Introduction
Most restorative dental treatment is because of dental caries, the most-prevalent disease in humans. Unchecked dental caries infection causes dentinal spread (cavitation) and destruction of tooth surfaces. Although we have been well trained as dental clinicians to diagnose caries lesions as early as possible, identifying the presence of early caries lesions proves to be challenging prior to cavitation, because our detection methods are crude and insensitive1. For example, bitewing radiographs do not normally reveal presence of a caries lesion until it is halfway through the enamel layer, histologically. By then the lesion may be more advanced than it first seems and close to the dentin.
With the advent of new early detection tools, there is promise of managing proximal caries lesions that are not detectable clinically, prior to cavitation. This could provide a healing effect while preventing cavitation, requiring restorative treatment.
Over the years, various methods have been used to manage visible caries lesions of axial surfaces that have not yet cavitated but are significantly demineralized. Such methods include separation of the teeth using orthodontic separators and applying a surface sealant2. If the contacting tooth is a primary molar, a class II glass ionomer restoration in the adjacent tooth has been placed to provide sufficient fluoride release to remineralize the contacting early lesion3. Although these and other measures have been attempted, the challenge remains to identify the status of the lesion at the outset and to evaluate the outcome of whatever treatment is chosen.
Most clinical dentistry involves removal of caries lesions and restoration of affected teeth. Because detection of the presence of non-cavitated caries lesions is difficult, we sometimes make faulty assumptions about the status of a lesion.
In reviewing the dental literature to find what treatments have been used to treat non-cavitated caries lesions, one finds smooth surface sealants, resin infiltration, enamel microabrasion, and various fluoride applications.
Surfaces treatment methods
Sealants
Bonded resin sealant material, used primarily for pits and fissures, has been used for contacting proximal surfaces as well4. The challenge is how to reliably bond the resin to the smooth surface. Some clinicians have attempted to separate teeth and apply a sealant to an acid-etched proximal surface. There is little data to support this technique and it has not gained much interest in the profession. (Figs. 1 & 2)
Fig. 1

Fig. 2

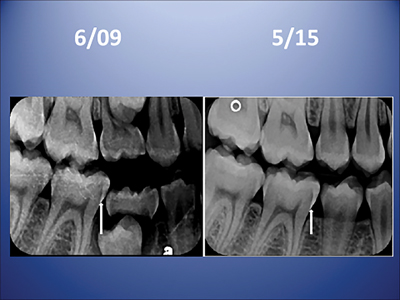
Resin Infiltration
Resin infiltration has been in clinical practice for around 12 years. It allows the application of a fluid (diluent) resin to penetrate the enamel surface into the enamel caries lesion all the way to the dentino-enamel junction, after a surface treatment. The procedure involves acid treatment of the enamel surface and the application of resin, with the goal of stopping progression of a non-cavitated early lesion. This method is well documented with long-term controlled trials.5,6 (Figs. 3 & 4) Although such resin infiltration is scientifically sound and well supported, it is technique sensitive, and requires ideal rubber dam placement. It has not been documented to be effective unless a carefully placed rubber dam is used; when a properly placed rubber dam is used, studies show that resin infiltration slows or halts early caries lesion progression on approximal tooth surfaces.7
Fig. 3

Fig. 4
Microabrasion
Enamel microabrasion, is used effectively to treat superficial discoloration and decalcification lesions on facial surfaces of teeth, especially incisors and canine teeth. The combination of hydrochloric acid and abrasive particles in a water-soluble gel has been marketed since the late 1980s. Enamel microabrasion permanently removes an imperceptible amount of surface enamel and superficial intrinsic discoloration with it, leaving a lustrous surface as it remineralizes. (Figs. 5,6 & 7) However, the structure of a caries lesion that is not yet cavitated is different from a “dysmineralization” defect, therefore enamel microabrasion is not recommended for treating early caries lesions8. It is mentioned here for completion sake, because it is an enamel surface treatment9.
Fig. 5

Fig. 6

Fig. 7

Silver Diammine Fluoride
Recently, several authors have described the use of 38% silver diammine fluoride (SDF) to treat approximal non-cavitated lesions.10,11 SDF, developed in Japan in 1969 was introduced and approved in North America as a tooth desensitizing agent in 2015. Its off-label use of abating the progress of dental caries infections has become extremely popular in the last half year. The chief question is how to apply the silver diammine fluoride liquid on lesions of contacting proximal tooth surfaces. It can be applied with floss, particularly the “fuzzy” kind, but recently Croll and others have documented the use of soft dental picks inserted interproximally.12 Fig. 8 Although neither of these methods of application has been studied in controlled clinical trials, positive clinical outcomes have been described in peer reviewed articles. One big advantage of soft dental pick SDF insertion is that multiple interproximal sites can be treated simultaneously. Immediate fluoride varnish covering of treated teeth is an important part of the dental soft pick application protocol. The dental soft pick method can be outlined by the following steps:
- clear the interproximal site with dental floss
- isolate the region, typically with cotton rolls or an absorbing pad for maxillary teeth
- dry the site with air spray and insert the soft pick that has been coated with SDF fluid
- with a small applicator, paint more fluid all along the sluiceways
- slide the soft pick in and out a few times to achieve flow of the fluid
- leave the soft pick in full insertion for about 60 seconds then coat the region with 5% fluoride varnish, making sure the varnish flows into the void left by removal of the pick.
- have the patient occlude on a 2×2 cotton gauze for about 3 minutes.
Studies are recommended to investigate the full implications of this method.
Fig. 8

Fluoride
The use of fluoride as a remineralizing agent to intercept non-cavitated caries lesions has been practiced by dentists more than any other method. However, there are several papers going back 30 years or more on the use of fluoride, that discuss the need to assess the status of the lesion at the outset. First it must be determined that the lesion is not yet cavitated; if it were to be cavitated, the ability of fluoride to remineralize and repair the surface is limited.13 Because radiographs are very poor and insensitive in determining the status the lesion, it is difficult to assess the effectiveness of fluoride application in such cases. However, as improved and more sensitive methods of early detection of caries lesions are developed and become available, smooth surface enamel “healing” by various fluoride products could be a real possibility.14 As seen in Figs. 9-11, there is a small distal lesion on tooth #55, yet that tooth will exfoliate in several months. There is likely a small lesion already formed on the mesial of #16, albeit undetectable radiographically or clinically. Placement of a DO restoration on #55 with a glass ionomer material can leach fluoride from that restoration into the lesion on #16, healing it over time.
Fig. 9
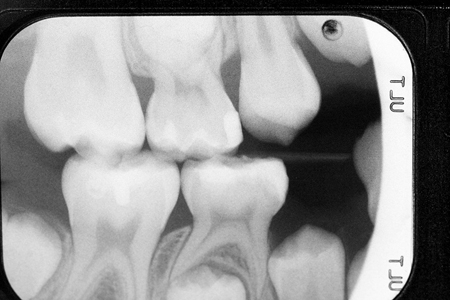
Fig. 10

Fig. 11

Discussion
It is intriguing to consider current methods and what will be used in the future for the treatment of proximal surface caries lesions. A primary “medical” approach will undoubtedly delay and perhaps in some cases preclude the surgical restoration of teeth. The first surgical cutting and restoration of a tooth surface is inevitably not the last.
As noted above, the inability to determine the status of a caries lesion at the outset affects the ability to determine appropriate treatment and how successful it might be. Yet today, there are examples of improved early caries lesion detection methods including the use of: laser fluorescence, intense visible light on the surface, separation of teeth with orthodontic separators and visual exploration. New concepts of caries diagnosis and other methods yet to be developed give hope that prevention of the disease could play a much bigger role than surgical intervention for teeth with advanced carious infection.
“Watching” a caries lesion in practice, while documenting it as “non-cavitated” is commonly accomplished with a note in a patient’s dental record. Although not discussed in the context of this paper, it is important to note that a big part of the problem related to lack of predictive evidence in treating non-cavitated proximal lesions, is that the profession has not generally implemented a system of tracking the diagnostic status of caries lesions.
In clinical research studies in an academic institution, where it is easier to document the precise status of caries lesions going into a study, it is possible to acquire credible information regarding outcomes, at certain intervention periods. In fact, watching lesions or merely noting their presence prior to cavitation, or assuming that they have not cavitated is likely one of the largest recordings in the database of one’s practice. This speaks to the need for practitioners to carefully document the status of lesions that have not progressed to the point of cavitation, so future comparisons can be made. Clearly, dentists and patients would favor definitively reducing the progression of caries lesions if there was a sure way of achieving this goal. Financial incentive to deploy “medical” treatments in attenuating progression of caries lesions certainly plays a big factor in how patients and dentists view the dental caries problem. Third party carriers generally do not reimburse patients and dentists significantly for non-surgical approaches to caries management. This is true for a variety of reasons and must be challenged and changed.
Conclusion
The idea of minimally invasive medical treatments on the surface of proximal lesions prior to cavitation is consistent with the notion of medical management of dental caries. This is the intent to manage dental caries as a disease as opposed to merely using a “lesion specific” approach. The latter approach, waiting for caries lesions to advance until restorative intervention is necessary, ignores the modern science associated with understanding of oral biofilm as well as dietary saliva and other factors contributing to the progression of caries lesions. If we continue to treat caries only as lesions (the outcome of the disease) and not as a disease leading to those lesions, our attempts to manage the disease like other chronic diseases, will be futile.
Oral Health welcomes this original article.
References
- Schwendicke, Falk and Göstemeyer, Gerd. Conventional bitewing radiography Clinical Dentistry Reviewed (2020) 4:22.
- Croll TP: Bonded resin sealant for smooth surface enamel defects: new concepts in “microrestorative” dentistry. Quintessence International, 18: 5-10, Jan 1987.
- Croll TP, Berg J: Delivery of fluoride solutions to proximal tooth surfaces, Part I. Inside Dentistry, 13(7):90-91, July 2017.
- Croll TP, Sundfeld RH, Berg JH: A pit-and-fissure clinical protocol. Compendium Contin. Educ. Dent, 26(12):862-868, Dec 2005.
- Arslan, Soleyam and Kaplan, Melek Hilal. The Effect of Resin Infiltration on the Progression of Proximal Caries Lesions: A Randomized Clinical Trial. Med Princ Pract 2020; 29:238–243.
- Peters MC, Hopkins AR Jr, Zhu L, Yu Q. Efficacy of Proximal Resin Infiltration on Caries Inhibition: Results from a 3-Year Randomized Controlled Clinical Trial. J Dent Res. 2019 Dec;98(13):1497-1502.
- Paris S, Hopfenmuller W, Meyer-Lueckel H. Resin infiltration of caries lesions: an efficacy randomized trial. J Dent Res. 2010 Aug;89(8):823-6.
- Croll, TP: Enamel Microabrasion, (textbook) Quintessence Publishing Company, 1991.
- Donly KJ, Croll TP: Enamel microabrasion for removal of superficial coloration and surface texture defects. Chapter 9 in: Perdigao, J: Tooth Whitening-An Evidence-Based Perspective. Springer, Switzerland, 2016, pp 201-209.
- Croll TP, Berg JH, Donly KJ. Silver in medicine and dentistry. Inside Dentistry. 2020; 16(10):35-40.
- Croll TP, Berg JH. Radiographic verification of silver diammine fluoride action on proximal dental caries lesions in a teenager. Dental Economics. 2021; 111(5):52-53.
- Croll TP, Berg JH: Delivery methods of silver diammine fluoride to contacting proximal tooth surfaces and history of silver in dentistry. Compend Cont. Ed. in Dent. 2020; 41(2): 84-90.
- Croll TP, Berg J: Delivery of fluoride solutions to proximal tooth surfaces. Part II: Caries interception with silver diamine fluoride. Inside Dentistry, 13(9):56-58, September 2017.
- Croll TP, Berg JH, Christensen GJ. SDF for managing open gingival floor margins in Class II restorations. Inside Dentistry. 2021; 17(5):20-24.
About the Author
 Dr Berg is a consultant in the dental industry and practices Pediatric Dentistry part-time in the Phoenix area. He is former Dean at the University of Washington School of Dentistry. He is a Past-President of the AAPD. He is also a Past President of the American Academy of Esthetic Dentistry.
Dr Berg is a consultant in the dental industry and practices Pediatric Dentistry part-time in the Phoenix area. He is former Dean at the University of Washington School of Dentistry. He is a Past-President of the AAPD. He is also a Past President of the American Academy of Esthetic Dentistry.
 Dr. Croll is Clinical Director of CAVITY BUSTERS DOYLESTOWN, LLC in Doylestown, Pa. He is currently Adjunctive Clinical Professor of Pediatric Dentistry at the University of Texas Health Science Center in San Antonio and Clinical Professor of Pediatric Dentistry at Case Western School of Dental Medicine.
Dr. Croll is Clinical Director of CAVITY BUSTERS DOYLESTOWN, LLC in Doylestown, Pa. He is currently Adjunctive Clinical Professor of Pediatric Dentistry at the University of Texas Health Science Center in San Antonio and Clinical Professor of Pediatric Dentistry at Case Western School of Dental Medicine.
Read more articles from the 2021 Proactive Intervention Dentistry issue!












