Introduction
Amidst various technologies and treatment options for replacement of one’s tooth, dental implants have become the standard of care in present day practice. No longer are we enamoured by the body’s ability to accept an endosseous implant as its own. The landmark phenomenon of osseointegration by which titanium fuses to bone at a microscopic level allowing for rehabilitation of single or multiple teeth is now routinely seen in everyday practice.1
That said, the time lines, protocols and indications of implant dentistry are constantly evolving. Where we once felt it necessary to wait great lengths of time between extraction, implant placement and restoration we are now aware that expedited therapy including same day care exist to our patient base.2 In keeping with this patient centred mentality many surgical techniques have been employed to circumvent adjunctive procedures and streamline care for those desiring tooth replacement.
In an effort to tackle thin alveolar ridge deformities without the need for horizontal augmentation, manufacturers have developed narrower implants with similar strength properties3 and burs which can expand the boney housing.4 Similarly, the advent of shorter dental implants5 and various kits to maneuver anatomical barriers such as sinuses and nerves have grown in popularity. In addition, modern treatment concepts have now championed the placement of angulated implants6,7 to avoid some of the aforementioned anatomic concerns. In recent years groups of clinicians have actually advocated maintenance of a portion of tooth in an effort to maintain the buccal bone and convex form to improve esthetics during implant placement – what is now referred to as partial extraction therapy (PET).8
In keeping with this so-called “convenience profile” of treatment alternatives which aim to minimize number of surgical procedures, morbidity and cost while increasing case acceptance, this article outlines an unconventional approach to aid a patient in implant rehabilitation. This treatment plan represented a less invasive option that was not explored by other clinicians during a number of previous consultations which involves placement of dental implants directly through a maxillary impacted canine.
Although a number of articles exist which examine the efficacy of placement of dental implants through impacted teeth9-11 this article shows immediate placement and temporization. As far as the author is aware this is the first of its kind.
Case Background
A 48-year-old, systemically healthy, non-smoking male presented for consultation regarding replacement of several questionable anterior maxillary teeth. The patient had previously visited a number of dentists and surgeons and was seeking a tertiary opinion. In all circumstances, teeth 53 and 12-22 had been deemed hopeless due to moderate-severe bone loss as seen in the initial panorex radiograph (Fig. 1). All teeth in question had significant recession, spacing, mobility, suppuration and were periodontally compromised (Figs. 2-4). The recommendation to remove them in favour of dental implants had been offered. The reason for multiple consultations surrounded the fate of an impacted canine (13) located in the palate which lay horizontal and impeded the placement of a number of implants in the area in question.
Fig. 1

Fig. 2

Fig. 3

Fig. 4

Initially the patient had been sent to see an orthodontist to explore exposure of the impacted tooth and extrusion into the appropriate arch position. The orthodontist had expressed concerns with whether the tooth may be ankylosed or if significant movement of this nature could be accomplished in a timely fashion if at all. It was felt in a best-case scenario it would take over a year to shift the tooth to the desired position.
Upon declining orthodontic therapy, the patient visited a dentist and oral surgeon whose recommendation was to surgically access and remove the impacted canine. The area would be augmented at the time of removal and a return approximately four to six months following the initial surgery to place the implants. Although this approach is performed routinely with relative ease and safety by experienced surgeons, the patient was strongly against undertaking the procedure and continued seeking alternative options.
Surgical Approach
The typical pre-operative protocol for implant therapy utilized in this practice involves prophylactic antibiotics starting one-day prior to surgery.12 In addition, pre-emptive Ibuprofen 600mg is administered immediately prior to the procedure in office as well as a 30 second rinse with Peridex mouthwash. The antibiotic would normally be taken for one week, until completion of the course and Ibuprofen taken as needed for pain and discomfort. In this specific instance the patient was a herbalist and unwilling to take any of the aforementioned pharmaceuticals.
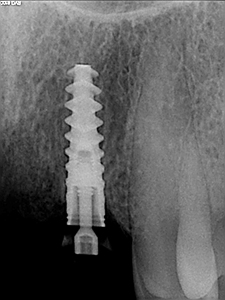
The patient was locally anesthetized using Lidocaine 2% (1:100 000 epinephrine). All teeth were removed atraumatically via elevation and forcep delivery. No flaps were reflected at the extraction sites so as to minimize invasion, not to disturb the blood supply/periosteum and reduce the risk of further blunted papilla. Thorough curettage was undertaken to remove any granulation tissue and irrigation to ensure that the sockets were sound. All implants were placed as per manufacturers instruction at 1500 RPM with abundant irrigation. Guide pins were used to confirm depth and angulation of the initial twist drill osteotomies (Figs. 5 & 6). Osteotomies were somewhat underprepared to ensure high torque values were reached in preparation for immediate temporization of the implants. All implants were placed initially by handpiece and to final depth with torque wrench achieving primary stability at all sties (>35ncm) (Figs. 7 & 8).
Fig. 5
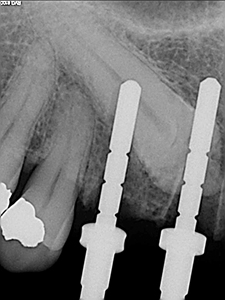
Fig. 6
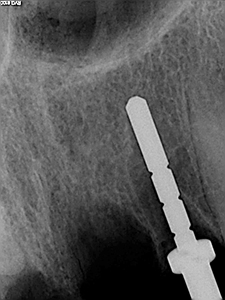
Fig. 7

Fig. 8
A lab fabricated provisional shell was then bonded to temporary abutments and then finished chairside by the referring dentist to ensure satisfactory shape, fit and contour. Occlusion was checked and adjusted accordingly to avoid trauma in excursive movements.
The patient was advised to refrain from biting into firm, tough foods in the area for the first two months and when possible to completely avoid function on the temporary bridge. A request to cut food and institute a softer diet in general was encouraged to minimize transmission of forces to the implants which were undergoing integration.
Results
The patient was seen at various intervals to evaluate post-operative healing and ensure the region was free of complication. The initial two-week visit involved visual evaluation to confirm absence of significant inflammation, edema or signs of infection including presence of exudate, lymphadenopathy, fever, malaise, fetid odour and foul taste. The patient reported no pain or discomfort even in the early healing phase following the surgery. No analgesics were required at any point following the procedure. The clinical healing mirrored the patients asymptomatic state and all appeared to be healing uneventfully. Close observation of the patient’s occlusion was undertaken and any necessary adjustments were performed to ensure clearance of the temporary prosthetic. Confirmation that the temporary was not mobile was also assessed. Reinstitution of normal hygiene protocols were reinforced to minimize plaque and food accumulation. Minimal function and softer diet were ongoing recommendations.
The patient was seen at subsequent two-month and four-month follow-up appointments which involved similar evaluation to the two-week protocol. In addition, radiographs were taken to assess bone levels and confirm appearance of integration. In both instances the radiographs displayed stable crestal bone and normal density and trabecular patterns. To be noted – no peri-apical lucency or issue seemed to be associated with the impacted canine which had been penetrated during osteotomy preparation and implant placement. The temporary prosthetic was removed at these appointments to view the implant collars, per-implant tissues, irrigate and percuss. Palatal palpation was consistently undertaken to ensure no formation of underlying abscess was occurring.
Following the four-month appointment the patient returned to the restorative doctor for impressions and subsequent restoration. The bridge work achieved acceptable esthetics and the patient was pleased with the outcome not only given his initial state but also considering the expedited protocols/minimal procedures required relative to traditional recommendations.
The patient was seen two months following insertion of the bridge work to ensure the tissues were well accepting of the restoration and no peri-implant inflammation existed. He was seen at six months following insertion and then annually thereafter. At these annual visits, xrays were prescribed and further clinical examination was performed to ensure peri-implant health was maintained.
The accompanying intra-oral photos (Figs. 9-12) and more importantly radiographs evidence stable healing over a two -year (Figs. 13-15) and five-year period (Figs. 16-18).
Fig. 9

Fig. 10

Fig. 11

Fig. 12

Fig. 13

Fig. 14

Fig. 15

Fig. 16
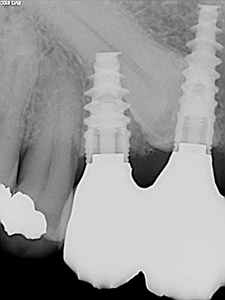
Fig. 17

Fig. 18

Discussion
It has long been presumed that true bone to implant contact must be achieved as a requisite for a dental implant to osseointegrate.1,13 Removal of remaining fibrous tissue or tooth fragments has been advocated as their presence is considered disruptive to this integrative process. Although extensive research has not been focused on the interaction of implants and teeth, a number of papers have emerged over the last decade exploring the plausible success of so-called dento-integration.
One of the first landmark studies by Hurzeler and Zuhr8 put forth the idea of intentionally maintaining a thin piece of tooth within the socket in an effort to optimize aesthetics and prevent buccal bone deformation following implant placement. Implants were placed immediately in these scenarios and the sub-field of partial extraction therapy (PET) was born. Since this proof of principle study many others have promoted this technique and it has not only become an accepted standard with high rates of success but to many considered superior to a traditional approach from an esthetic standpoint.8,14
A number of other studies9-11 in the same time period not only looked at portions of teeth being maintained rather the results of placement of implants through impacted teeth similar to this paper. Davarpanah9-11 and his group have put forth the most extensive body of evidence with a number of case series’ that follow placement of implants through impacted teeth in multiple regions of the mouth. Although their samples are not particularly large they show a high and similar success rate to those implants placed within the alveolar housing. Their cases have a moderate follow up and span from six months to eight years without complications or issues within the patient base. Unlike the current study, all implants were either submerged or healing abutments placed versus immediate temporization.
Although many would still opt for pre-emptive removal of the impacted tooth given its routine nature one must consider that in many instances such teeth can be ankylosed and the various challenges that come with exposure.15,16 In these cases removal is not performed with ease and can be quite traumatic involving removal of surrounding bone in order to facilitate exodontia. As a result, augmentative procedures involving bone grafting must be undertaken to regenerate the defect in preparation for subsequent implant placement. This not only increases the number of surgeries but also heightens morbidity, invasion, cost and longer duration of an edentulous state. All of these factors must be weighed when considering various treatment modalities.
There are still major questions surrounding the therapy being investigated Namely, what are the processes that allow for such integration to occur and how do patients seem void of symptoms or pulpal changes in the penetrated tooth? In terms of the integration process it would appear that formation of new bone occurs at the implant-dentin interface and between spaces where the tooth had been prepared for osteotomy (Fig. 19). It must be considered that these findings although being histologic are indeed from a beagle dog study.
Fig. 19

There are other animal studies17 which have shown development of an actual periodontal ligament at the implant-tooth interface but in these cases a gap or enlarged osteotomy was created whereas in this study under-preparation of osteotomies was employed to garner high torque and intimacy to the implant. It is therefore likely that the former findings from Hurzeler’s PET study are more applicable to the case in discussion.
From an endodontic standpoint one would expect pulpal necrosis and a subsequent periapical pathology to ensue. A number of thought processes have been proposed to explain the absence of such effects. In this case, the osteotomy was created at the coronal portion of the tooth. Similar to undertaking a partial pulpotomy it is possible that the apical portion of the pulp remained intact and viable.18 In a monkey model Warrer et al19 found when implants were drilled through teeth that the pulps remained unaffected after three months. One could also argue that because implant surgery is carried out in a sterile or “sterile-like” setting the ability for the oral cavity to contaminate the impacted tooth may be eluded and therefore infection could be prevented. Finally, when we look to the endodontic literature, Sabeti et al20 showed that when contamination was prevented, “periapical complications and root obturation can be avoided following endodontic therapy”.
Case Selection
One important piece to highlight when considering this procedure was appropriate case selection. Although obtaining consent for any dental treatment is crucial it becomes particularly paramount in circumstances where unconventional therapy is being offered to a patient. A thorough explanation of various options along with advantages, disadvantages and risks, benefits was undertaken. Amongst these options were no treatment or a removeable partial prosthetic. The patient was adamant not only to fill the to-be missing area but to have a fixed prosthetic. The restoring dentist deemed the span too long to offer a conventional bridge. Orthodontic extrusion was also briefly discussed but the patient declined.
Once the decision was made by the patient to pursue implant rehabilitation we moved to a more detailed discussion of various options. The suggested treatment was removal of the impacted canine followed by augmentation and a delayed return some months later once the bone had matured to place implants to restore the missing space from 13-22. The patient was adamant to avoid this process and so the discussion of the unconventional approach ensued. The patient was well aware that although this treatment was not experimental, it had limited evidence basis and track record. He was aware that not only may the implants be at higher risk for complication and failure but the impacted tooth could very well become necrotic, infected and necessitate removal. The patient completely understood the pros and cons and felt comfortable with the risks moving forward with therapy.
Conclusion & Commentary
Life long learning is paramount to ensure the highest standard of care in any profession. As dentists we commit ourselves with the task of keeping up with a fiercely ever-changing field. Through attending lectures, training and reading journals we attempt to maintain the pace of care. Within dentistry, implant technology is one of the fastest evolving and growing areas. For this reason, one must be careful not to become set in their ways or confined to a comfort zone out of ease. Being open to new modalities even when deemed unconventional is important to widen one’s repertoire. I can certainly imagine that when PI Branemark proposed the utilization of titanium screws in a human jaw to secure a proshthetic many were less than sold regardless of evidence shown in rabbit tibias and the orthopedic literature.
This beckons another important closing discussion. In my short career it has become painfully apparent that dentistry seems to be a cold, eat-our-own type of environment. Most are quick to judge others’ work or pitfalls giving little consideration to the specific situation that may have unfolded in the chair, patient challenges or discussions had. We mustn’t jump to throw others under the bus without understanding the full picture or story. I would imagine more readers grimaced than smiled when first laying eyes on the title of the article and seeing the radiographs within. One might assume such treatment could only be carried out by a “cowboy” or someone lacking knowledge or surgical prowess. In fact, that is exactly what another surgeon told this very patient when he inquired about the option. Had the surgeon ever delved into the literature, had he ever attempted a case himself? So why would he be quick to dismiss the feasibility? Who really was the negligent provider?
The placement of these implants through an impacted canine represents a path less taken but ultimately a high standard of care and success by any criteria especially the patient who was unwilling to consider the proposed traditional therapies. We should all be open to novel techniques that may aim to minimize invasion and morbidity while garnering case acceptance and expediting care to our patient base. More research is definitely warranted in this promising area of implantology.
Oral Health welcomes this original article.
Special thanks to Drs Vickie & James Sugarman for the restorative collaboration on this case.
References
- Branemark, P-I., B-O. Hansson, R. Adell, U. Breine, J. Lindstrom, O. Hallen, and A. Ohman. Osseointegrated implants in the treatment of the edentulous jaw. Scand. J. Plast. Reconstr. Surg. 11: Suppl. 16, 1977.
- Schnitman PA, Wöhrle PS, Rubenstein JE, DaSilva JD, Wang NH. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants 1997;12(4):495-503.
- Arisan, V., Bolukbasi, N., Ersanli, S., & Ozdemir, T. (2010). Evaluation of 316 narrow diameter implants followed for 5‐10 years: A clinical and radiographic retrospective study. Clinical Oral Implants Research, 21(3), 296–307.
- Salah Huwais, Eric G. Meyer. A Novel Osseous Densification Approach in Implant Osteotomy Preparation to Increase Biomechanical Primary Stability, Bone Mineral Density, and Bone-to-Implant Contact . Int J Oral Maxillofac Implants 2016; (10 pages)
- Annibali, S., Cristalli, M. P., Dell’Aquila, D., Bignozzi, I., La Monaca, G. & Pilloni, A. (2012) Short dental implants: a systematic review. Journal of Dental Research 91, 25–32.
- Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark system implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res 2003;5:2–9.
- Malo P, de Araújo Nobre M, Lopes A, Moss SM, Molina GJ. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc 2011;142:310–20.
- Hurzeler MB, Zuhr O, Schupbach P, Rebele SF, Emmanouilidis N, Fickl S. The socket-shield technique: a proof-of-principle report. J Clin Periodontol. 2010;37(9):855–862.
- Davarpanah M, Szmukler-Moncler S. Unconventional implant placement. I. Implant placement in contact with ankylosed root fragments. A series of 5 case reports. Clin Oral Implants Res. 2009; 20(8):851-856.
- Davarpanah M, Szmukler-Moncler S. Unconventional implant placement. II. Placement of implants through impacted teeth. A series of 5 case reports. Int J Perio Rest Dent 2009; 29(4): 405-413.
- 11. Davarpanah Mithridade , Szmukler-Moncler Serge, Davarpanah Keyvan, Capelle-Ouadah Nedjoua, Demurashvili Georgy, Rajzbaum Philippe. Unconventional Implant Placement IV. Implant Placement through Impacted Teeth to Avoid Invasive Surgery. Long-term Results of 3 Cases. J Open Dent. 2015 9:15-20.
- 12. Bodil Lund, Margareta Hultin, Sofia Tranæus, Aron Naimi‐Akbar, Björn Klinge. Complex systematic review ‐ Perioperative antibiotics in conjunction with dental implant placement. Clin Oral Implant Res. 2015; 26(11): 1-14.
- T. Albrektsson, P.I. Brånemark, H.A. Hansson, J. Lindström, Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-toimplant anchorage in man, Acta Orthop. Scand. 52 (2) (1981) 155–170.
- Gluckman H, Salama M, Toit JD. Partial Extraction Therapies (PET) part 1: maintaining alveolar ridge contour at pontic and immediate implant sites. Int J Periodontics Restorative Dent. 2016;36(5): 681–687.
- Orlando Motohiro Tanaka, Ana Letícia Rocha Avila, Ariel Adriano Reyes Pacheco, Matheus Melo Pithon.Four impacted canines in an adult patient: A challenge in orthodontics. Ind J Dent Res. 2014; 25(1):125-127.
- V.G. Kokich. Surgical and orthodontic management of impacted maxillary canines: J Ortho Dent Ortho. 2004; 126(3):278-283.
- Buser D, Warrer K, Karring T, Stich H. Titanium implants with a true periodontal ligament: An alternative to osseointegrat- ed implants? Int J Oral Maxillofac Implants 1990;5:113–116.
- Blanco L, Cohen S. Treatment of crown fractures with exposed pulps. J Calif Dent Assoc 2002;30:419–425.
- Warrer K, Karring T, Gotfredsen K. Periodontal ligament formation around different types of dental titanium implants. I. The self-tapping screw type implant sys- tem. J Periodontol 1993;64:29–34.
- Sabeti MA, Nekofar M, Motahhary P, Ghandi M, Simon JH. Healing of apical periodontitis after endodontic treatment with and without obturation in dogs. J Endod 2006;32:628–633.
About The Author
 Dr. Walton earned his Doctor of Dental Surgery degree from the University of Toronto. Prior to pursuit of his graduate dental studies, he completed externships at the University of Michigan and overseas at King’s College School of Medicine and Dentistry in London, England. Dr. Walton completed his Master’s degree in Periodontology at the Harvard School of Dental Medicine. His practice includes conventional periodontal therapy for tooth maintenance, periodontal plastics as well as advanced regenerative techniques and implant rehabilitation. His current area of focus lies in immediate implant placement and temporization for both single, multiple and full arch reconstruction.
Dr. Walton earned his Doctor of Dental Surgery degree from the University of Toronto. Prior to pursuit of his graduate dental studies, he completed externships at the University of Michigan and overseas at King’s College School of Medicine and Dentistry in London, England. Dr. Walton completed his Master’s degree in Periodontology at the Harvard School of Dental Medicine. His practice includes conventional periodontal therapy for tooth maintenance, periodontal plastics as well as advanced regenerative techniques and implant rehabilitation. His current area of focus lies in immediate implant placement and temporization for both single, multiple and full arch reconstruction.
Dr. Walton is a Fellow of the Royal College of Canada and a US Board Certified Diplomate of Periodontics and Implantolgy. He maintains an affiliation to University of Toronto, and Harvard as a clinical instructor, international research fellow, admissions committee member and active alumnus.
RELATED ARTICLE: When to Take a CBCT Scan for Implant Placement












