
Rehabilitation of the aesthetic zone with dental implants is a widespread technique in dentistry. However, when a single central incisor is involved, numerous surgical and prosthetic protocols have been described to achieve a long-lasting aesthetic result that resembles the contralateral incisor.1 In many cases, replacing a single tooth on the aesthetic front is much more complicated than restoring the entire sector, as achieving a natural-looking emergence of the prosthesis and making the final aesthetics of the restoration blend in with the rest of the teeth is a task of the utmost complexity.2-3 For the maintenance of the soft tissue, many protocols have described the technique of immediate post-extraction implant with connective grafts and immediate provisionalization to ensure that the initial contour of the extracted tooth is maintained in the restoration. On other occasions, the decision to extract the tooth and allow the soft tissue to heal, resulting in a higher percentage of keratinized gingiva and inserting an early implant, also yields good long-term aesthetic results.4-5 Nowadays, there is significant controversy in the choice of these two protocols, with publications on both ensuring a better aesthetic result and maintenance of hard and soft tissues over time.5-7
The use of transepithelial components to make single-tooth prostheses is an innovative approach that allows us to achieve a correct seal and prosthetic-implant fit, moving the critical junction point to a more coronal area, leaving more space for the soft tissues and thus allowing less gingival retraction due to compression or bacterial filtration.8-9 When we combine the use of a single transepithelial unit with the help of interfaces for the prosthesis fabrication, we improve the fit of the restoration and reduce the possible dimensional changes of repeatedly placing the crown in the furnace.10-13 The interface is an intermediate piece that joins the crown to the transepithelial component and acts as an isolated, micro-milled element with an excellent passive fit, which allows cold cementing to the final restoration to achieve a screw-retained crown without distortion due to fabrication.10-13 These interfaces can be of different thicknesses and heights to suit other clinical cases with different gingival thicknesses (Figs. 1 and 2). In the following clinical case, we show the resolution of an implant in the aesthetic sector through the use of a single transepithelial component and an interface that allows the creation of an individualized emergence profile by the clinical situation, moving the critical point of the implant-prosthesis junction away from the juxta-gingival area, as well as the step-by-step work with the interfaces.
Fig. 1
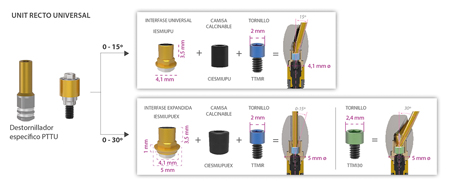
Fig. 2

Clinical case
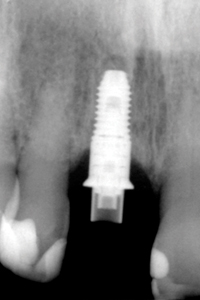
We present the case of a 60-year-old male patient who came to our clinic requesting treatment for tooth 11. He had been in pain for several days, with mobility and suppuration through the sulcus, which led us to suspect the presence of a fracture in this tooth. We decided to carry out a dental cone beam to confirm our initial diagnosis (Figs. 3-5).
Fig. 3

Fig. 4
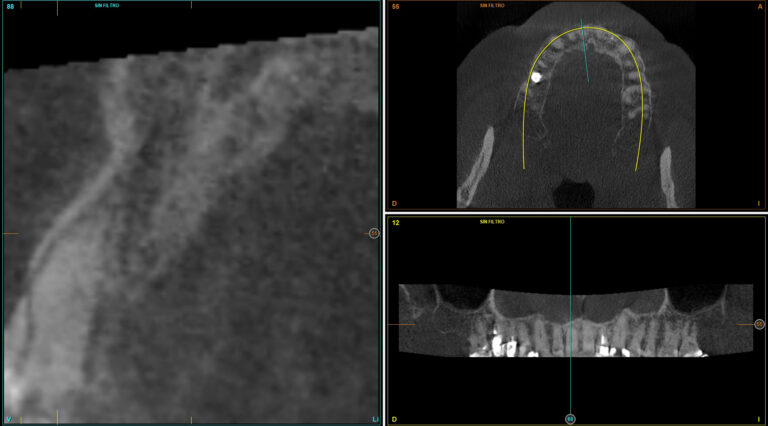
Fig. 5

Given the findings of the cone beam, it was decided to extract the fractured tooth and regenerate the alveolus with PRGF-Endoret (Biotechnology Institute) to achieve an increase in the soft tissue and partial healing of the hard tissue and to be able to carry out an early insertion implant eight weeks after tooth extraction. Once the tooth has been extracted and with a better starting point for the soft tissue, a new diagnostic cone beam is performed (Figs. 6-8). In the images, we can see a regeneration of the alveolus and a residual bone ridge of sufficient height and width for the direct insertion of an implant. It is decided that the length of the implant should be 8.5 mm.
Fig. 6

Fig. 7

Fig. 8

At the time of implant insertion, it was decided to carry out immediate loading to gradually shape the soft tissues and generate a progressive load on the bone. This is possible due to the excellent quality of the bone bed and the stability achieved with the implant at the time of surgery (35 Ncm). For this purpose, a transepithelial unit is placed at the time of insertion (Fig. 9), which will later be used for the definitive prosthesis. In this way, we ensure a tight implant-prosthesis seal from the beginning and a soft tissue union through the hemidesmosomes that will favour the maintenance of the gingival margin and the surrounding soft tissues. Once the surgery is completed, we take the impression directly on the transepithelial component and generate a working model for the crown fabrication. The crown will be made using an interface, which will be placed juxta-gingivally to leave the critical prosthesis-implant junction at a point away from the implant connection and with less bacterial penetration (Fig. 10). On this interface, we carry out the diagnostic wax-up, and through the wax-up, we make a provisional acrylic crown that will be cemented to the interface once it is finished. This way, the interphase-abutment connection is preserved intact, generating fewer errors (Figs. 11-13).
Fig. 9
Fig. 10A

Fig. 10B
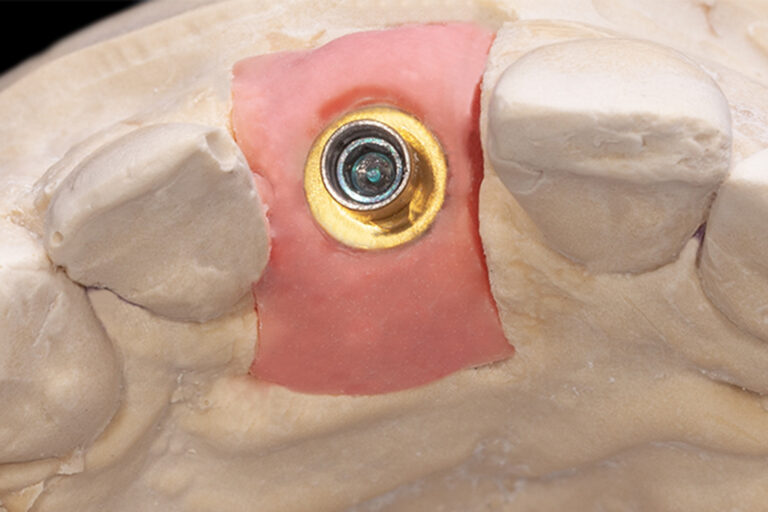
Fig. 11
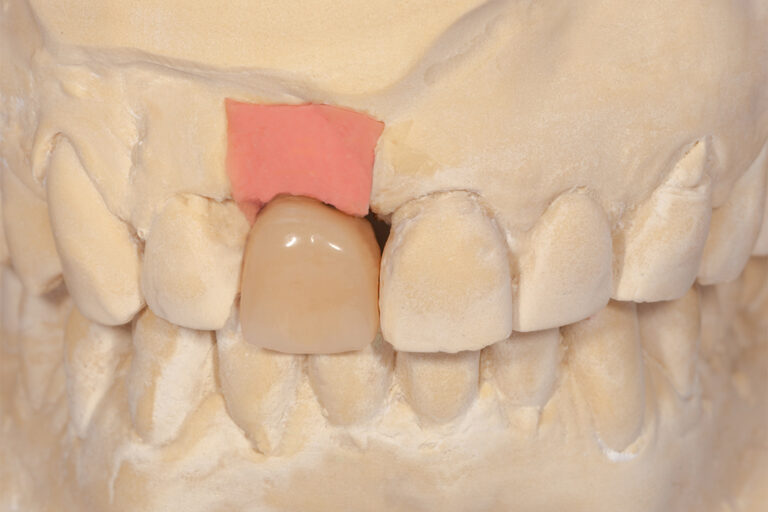
Fig. 12

Fig. 13
The final prosthesis is made three months after implant placement and immediate loading. The soft tissues are stable at this point, and the impression is retaken on the same transepithelial without being removed (Fig. 14). The case is finished with a ceramic crown (Emax) cemented to a new interface on the same transepithelial component. Ceramic veneers are placed on the adjacent teeth to achieve harmony of the anterior front and to improve the aesthetics of the composite reconstructions that were present with pigmentation and misaligned margins (Figs. 15 and 16). The patient attended regular follow-up visits at one month, three months, six months and one year after the insertion of the implant and the final crown, and then once a year. None of the follow-up visits showed any problems in the bone bed or the gingival margin of the implant-supported restoration. At five years, we can observe the complete stability of the treatment (Figs. 17-21).
Fig. 14

Fig. 15

Fig. 16
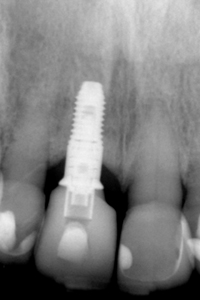
Fig. 17

Fig. 18
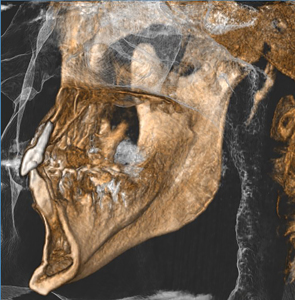
Fig. 19

Fig. 20

Fig. 21

Discussion
In single-unit implant rehabilitation in the aesthetic sector, prosthetic components that allow good soft tissue adaptation can make a difference, especially in the long term.1-2 In addition, achieving an implant-prosthesis seal and not replacing the transepithelial component to preserve the soft tissue attachment through the gingival hemidesmosomes can also be a differentiating factor, as in the case we have shown. A systematic review with meta-analysis analyzing immediate loading protocols according to the type of restoration used found no statistically significant differences between the different types of prostheses used (fixed, removable, provisional, and definitive). However, more substantial increases in ISQ values were found in the follow-up of patients with immediate loading when the prostheses were definitive, which seems to indicate that not removing the prosthesis favours not only the sealing and good behaviour of the soft tissues but also the integration of the immediately loaded implant.14 The use of transepithelial component may achieve an effect similar to that reported in the meta-analysis mentioned above, preventing soft tissue breakdown in the transepithelial-implant area, extending soft tissue stability, and favouring implant integration without vestibular defects. The use of interfaces has also been studied by our study group in single and multiple implants, obtaining good results, reducing the errors of direct-to-implant measurements and the distortions of several entries in the furnace of the component that will finally be screwed in, creating discrepancies and micro-gaps when there are multiple thermocycling cycles.11-13
Conclusion
Rehabilitation of a central incisor can be carried out in a protocol of early deferred implantation, immediate loading and immediate provisionalization with unitary transepithelial and use of interfaces with successful treatment both aesthetically and in terms of crestal bone maintenance, as we have shown in this clinical case.
Oral Health welcomes this original article.
References
- Kan JYK, Rungcharassaeng K, Deflorian M, Weinstein T, Wang HL, Testori T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol 2000. 2018 Jun;77(1):197-212.
- Testori T, Weinstein T, Scutellà F, Wang HL, Zucchelli G. Implant placement in the esthetic area: criteria for positioning single and multiple implants. Periodontol 2000. 2018 Jun;77(1):176-196.
- Gomez-Meda R, Esquivel J, Blatz MB. The esthetic biological contour concept for implant restoration emergence profile design. J Esthet Restor Dent. 2021 Jan;33(1):173-184.
- Arora H, Ivanovski S. Clinical and aesthetic outcomes of immediately placed single-tooth implants with immediate vs. delayed restoration in the anterior maxilla: A retrospective cohort study. Clin Oral Implants Res. 2018 Mar;29(3):346-352.
- Chochlidakis KM, Geminiani A, Papaspyridakos P, Singh N, Ercoli C, Chen CJ. Buccal bone thickness around single dental implants in the maxillary esthetic zone. Quintessence Int. 2017;48(4):295-308.
- Hassani A, Hassani M, Bitaraf T. Immediate vs Delayed Restorations of Immediately Placed Single Implants in the Anterior Maxilla: A Nonrandomized Clinical Study. Int J Oral Maxillofac Implants. 2021 Nov-Dec;36(6):1159-1164.
- Schropp L, Isidor F, Kostopoulos L, Wenzel A. Patient experience of, and satisfaction with, delayed-immediate vs. delayed single-tooth implant placement. Clin Oral Implants Res. 2004 Aug;15(4):498-503.
- Hernández-Marcos G, Hernández-Herrera M, Anitua E. Marginal Bone Loss Around Short Dental Implants Restored at Implant Level and with Transmucosal Abutment: A Retrospective Study. Int J Oral Maxillofac Implants. 2018 Nov/Dec;33(6):1362-1367.
- Steflik DE. Optimizing soft tissue consistencies around transepithelial abutments. Dent Implantol Update. 1992 Feb;3(2):9-12.
- Anitua E, Alkhraisat MH. Single-unit short dental implants. Would they survive a long period of service? Br J Oral Maxillofac Surg. 2019 May;57(4):387-388.
- Anitua E. Immediate Loading of Short Implants in Posterior Maxillae: Case Series. Acta Stomatol Croat. 2017 Jun;51(2):157-162.
- Anitua E, Piñas L, Escuer-Artero V, Fernández RS, Alkhraisat MH. Short dental implants in patients with oral lichen planus: a long-term follow-up. Br J Oral Maxillofac Surg. 2018 Apr;56(3):216-220.
- Anitua E, Alkhraisat MH. Clinical Performance of Short Dental Implants Supporting Single Crown Restoration in the Molar-Premolar Region: Cement Versus Screw Retention. Int J Oral Maxillofac Implants. 2019 July/August;34(4):969–976.
- Sanz-Sánchez I, Sanz-Martín I, Figuero E, Sanz M. Clinical efficacy of immediate implant loading protocols compared to conventional loading depending on the type of the restoration: a systematic review. Clin. Oral Impl. Res. 2015;26:964–982.
About the Author

Dr. Eduardo Anitua is the Director of the Eduardo Anitua Institute and the Scientific Director of the BTI (Biotechnology Institute). He received his MD (Medicine and Surgery) from the University of Salamanca in 1979. Stomatology Specialist at the University of the Basque Country, he continued his studies in the United States and Europe. He has spoken at conferences at several universities and post-graduate programs and has given over 500 courses and conferences on implants, prostheses, dental aesthetics, and tissue regeneration at conferences in Europe, the United States, South America, and Asia.









