Upon insertion of a newly fabricated dental prosthesis, it drops intraorally and fits perfectly requiring minor adjustments. The patient looked in the mirror following this insertion and was delighted with the final aesthetics results. The patient states, “It looks and feels perfect, just like my natural teeth”. As dentists, we take full credit and thanks our patient for treatment well done.
A few patients later, there is another final prosthesis insertion appointment scheduled. However, this appointment was not as successful as the initial prosthesis insertion. The implant crown did not fit passively requiring multiple adjustments inter proximally to insert and heavy occlusal adjustments to achieve implant protected occlusion. The shading was mismatched to adjacent teeth and morphology of the crown looks like a dinner bun rather than the anatomy of a tooth. As dentists, we feel embarrassed assessing the final clinical outcome. In situations when this occurs, we target our scapegoat often stating, “Oh its that dental laboratory technician again”. We blame someone who the patient does not know and has never met.
As Prosthodontic residents at University of Toronto, in our the first year of training we were mandated to spend a full month in a commercial dental laboratory to observe and fabricate dental prosthesis. We rotated through departments ranging from fabrication of master models to mounting; we fabricated and waxed up dentures to completion with final processing. Additionally, we participated in the fabrication of fixed crown and implant restorations and we were introduced to digital scanning technology and 3-dimensional printing as it applies to dental technology. We witnessed a wide range of bite registrations and lab prescriptions provided by dentists as well as the formulation of final impressions, assessing their quality at completion. Most dental laboratory managers would concur with the concept of “garbage in, garbage out”. As a result, sometimes laboratory managers are required to make uncomfortable phone calls to dentists, politely asking for another impression or for other pertinent information used to facilitate the fabrication of the desired dental prosthesis.
In order to bridge the gap, no pun intended, between clinical dentists and dental laboratory technicians, this article outlines the responses gathered from interviews with 4 different dental technicians, all from different laboratories; all technicians have had a vast range of experiences. This article is intended to improve the communications and appreciate the challenges faced by our “Silent Dental partners”. Below are the questions that were asked to technicians and the corresponding answers that they provided:
1) Please tell us about your experience as a Dental Laboratory Technician, i.e. number of years of working experience, your current role and job duties for your respective dental laboratories.
Slawek Bilko of LHM Dental Studios Ltd.:
“I was trained as a dental technologist in Germany and began work there in 1993. I came to Canada in 1990 and began working for Lindberg & Homburger. I am currently the owner of that lab, now called LHM Dental Studios. As dental implants emerged as an option for patients, I embraced the technology and quickly became known as an expert in the field. As recognition for this, I was invited to become an ITI Fellow and I am currently the only dental technologist to have this distinction. I continue to embrace the latest in dental technology.”
Mike Callaghan of SHAW Lab Group:
“I’ve been in the business for 31 years and I have worked all aspects of dental technology including dentures, orthodontics, crown and bridge, implants and CAD/CAM dentistry, as well as chair side in-office experience.”
Rudy Ghoubrial of ADL Dental Laboratories Ltd.:
“After I finished studying the dental technology program, I got the opportunity to work at ADL Dental Laboratories. I started my career in the model department and I worked my way up. I was lucky enough to work in every department and I gained most of my experience in the porcelain department working with all the Aesthetic and Full Mouth Rehabilitation cases. As an ADL technician I attended the same courses dentist and prosthodontists did to truly understand dentistry from their perspective. After working in every department over those 20 years, I got the opportunity to become the Director of Technical and Lab Operations.”
Andreas Sommer of Durban Dental Laboratories:
“With more than 35 years of experience, I began my career in a family owned dental laboratory, Micro-Dent, in Toronto, ON, in 1982. I founded Sommer Restorative Prosthetics in 1992 and then merged with the Aurum Group as a vice president/co-owner of Aurum-Classic Dental Lab Toronto from 1994 to 2014. I then purchased the lab and merged it with Durban Dental, I am now the vice president/co-owner of Durban Dental Laboratories (Toronto) since 2015. Also maintaining a private practice denture clinic, Sommer Denture Centre since 2013. My background includes an extensive knowledge in cosmetic, implant, physiologic dentistry, full intraoral rehabilitations, and denturism. In my current post I ensure and maintain quality control, oversees workflow and laboratory projects in all departments and works in all areas of the dental lab, including dentures, cast partials, orthodontic appliances, crowns, and bridges. I am a handson technologist and lecturer on restorative dental lab materials for leading dental manufacturers such as Myerson and Dentsply/Sirona. I have attended the Dental Technology Program at George Brown College. I received my license as a dental technologist by the College of Dental Technologists of Ontario in 1991. Graduating in 2012 with a diploma in denturism from Trillium College. I strive to stay on the cutting edge of dental technology with attending numerous CE events, with the advent of digital technology I am diligently following the latest updates and changes while continuing my professional growth.”
Fig. 1
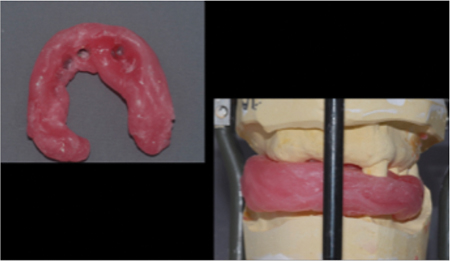
Fig. 2
2) As dental laboratory technicians, in your expert opinion, what are some of the common mistakes, challenges, miscommunications or preventable error made in the following aspects of dentistry?
a) Fixed Prosthodontics
b) Removable Prosthodontics
c) Aesthetic dentistry
d) Fixed Implant Prosthetics
e) Removable Implant Prosthetics
f) Common miscellaneous errors
Slawek Bilko of LHM Dental Studios Ltd.:
a) Fixed Prosthodontics: “Bad impressions are the most common problem and are the most preventable errors. Inadequate reductions, wrong bites – common problems which are easily preventable. Communication: poor prescriptions that are lacking in detail and instruction. Requires follow-up phone calls that take extra time.”
b) Removable Prosthodontics: “Very often doctors can’t take a bite at the appropriate VDO, which results in multiple re-sets and inadequate rest preparations.”
c) Fixed Implant Prosthetics: “Inadequate interocclusal space. Bad implant placement – can’t make screw retained restoration when requested. Not willing to make verification jig and pick up impression.”
d) Removable Implant Prosthetics: “Inadequate interocclusal space. Not willing to make verification jig and pick up impression.”
e) Common miscellaneous errors: “Not having washed or disinfected the impressions. Send pictures that we could use when choosing shade. Adjust interproximal contacts so we could make long, broad contacts.”
Mike Callaghan of SHAW Lab Group:
a) Fixed Prosthodontics: “We see poor impressions lacking details, incomplete impressions, pulls, drags and insufficient impression material. Recently seeing more plastic triple trays for single crowns and bridges which in themselves are too flexible creating distortions not seen after tray removal. We are not seeing preps that consider for materials, ie: sharp line angles, insufficient clearance, margins in undercuts, over contoured preps.”
b) Removable Prosthodontics: “For the most part dentists have lost the art of dealing with removable dentures. We think this because we hear our clients often say that they hate dentures. Too many short cuts, leading to multiple tryins that often end up with poor results and disappointed clients. Maybe they are tackling cases where patient expectations are too high for what the final result actually is.”
c) Aesthetic dentistry: “Poor prep designs, no pre-planning, lack of communication about the underlying tooth colours, under preparing with expectation of material that will not satisfy the end result.”
d) Fixed Implant Prosthetics: “Not attending proper continuing education courses, however we rarely see it prosthetically driven. Implants too deep, too shallow, too facial, and too palatal. No consideration for inter occlusal space especially with full arch dentistry. Price often wins over the right thing to do, as often a better long-term solution exists but finances get in the way.”
e) Removable Implant Prosthetics: “Not enough implants for the restoration, not enough inter-occlusal space. As an example, a dentist wants a horseshoe palate when they should know that these are tissue borne and need the palate for stability.”
f) Common miscellaneous errors: “When a prescription is not detailed enough. Appointments dates are missing, stump shades missing, lack of patient records, ie: photos, inaccurate bite registration, etc. No study models, no X-rays provided for implant cases. Cases being rushed when complicated as well as a lack of understanding of the lab process. Often times laboratories are blamed and the dentist will wonder if the laboratory has altered the case in any way to have caused the complications. We believe it’s a two-way street, that problems are often two-sided and can be resolved with better communication.”
Rudy Ghoubrial of ADL Dental Laboratories Ltd.:
a) Fixed Prosthodontics: “Not enough clearance in the occlusion, distorted impressions, bulky preparations, inaccurate bite registrations and wrong shades.”
b) Removable Prosthodontics: “Distorted impressions, wrong bite registration, no border-molding, insufficient preps for cast partials and inaccurate set-up try-in.”
c) Aesthetic dentistry: “Poor planning, not enough reductions for veneer cases, no diagnostic wax up-and no pictures for shape or shade).”
d) Fixed Implant Prosthetics: “Poor planning, improper implant placement angulation, not enough vertical height and an implant being placed too close to the adjacent teeth.”
e) Removable Implant Prosthetics: “Implants are placed too deep or too high to use locators, not enough vertical height to use bars with locators or bars with attachments and incorrect implant placement angulation.”
f) Common miscellaneous errors: “Using wrong impression coping’s (open tray vs. close tray), using the wrong bite registration material, not enough detailed information given on the prescription.”
Andreas Sommer of Durban Dental Laboratories:
a) Fixed Prosthodontics: “Insufficient prep designs, to be anatomic in design, molars should not have flat occlusal plane, preparing a sulcus, anterior reductions, labially the tooth has three basic planes that have to be reproduced in the final crown, provide clear and accurate margins, provide proper retraction for impression taking, inadequate bite registrations, adhesive in trays to prevent separation of the impression material from the tray, improper use of triple tray’s (the should not to be used for bridges, single tooth only with a minimum of one tooth on either side and always send a bite registration. Never use two triple trays to take a full arch impression. Improper retraction around the margin, margins not properly defined and inaccurate PVS impressions. Impressions should be reviewed chair-side for drags and voids.”
b) Removable Prosthodontics: “Proper final impressions, i.e. border molding of full denture cases, PVS and custom trays for cast partials, incomplete saddle areas in lower posterior edentulous cast partials (altered cast impressions), bite blocks missing proper markings-midline, cuspid lines, smile lines.”
c) Aesthetic dentistry: “Smile design shapes, proper wax ups, providing models of ap-proved temporaries, accurate preps and impressions.”
d) Fixed Implant Prosthetics: “Proper impression copings for the case, closed tray should only be used for a single perfectly placed implant, otherwise open tray is the better option for multiple and angled implants.”
e) Removable Implant Prosthetics: “Properly designed custom trays, verification jigs luted intra-orally for passivity and accuracy of models.”
f) Common miscellaneous errors: “Implant transfers not being x-rayed at the time of impression, anterior emergence profiles not being developed properly in implant restorations in the temporary phase allowing for proper thickness of the materials used in the restorations, prescriptions not properly filled out, this is a legal document in record keeping, not using firm/ridged bite registrations, not having all the proper armamentarium for restoring implants, i.e. screw drivers.”
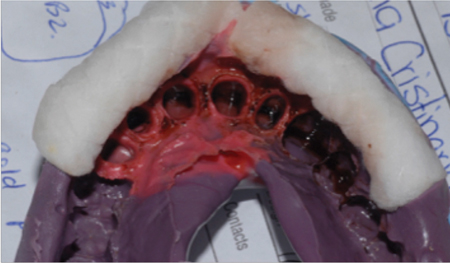
Fig. 3

Fig. 4
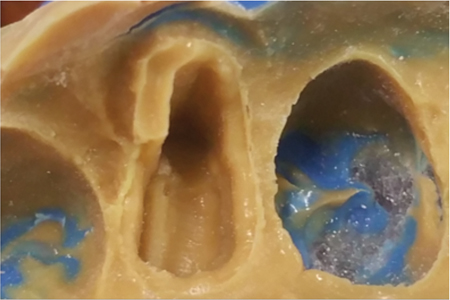
Fig. 5

3) Please make five recommendations where an improved teamwork and collaborations between the dentists and lab technicians can be achieved to optimize the final dental prosthesis.
Slawek Bilko of LHM Dental Studios Ltd.:
• “Treatment planning before a case begins.”
• “Use of full arch impressions.”
• “Use of firm and rigid bite registration material.”
• “Use of shoulder preparations for metal free restorations.”
• “Give a brief but exact description of what is required to be done on the case.”
Mike Callaghan of SHAW Lab Group:
• “More detailed prescriptions.”
• “Technicians and dentists should attend courses together so that they are learning together.”
• “We would like our clients to come visit the laboratory to get a greater understanding of the technology and processes involved.”
• “Post-operative photos that communicate the end result, good or bad so we can learn and improve.”
• “Greater use of technology to communicate; Skype, video conferencing about cases and greater knowledge of patient expectations. Perhaps a document where the patient describes in writing their expectations of the end result.”
Rudy Ghoubrial of ADL Dental Laboratories Ltd.:
• “Planning cases in advance.”
• “Clear instructions and information about cases.”
• “Building a strong relationship between the dental laboratory and dental office teams.”
• “Technical communications should be with one person all the time to ensure accuracy and consistency.”
• “Exchange dental experience between dentist and dental laboratories.”
Andreas Sommer of Durban Dental Laboratories:
• “Proper case/treatment plan outline and prescription.”
• “Study models and bite registrations.”
• “Photos (AACD).”
• “Working with check lists.”
• “Provide all implant information, i.e. letters from the surgeon, provide information on the prescription, photocopy of the sticker on file.”
Fig. 6

Fig. 7
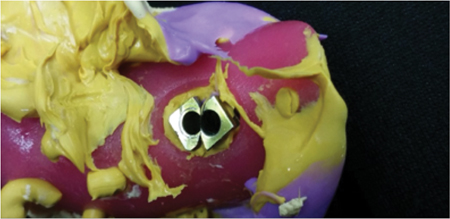
Fig. 8

4) In your opinion, what technical advances in dental laboratory will impact the quality of dentistry in the best interest for our patients?
Mike Callaghan of SHAW Lab Group:
“Digitally planned cases, digital impression taking, digital smile design. Printed models, printed surgical guides, printed and/or milled denture and orthodontic appliances will make huge advancements with consistent and predictable results. Modelless dentistry will be more accurate with faster turnaround times for ease of patient scheduling.”
Rudy Ghoubrial of ADL Dental Laboratories Ltd.:
“In my opinion, the digital technology and CAD/CAM technology will improve the quality and the accuracy of all our work to benefit the patients.”
Andreas Sommer of Durban Dental Laboratories:
“Intraoral scanners, milling of model’s and restorations, 3D printing of model’s and restorations, digital surgical planning of comprehensive implant and orthodontic cases.”
Fig. 9

Fig. 10

5) What final message would you wish to share with all the dentists in regards to improved communications with the dental laboratory technicians and clinical dentists?
Slawek Bilko of LHM Dental Studios Ltd.:
“Please write clear prescriptions (handwriting as well as content.) Tell us what you would like us to do, don’t let us second guess. Involve us in the treatment plan. Give us sufficient time to work on the cases.”
Mike Callaghan of SHAW Lab Group:
“We want to know the good, the bad and the ugly that we do. Communication can only make us better at what we do together. There is a trial period for us to know each other’s preferences and to build a foundation to be successful in the long term. There maybe be hiccups along the way, but if given enough time we can truly have great teamwork.”
Rudy Ghoubrial of ADL Dental Laboratory Ltd.:
“The message I wish to share with all the dentists is to improve communications between dental laboratory technicians and clinical dentists. As a dentist please build strong relations between you and your laboratory technician, communicate about cases clearly, send study models to your laboratory technician and digital photos to discuss cases in advance, visit your dental laboratory to see the process of the cases, meet the technicians and learn about the technology they have invested in.”
Andreas Sommer of Durban Dental Laboratories:
“If you are working with a knowledgeable laboratory they are a great asset in planning out cases. They can provide technical solutions, material choices and timelines for case fabrications. Provide the overall treatment plan of the case and always plan your cases with the final result in mind. Remember it’s the patient we all are working for!” OH
Oral Health welcomes this original article.
About the Author
 Dr. Mark H. E. Lin graduated from the University of Detroit Mercy for his dental program. He then completed a one-year General Practice Residency program at the Miami Valley Hospital in Dayton, Ohio. He practiced general dentistry for 13 years and then returned to complete his post-graduate training in the specialty of prosthodontics at the University of Toronto. He maintains a full-time specialty practice as a prosthodontist at Dr. Mark Lin Prosthodontic Centre.
Dr. Mark H. E. Lin graduated from the University of Detroit Mercy for his dental program. He then completed a one-year General Practice Residency program at the Miami Valley Hospital in Dayton, Ohio. He practiced general dentistry for 13 years and then returned to complete his post-graduate training in the specialty of prosthodontics at the University of Toronto. He maintains a full-time specialty practice as a prosthodontist at Dr. Mark Lin Prosthodontic Centre.












