This article is the fifth in a series by the author submitted to and published in Oral Health. The previous four articles of the series were published in the August 2015 to 2018 issues with the titles: Surgical Risk Factors in Implant Dentistry: Influence on Failures and Bone Loss1, Patient Related Systemic Risk Factors2, Patient Related Local Risk Factors3 and Operator Related Risk Factors.4 This fifth article will cover unrestorable implants, which include risk factors in the third and fourth categories (Table I) and will illustrate representative cases from the author’s practice that demonstrate various case types with unrestorable implants.
Table I

Perhaps the two most common complications resulting in the inability to restore dental implants are implant malposition and fractures of the implant or abutment (see Table II). See Tables III and IV which summarize implant fracture etiological risk factors and implant material flexural strength respectively. Many implants today are made with more fracture resistant type IV titanium that is cold-worked and an improved titanium alloy uses zirconium for even further strength. When confronted with an unrestorable implant, a strategic decision needs to be made as to whether to remove or “bury” the implant. This decision primarily depends on the planned remediation of the case but can be influenced by several other factors such as the risk and trauma of removing the implant, and the patient’s preferences when several options are available. This article will review some of the situations resulting in unrestorable implants as well as their treatment, and will include several clinical examples from the author’s private practice.
Table II

Table III
Table IV

Data from American Society for Testing and Materials (AST International Standards)
* The stress at which the material is changed in shape due to permanent strain
** The maximum stress that a material can withstand before failure in tension
Unrestorable implants-etiology and treatment: implant malposition: oro-facially
Implant malposition in the oro-facial dimension and particularly being too far facially inclined in the maxilla, may be the most common operator related risk factor (anecdotal). These implants potentially can have an increased incidence of biological complications such as bone loss, implant loss, esthetic and prosthetic complications and may not be restorable. See Figures 1A, 1B and 1C for a case where the implant was positioned too far to the facial and could not be restored in an acceptable fashion. To remediate the case, and in order to avoid the trauma of removing the osseointegrated implant, a decision was made to “bury” the implant and restore the edentulous area with a fixed bonded restoration. The patient declined alternate treatments, including removing the implant, grafting and placing another implant.
Fig. 1A
Fig. 1B

Fig. 1C

Sometimes an implant is placed too far to the facial but a decision is made to restore it, but only with patient informed consent, knowing to expect a compromised result. See Figures 2A, 2B and 2C for a case where the consequences of a labially inclined implant position, resulted in a long clinical crown with the definitive restoration. The patient had a low lip line and was prepared to accept the compromised esthetic result.
Fig. 2A
Fig 2

Fig. 3

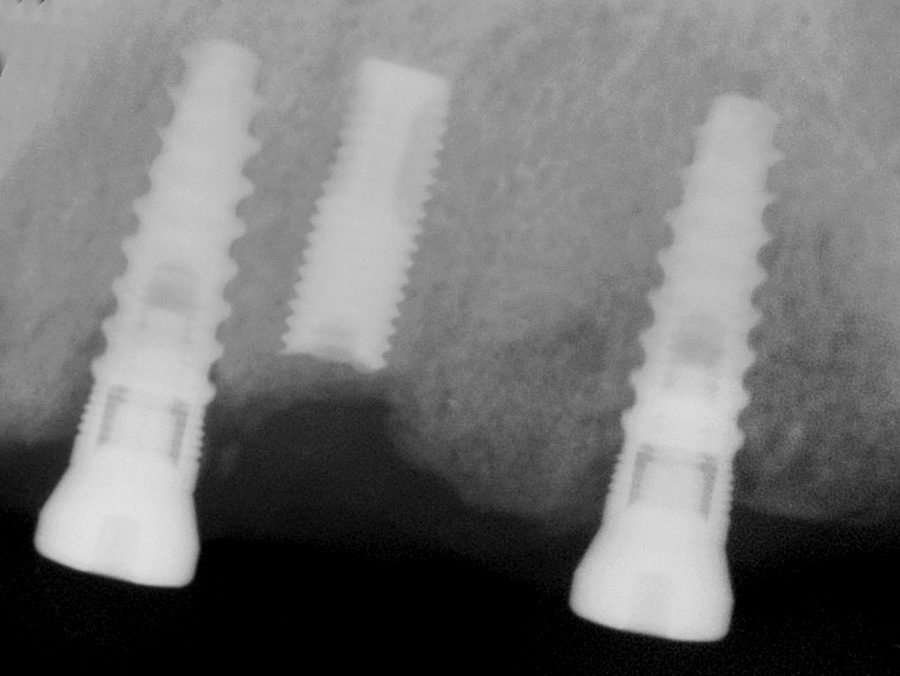
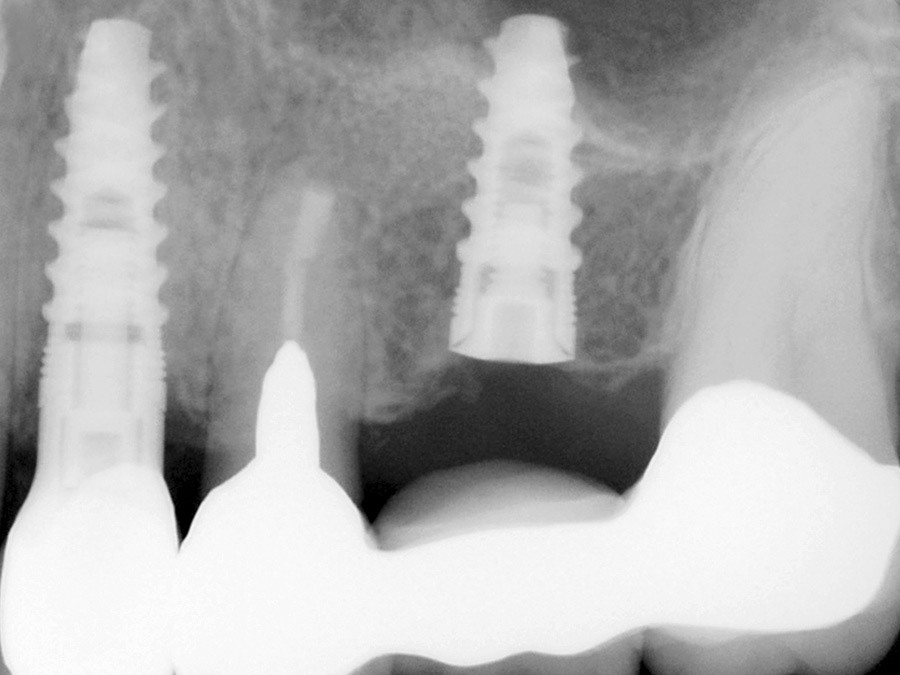
Implant malposition: mesio-distally
In the mesio-distal dimension, implants in too close a proximity to each other may result in increased risk of recession, bone loss, lack of an interproximal papilla5,6 and may not be restorable. See Figure 3A for a case referred for management where three adjacent implants were too close such that all three could not be included in the restoration. The initial rationale in placing three implants was to compensate for the short implants that were required. In hindsight it would have been better to leave out the middle implant. To remediate the case and to avoid the trauma of removing the osseointegrated implant, a decision was made to leave the middle implant unrestored. In some less severe cases, implants are restored despite being in too close proximity. See Figure 3B where the mesio-distal proximity of the two implants resulted in poor interproximal crown contours.
Fig. 3A

Fig. 3B
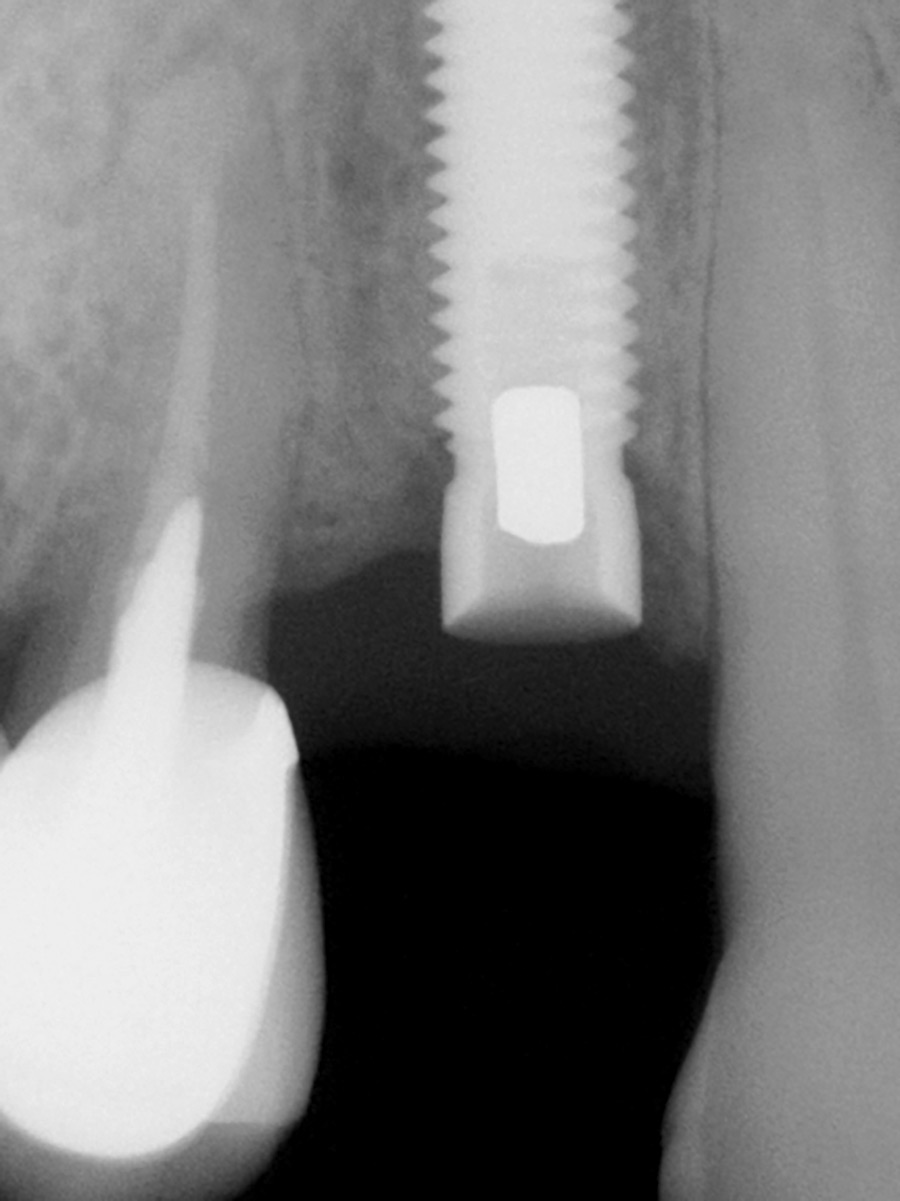
Implant malposition: apico-occlusally
In the apico-coronal dimension, an implant placed too deeply may result in more difficult prosthetic management and deeper periodontal pockets (Figs. 4A & 4B). At the other extreme an implant placed too superficially may not allow sufficient vertical space for a well contoured restoration and may result in a ridge lap design that is not ideal for oral hygiene (anecdotal). See the case in Figures 5A, 5B and 5C where limited vertical space apically (in order to avoid bone perforation) and limited vertical space coronally (due to the limited available occlusal clearance) necessitated the use of a short implant as well as a very short clinical crown restoration. Also see Figures 6A to 6D for a case referred to the office for management that were restored with a ridge lap due to a reduced vertical clearance. In situations with even less clearance, the case may be unrestorable due to minimum space requirements for the prosthetic components and materials. A guideline may be a minimum of 5 mm and 7 mm of occlusal clearance for screw and cement retained restorations respectively (anecdotal).
Fig. 4A

Fig. 4B

Fig. 5A
Fig. 5B

Fig. 5C

Fig. 6A

Fig. 6B

Fig. 6C

Fig. 6D

Abutment Fracture: screw retained
In most cases, fractured screw retained abutments can be retrieved and there are several kits on the market designed for this. If the residual fractured abutment is not removed, it renders the implant unrestorable. See Figures 7A and 7B for a case of a 90-year-old patient, where the previously placed fractured screw retained abutment was not removed. The patient was undergoing additional implant placements for a planned overdenture implant restoration and in part due to this, the implant with the abutment fracture was less strategic. To simplify the treatment and avoid the trauma of removing the implant, a decision was made to “bury” this implant and place additional implants both mesially and distally.
Fig. 7A

Fig. 7B
Abutment Fracture: Cement retained
In all if not almost all contemporary implant restorations, definitive abutments are NOT cemented into the implant. However, in the 1980’s with some implant systems, it was common practice to utilize either cemented or screw retained abutment options. When abutments were cemented, they were typically fabricated with a non-precious metal for strength and “permanently” cemented. On occasion abutment fractures still occurred and then presented the problem of not being able to simply remove the residual cemented fractured abutment. Attempts at drilling out the fragment and restoring the case resulted in significant compromised results at best (personal experience). As a consequence, often these implants were “buried” rendering them unrestorable or the implants were removed and alternate options considered (Figs. 8A & 8B).
Fig. 8A

Fig. 8B
Implant Subcrestal Fracture
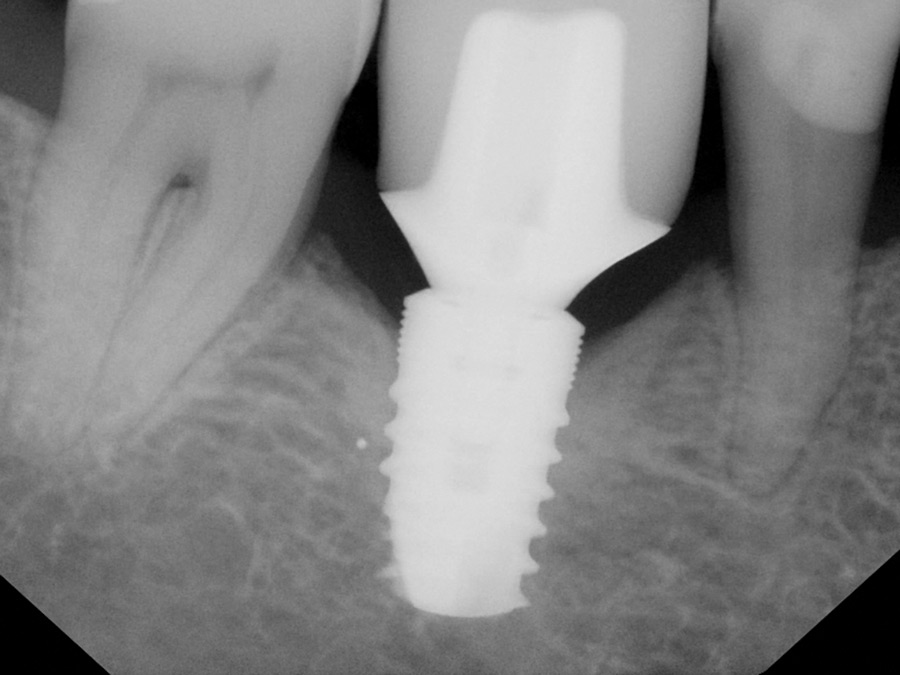
Fractures of the implant body are not as common as they used to be (personal experience). In the 1980’s implants were often manufactured with Grade I pure titanium while contemporary implant materials are typically Grade II, IV or V. Grade I is the weakest strength of all the titanium grades (see Table IV) and was likely an important factor accounting for their 5% or more fractures in posterior restorations.7 See Table III for a summary of “implant fracture risk factors”. See Figures 9A to 9C for a case where two grade I pure titanium implants were restored in the posterior zone, then fractured after two years in function, were removed, the explantation sites were grafted, and then the implants were replaced on a “delayed” basis with two wide neck Grade IV cold worked titanium implants. See Figures 10A to 10C for two cases where the Grade I implant body fractured and was buried.
Fig. 9A
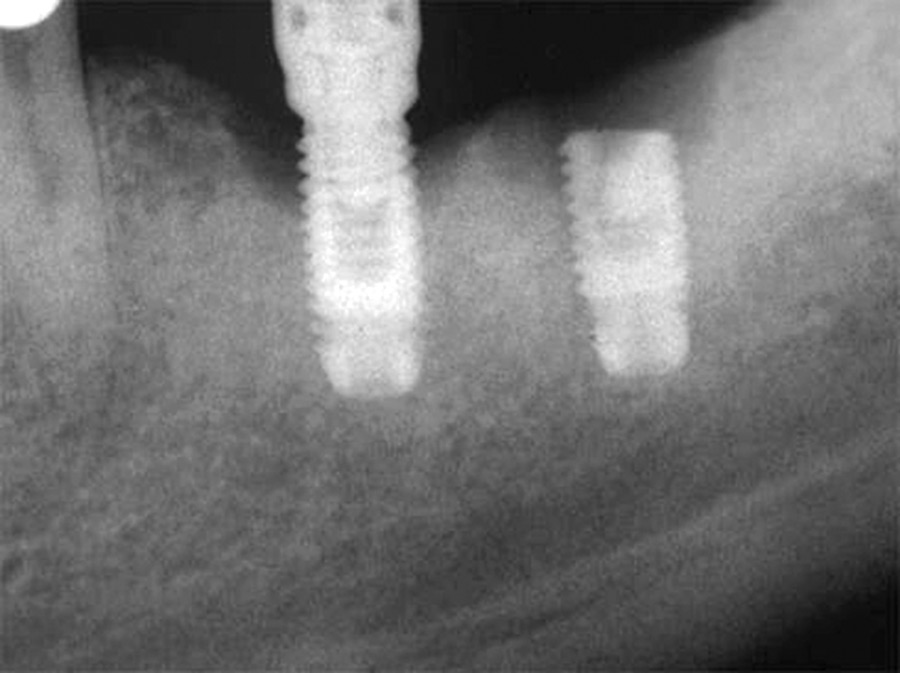
Fig. 9B
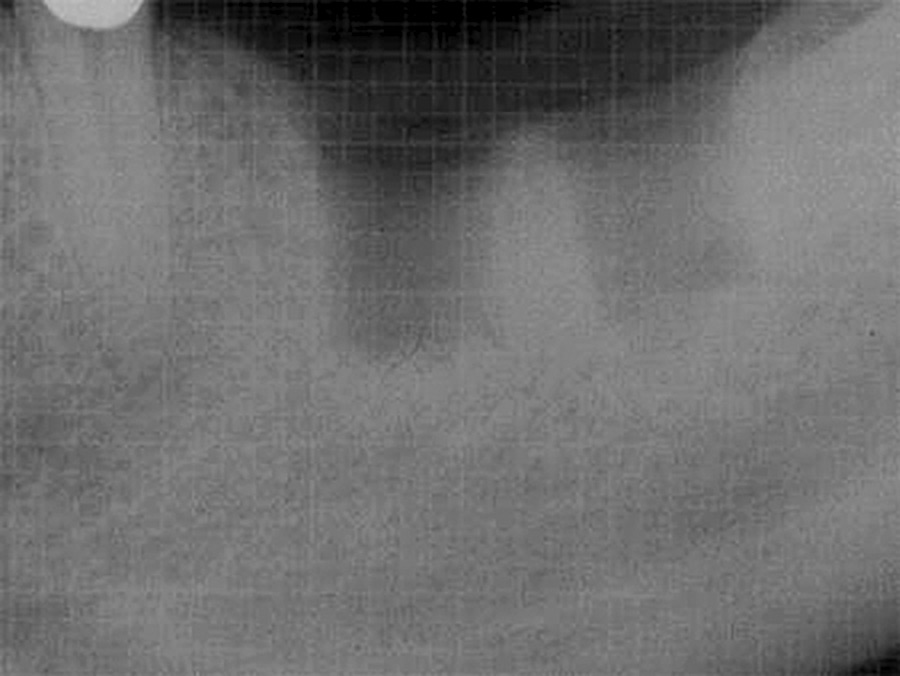
Fig. 9C
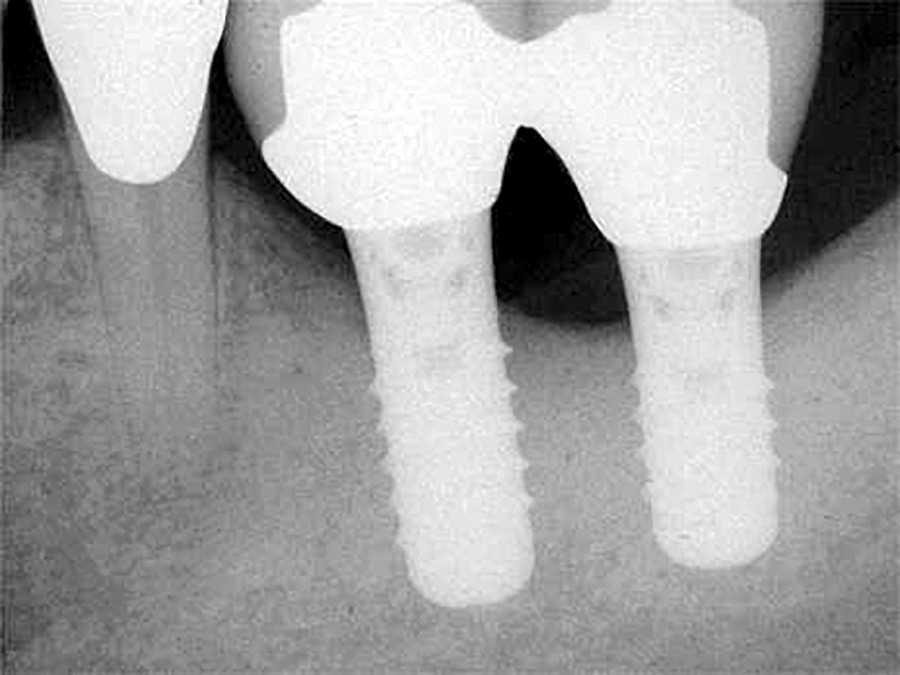
Fig. 10A

Fig. 10B
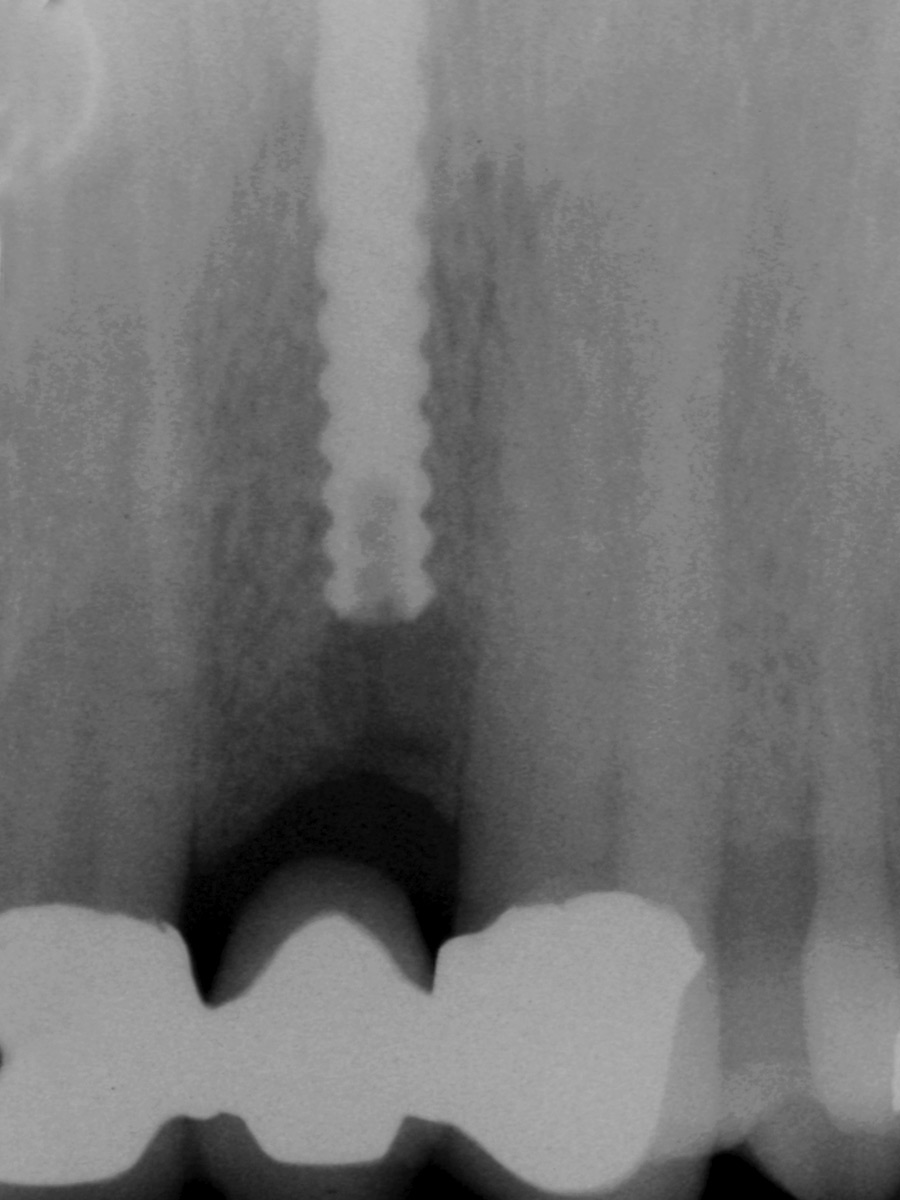
Fig. 10C
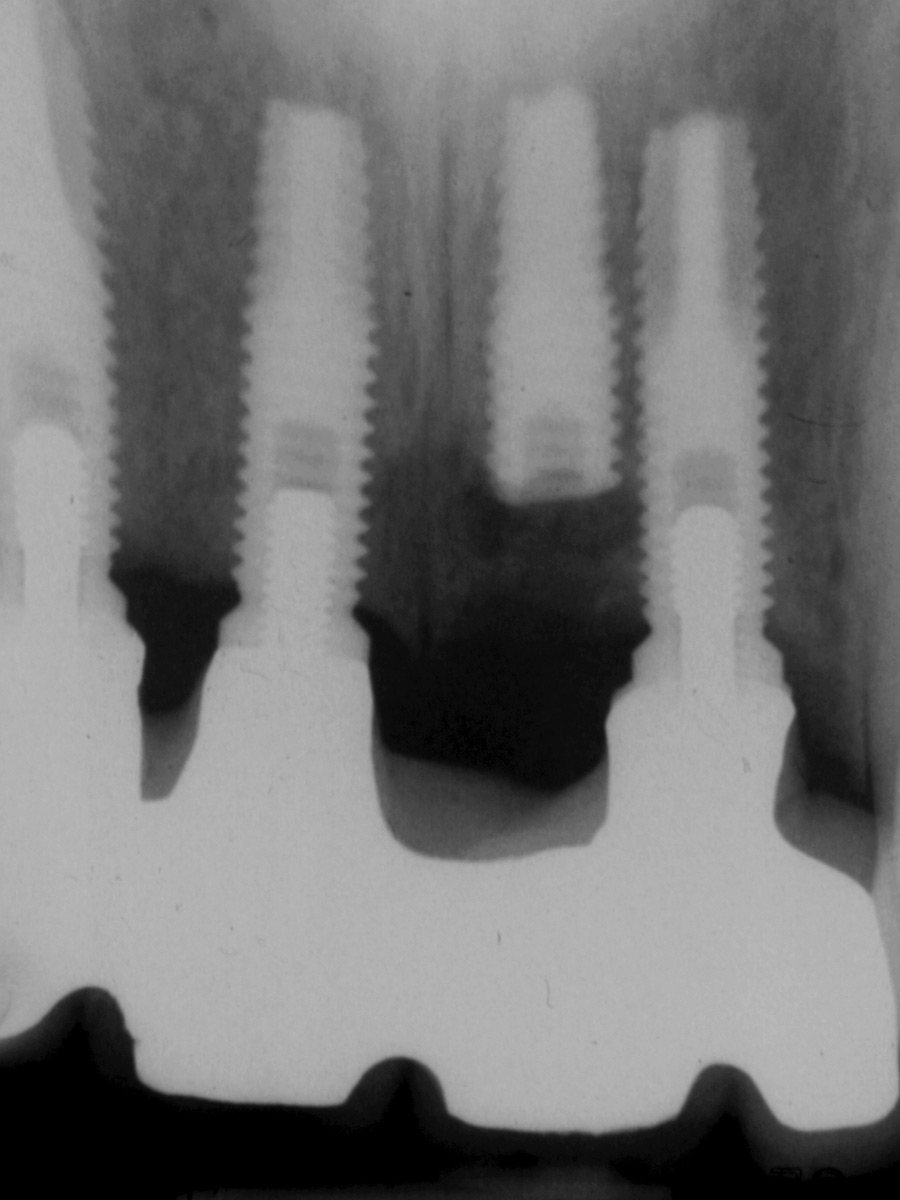
Implant Prosthetic Module Fracture (“Hex Split”)
Fractures of the implant prosthetic module are very rare (anecdotal) with contemporary implants but prior to 1996 a popular internal hex system experienced about a 10% “late” fracture rate (personal experience). Specifically, the “hex” of the implant would “split” open thus the term “hex splits” was born. These fractures typically occurred two to three years after restoration and may have been due to “metal fatigue” combined with the relatively thin metal wall at the “apex” of the internal hex. In 1996 the manufactured thickened the metal walls by 0.2 mm and the hex splits all but disappeared (personal experience). See Figure 11A for a case where two implants suffering hex splits were “buried”, two new additional implants were placed and the case re-restored. Also, see Figures 11B and 11C for a case where the implant suffering the hex split implant was removed, and immediately replaced with a wider implant.
Fig. 11A

Fig. 11B
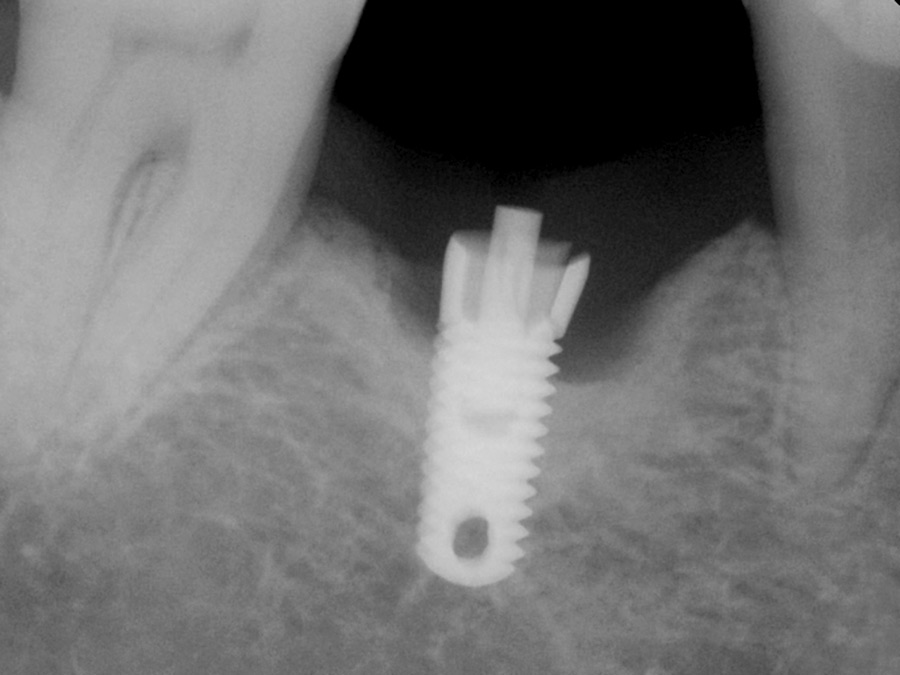
Fig. 11C
Miscellaneous Etiologies for Unrestored Implants
There can be other reasons where implants can be restored but are not. For example, a patient may change their mind after the implants are placed and choose not to restore some or all of their implants (sometimes for financial reasons). At times the restorative dentist and or patient may decide not to utilize all the implants in order to reduce the cost and or to simplify the restorative procedures. There can be other less common reasons, for example see the case in Figure 12. In this case the patient was having an implant placed at the 2.4 and at the same time crown lengthening prior to redoing her conventional fixed bridge at the 25 to 27. As the long-term prognosis of the bridge was questionable, an additional implant was “buried” at the 2.6 for potential future needs in Case 1 or both bridge abutments were to be lost in the future.
Fig. 12
Summary
This 5th article of the series of articles from this author submitted to Oral Health has continued on the subject of “Risk Factors in Implant Dentistry”. Specifically this 5th article has discussed the influence of some of the risk factors that impact on the restorability of implants, primarily due to implant malposition and component fracture such as abutment and or implant fractures. In the overall classification of risk factors in implant dentistry as outlined in Table I, the subject of this 5th article falls under both categories of “Operator Related Risk factors” and “Biomaterial Related Risk Factors”. This article also illustrated some of the author’s cases from his private practice, i.e. primarily illustrating cases exhibiting the risk factors leading to unrestorable implants.
Oral Health welcomes this original article.
References
- Arlin, M.L. “Surgical risk factors in implant dentistry: Effect on failures and bone loss”. Oral Health, August 2015, pages 32-38.
- Arlin, M.L. “Risk factors in implant dentistry: Patient related risk factors”, Oral Health, August 2016, pages 26-36
- Arlin, M.L. “Surgical risk factors in implant dentistry: Patient Local related risk factors”. Oral Health, August 2017, pages 10-24
- Arlin, M.L. “Surgical risk factors in implant dentistry: Operator related risk factors” Oral Health, August 2018, pages 40-57
- Salama H, Salama MA, Garber D, Adar P. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998 Nov-Dec; 10(9):1131-41.
- Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001 Oct; 72(10):1364-71.
- Eckert SE, Meraw SJ, Cal E, Ow RK. Analysis of incidence and associated factors with fractured implants: a retrospective study. Int J Oral Maxillofac Implants. 2000;15: 662–667.
About the Author
 Dr. Arlin received his DDS in 1977 (McGill), his Periodontics degree in 1980 (Toronto) and his FRCD(C) in 1983. He lectures locally, internationally, and authors many articles. He founded several study clubs, is a past president of the OSP, OSCO, and was head of the CAP’s Perio course. In 1980 Dr. Arlin started his practice and has placed over 14,500 implants.
Dr. Arlin received his DDS in 1977 (McGill), his Periodontics degree in 1980 (Toronto) and his FRCD(C) in 1983. He lectures locally, internationally, and authors many articles. He founded several study clubs, is a past president of the OSP, OSCO, and was head of the CAP’s Perio course. In 1980 Dr. Arlin started his practice and has placed over 14,500 implants.












