Tetracycline (TC) stained teeth are considered a side effect of high doses of TC antibiotics during permanent tooth formation.1 The problem is more common among people in their late 50s to early 70s who were born and raised in decades when TC antibiotics were most frequently used.2 Tetracycline-stained teeth have been classified by Feinman and by Jordan and Boksman, who reported on the whitening of tetracycline-stained teeth in 1984.3 It is important to correctly classify stained teeth before beginning the treatment protocol, as higher degrees of staining increase the complexity of treatment, from minimally invasive treatment to invasive full-coverage crowns.3 Feinman suggests whitening in 1° and 2° staining cases, while whitening is contraindicated in 3° and 4° cases.4 Jordan and Boksman on the other hand, argue that 1° to 3° staining classifications can be expected to benefit from bleaching, and to first suggesting whitening to the patient.5 Whitening is also the safest method of changing tooth color while preserving tooth structure, and in the case of tetracycline-stained teeth, the typical treatment time is estimated to be 1-12 months, with an average of 3-4 months. In some cases, whitening alone is successful, and it has been reported that whitening prior to veneer and/or crown restoration can help to manage the severely discoloured TC stained teeth.
In recent years, with the growth of minimally invasive concepts of dentistry and improvements in destaining agents, whitening is increasingly being used prior to laminated veneer and crown restorations involving tooth cutting, including Feinman’s 3° and 4° classifications.6 Some patients, faced with the choice of placing veneers on all their teeth, have begun to choose to use whitening only, even with higher degrees of staining. The aim is not to achieve perfect whiteness, but rather to secure some degree of esthetic improvement while preserving the patient’s functional teeth.
While it is relatively straightforward to place veneers on all teeth and make them white, it is much more difficult to handle cases in which the patient wants veneers on only some teeth and prefers non-invasive treatment on the remainder. In such cases, pure white veneers would create an unpleasant contrast with the other teeth and, thus, make the esthetics worse rather than better. However, creating veneers that match the colors and color gradations of tetracycline-stained teeth is not easy, as the colors are not uniform across the surface of the stained teeth. The situation is further complicated if the teeth have previously been treated and some of the tooth material removed, as this makes treatment options more involved.
Read: Laser Debonding of Ceramic Restorations
The following case reports the esthetic improvement by home whitening with 6% hydrogen peroxide (HP) followed by veneer restoration on 3° tetracycline-stained teeth (Feinman and Jordan and Boksman’s classification).
Case report
A 54-year-old woman presented at the Esthetic Dentistry Clinic of the Aichi-Gakuin University Dental Hospital, with the main complaint of wanting to whiten her teeth. Direct resin-based composite veneer procedures on teeth #12 to 22 had been completed at age 18 (Fig. 1), and these veneers showed significant wear and discoloration, with the particularly obvious discoloration of air bubbles in the veneer. Examination showed that all the patient’s maxillary teeth had 3° tetracycline staining. The placement of veneers from 15 to 25 and 35 to 45 was suggested, but the patient preferred treatment with less tooth structure removal and asked for the existing veneers on 12 to 22 be replaced, and the appearance of the other teeth to be improved as much as possible without invasive surgery. It was decided to home whiten all teeth with 6% HP dispensed in prefilled trays (Opalescence Go, Ultradent Products, USA), followed by ceramic veneer restoration on teeth 12 to 22.
Fig. 1

After scaling and mechanical tooth cleaning and prior to home whitening, the color was measured using a dental spectrophotometer (Rayplicker, Borea, France). The results showed that the maxillary right canine was C3 and the mandibular right central incisor was C4. Home whitening was performed for 90 minutes per day for 10 days. At the end of the whitening, the shade was C2 on the maxillary right canine and C3 on the mandibular right central incisor (Fig. 2).
Fig. 2

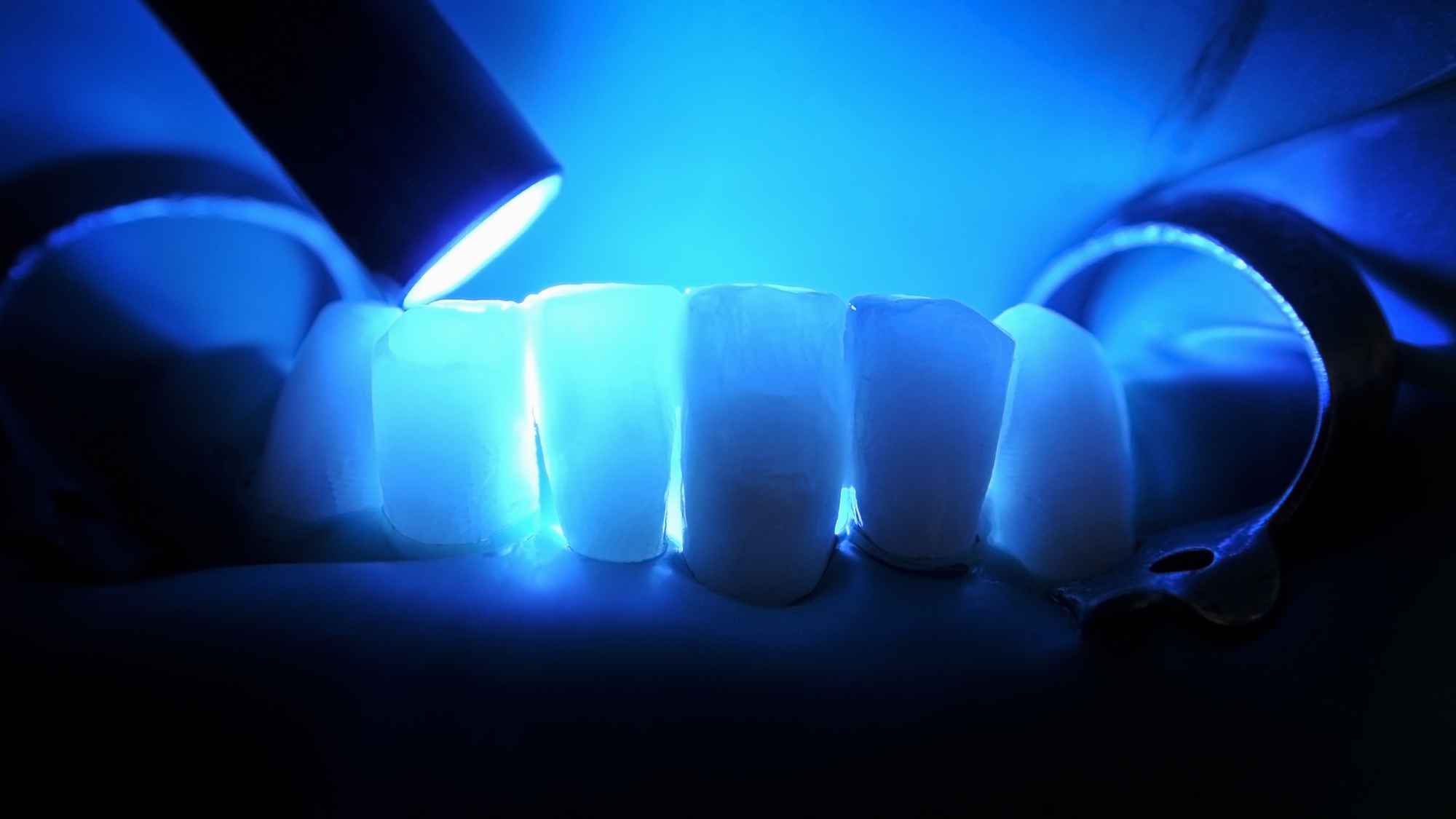
For the veneer restoration, a diagnostic wax-up was made (Fig. 3), and then the old restorations of the maxillary central and lateral incisors were removed under rubber-dam (Fig. 4) and flowable resin-based composite (Filtek Supreme Ultra Flowable Restorative, Solventum, USA) was used to build-up the teeth before preparation, followed by final formation (Fig. 5). A precise impression was taken while checking the amount of abutment tooth removal using a silicone guide. For the fabrication of the final restoration, IPS e.max Press (Ivoclar Vivadent, Liechtenstein), a lithium-disilicate-reinforced pressed ceramic, was used and laminated veneers were fabricated according to the manufacturer’s instructions. After the working model was made by injecting high-hardness dental stone into the impression taken, IPS model sealer (Ivoclar Vivadent) was applied to harden the plaster model surface and protect the abutment tooth models. Two layers of spacer were applied at a maximum distance of 1 mm from the margin. After adjustment of the working model, wax-up was performed and sprues were implanted in the wax pattern using the IPS e.max investment ring system. The wax up was then implanted in mold material (IPS Press VEST Premium, Ivoclar Vivadent) and left for 30 minutes before being placed in a furnace. The mold was heated at 850°C and for 45 min, in accordance with the guidelines for IPS Press VEST Premium rapid heating. After wax incineration, an IPS e.max press ingot was inserted into the ring, set in the center of the press furnace and pressed. After cooling the ring, the mold was abraded away with glass beads at 4 and 2 bar. To remove the reaction layer formed during pressing, Invex Liquid treatment was carried out for 10 minutes, after which the reaction layer was blasted with alumina at 1 to 2 bar. After these processes were completed, the sprues were cut and morphology corrected. The restorations were blasted with alumina at 1 atm to remove any contamination from the surface and cleaned under running water. Finally, staining and firing were repeated several times to ensure that the translucency and color of the veneers would match the appearance of the surrounding tetracycline-stained teeth when in place. The restoration was completed by glazing (IPS e.max Ceram Glaze Spray, Ivoclar Vivadent) and firing (Fig. 6). The final restorations were tested with try-in paste to confirm their esthetic properties. The patient was satisfied with the color tone and morphology, so after pre-treatment of the abutment and restoration under rubber-dam, the laminate veneers were placed using a light-cure resin luting cement (Panavia Veneer LC, Kuraray Noritake Dental, Japan) (Fig.7). At 14 months after surgery the laminate veneers were in good condition (Fig. 8).
Fig. 3

Fig. 4

Fig. 5

Fig. 6

Fig. 7

Fig. 8

Conclusion
Laminated veneer restorations together with home whitening using 6% HP can improve the esthetics of even severely tetracycline-stained teeth. Although it was difficult to uniformly whiten the entire crown of the severely tetracycline-stained teeth by whitening alone, bleaching was found to have a significant clinical effect, including stripe reduction, in some areas. In addition, the use of translucent ceramics as the material for the laminate veneers enabled a natural appearance while retaining the color of the underlying tetracycline teeth. No problems were found 14 months after treatment. It is suggested that in the treatment of severely tetracycline-stained teeth, whitening followed by restorative or prosthetic procedures may lead to acceptable esthetic results with minimal intervention. 
Oral Health welcomes this original article.
References
- Billings RJ, Berkowitz RJ, Watson G. Teeth. Pediatrics 2004; 113: 1120–1127.
- Tigecycline-induced tooth discoloration in children younger than eight years. Antimicrob Agents Chemother. 2021; 65(9): e0085421.
- Jordan RE, Boksman L. Conservative Vital bleaching treatment of discoloured dentition. Compend Contin Educ Dent 1984; 5(10): 803-805.
- Newsome PR, Linda H. Management of tetracycline discoloured teeth. Aes Dent Today 2008; 2:15-20.
- Bloomquist RF, Sword RJ, Londono J, Haywood VB. Bleaching: the initial treatment consideration for tetracycline-stained teeth. Br Dent J 2021; 230(12): 807-12.
- Botelho MG, Chan AWK, Newsome PRH, McGrath CP, Lam WYH. A randomized controlled trial of home bleaching of tetracycline-stained teeth. J Dent 2017; 67:29-35.
About the authors

Dr. Mayumi Maesako, Assistant Professor of Operative Dentistry, Aichi Gakuin University School of Dentistry, Nagoya, Japan, with a clinical practice emphasizing minimally invasive esthetic dentistry. Recipient, Board Certifications, Japanese Society of Conservative Dentistry and Japan Academy of Esthetic Dentistry.

Dt. Yu Kitamura, Adjunct Lecturer, Institute of Dental Technology, Aichi Gakuin University, Nagoya, Japan. His clinical practice emphasizes minimally invasive esthetic dentistry. A Founder, Citta Eterna and Member, Society of Japan Clinical Dentistry.

Dr. Akimasa “Aki” Tsujimoto, Professor and Chair, Operative Dentistry, Aichi Gakuin University School of Dentistry, Nagoya, Japan. Earned DDS and PhD, and was a tenured Professor, Nihon University, Japan. Visiting Professor at Creighton University NE and University of Iowa IA.