raises the issue of placement of oral implants in growing children, due to the influence of craniofacial growth on the implant’s behavior.3,4,6 The oral rehabilitation of patients with implants is generally delayed until the cessation of growth because an implant does not exhibit dentoalveolar adaptation in response to vertical alveolar growth or local bony remodeling as would occur in the case of a tooth. However, the use of removable dentures in the deficient residual basal bone structures usually observed in individuals with HED could be a cause of functional and psychological problems. Moreover, the salivary gland hypoplasia in HED patients typically leads to mucosal drying, which can cause poor removable denture retention and make it difficult for children to use removable dentures. Therefore, the use of dental implants before the cessation of growth in HED patients is encouraged by some dentists.6-8
When there is anodontia in the mandibular arch implants can be placed at an early age to improve retention and function. Implant survival has been reported for up to 26 years, on implants placed in early childhood.6 In an oligodont adult individual, implants are frequently placed, as most patients desire a comfortable, palate-free fixed or removable restoration. Bone augmentation in atrophic alveolar regions is thereby necessary in most cases. Primary or permanent teeth considered of little prosthetic value may be extracted and replaced in the course of rehabilitation by means of implants. Since this patient showed consistent attendance comprising oral hygiene, denture adaptation and renewal during the years, the treatment described in this article has an excellent prognosis.9
The dental team for patients with ED should include a general/paediatric/restorative dentist, a prosthodontist and an orthodontist. Other experts like oral and maxillofacial surgeons and speech therapists may be consulted. Treatment goals should be determined according to the patients’ age and demands. Treatment decisions, such as the indication of pre-prosthodontic orthodontic alignment of teeth, orthognathic surgery, time of dental implant placement, should be made interactively. Long term care and maintenance of patients with ED is a must and should provide a good prognosis.1,2,9
Oral Health welcomes this original article.
References
- Schnabl D, Gerhard S, Biederman R, Crismani A, Rasse M, Zauza K, Schmuth M, Kapferer-Seebacher I. Dental Management and Prosthetic Rehabilitation of Patients Suffering from Hypohidrotic Ectodermal Dysplasia: A Report of Two Case Histories. Int J Prosthodont. 2018 November/December;31(6):552-557.
- Schnabl D, Gruert I, Schmuth M, Kapferer-Seebacher I. Prosthetic rehabilitation of patients with hypohidrotic ectodermal dysplasia: A systematic review. J Oral Rehabil. 2018 Jul;45(7):555-570.
- Kramer FJ, Baethge C, Tschernitschek H. Implants in children with ectodermal dysplasia: a case report and literature review. Clin Oral Implants Res. 2007 Feb;18(1):140-6.
- Yap, AK, Klingberg I. Dental implants in patients with ectodermal dysplasia and tooth agenesis: a critical review of the literature. Int J Prosthodont. 2009 May-Jun;22(3):268-76.
- Chrcanvic BR. Dental implants in patients with ectodermal dysplasia: A systematic review. J Craniomaxillofac Surg. 2018 Aug;46(8):1211-1217
- Wang Y, He, Decker AM, Hu JC, Zou D. Clinical outcomes of implant therapy in ectodermal dysplasia patients: a systematic review. Int J Oral Maxillofac Surg. 2016 Aug;45(8):1035-43.
- Omondi BI, Chepkony F, Ariemba RM, Miyogo JO, Opinya GN. Prosthodontic Rehabilitation of a Child with Ectodermal Dysplasia: A Preliminary Report. It J Prosthodont. 2019 Jan/Feb;32(1):107-109.
- Knobloch LA, Larsen PE, Saponaro PC, L’Homee-Langlois E. Early implant placement for a patient with ectodermal dysplasia: Thirteen years of clinical care. J Prosthet Dent. 2018 May;119(5):702-709.
- Torres CP, Dos Reis AC, Queiroz AM, Stuani MB, Mira P, Ferreira PS, Gomes-Silva JM, Ramos ES, Huber J, Borsatto MC. Oral Rehabilitation of a Child with Hypohidrotic Ectodermal Dysplasia. J Dent Child (Chic). 2019 Sep 15;86(3):158-163.
About the Author
 Dr. Aragon is a Prosthodontist who maintains a full-time private practice in London, Canada. She is an Adjunct Clinical Professor at the Schulich School of Dentistry and a Lecturer at the Graduate Prosthodontics Program at the University of Toronto. She holds clinical privileges at the London Health Science Centre. She is a Diplomate of the American Board of Prosthodontics. E-mail: doctor@aragonprosthodontics.com – www.aragonprosthodontics.com
Dr. Aragon is a Prosthodontist who maintains a full-time private practice in London, Canada. She is an Adjunct Clinical Professor at the Schulich School of Dentistry and a Lecturer at the Graduate Prosthodontics Program at the University of Toronto. She holds clinical privileges at the London Health Science Centre. She is a Diplomate of the American Board of Prosthodontics. E-mail: doctor@aragonprosthodontics.com – www.aragonprosthodontics.com
To read more articles from the 2020 Prosthodontic issue of Oral Health, please click here.












