Maxillary implant prosthetic treatments may be considerably more difficult to accomplish when compared to the similar treatments for patients with edentulous mandibles due to many factors including bone quality, position of implants due to anatomical landmarks, need for grafting, prosthetic space needed, etc.
It is very important to assess a patient’s dental and medical history as well as bone quality and quantity and their impact on treatment success. In an ideal world, we would have a flowchart that would guide us to determine whether fixed or removable prostheses and how many implants would be enough for a particular patient in any given situation. However, implant success (biological or prosthetic) is very complex. Specific criteria and clinical guidelines should be identified for use in the treatment planning process. Determination of optimal implant positions and their relationships to residual ridges or extraction sites are one of the critical factors in determining designs for maxillary implant prostheses.
Prosthetic designs (fixed or removable) should be determined by clinicians prior to placing implants. The type of prosthesis the patient will be having, will determine the number and location of the implants, as well as bone augmentation or bone reduction. Also, material used for prosthesis should be determined based on opposing dentition, parafunctional habits of the patient, and other factors.
In this article, I tried to gather the most recent literature that will hopefully give us some insight to the best evidence-based treatment options that we can offer to our patients with edentulous maxillae.
1. Medical history
Most of the patients who are edentulous in one arch or both arches present with comorbidities. One common medical problem they present with is Diabetes Mellitus (DM). DM is not a risk factor for implant survival, but there is no information concerning appropriate perioperative management (medication) and wound closure. No much evidence exists in the literature for success of bone grafting procedures and progressive loading protocols in these patients.1,2
Low dose oral bisphosphonates (BP) intake for osteoporosis treatment does not compromise implant survival, but might cause MRONJ. High-dose of BP has led to the highest incidence of MRONJ, therefore implant treatment should not be advised in these patients.
In patients with comorbidities, the impact of specific, severe and even rare complications should be considered rather than implant survival.1,2
2. History of periodontal disease
Peri-implant inflammations represent serious diseases after dental implant treatment, which affect both the surrounding hard and soft tissue. Due to prevalence rates up to 56%, peri-implantitis can lead to the loss of the implant. Recall appointments with evaluation and elimination of risk factors (e.g. smoking, systemic diseases and periodontitis) are effective precautions.3
In periodontitis susceptible patients, residual pockets (≥ 5 mm) at the end of active periodontal therapy represent a significant risk for the development of peri-implantitis and implant loss than periodontally stable patients.4
For the treatment of peri-implant disease various conservative and surgical approaches are available. Mucositis and moderate forms of peri-implantitis can obviously be treated effectively using conservative methods such as manual ablations, laser-supported systems as well as photodynamic therapy, which may be extended by local or systemic antibiotics. In cases with advanced peri-implantitis surgical therapies are more effective than conservative approaches.
For patients with high risk of peri-implantitis, recommendation of 6 implants or more might be beneficial, since if one or more implants are lost, the patient can potentially continue to use the same prosthesis.3,4
3. Smoking
Many studies have shown that smokers are more prone to peri-implant bone loss and experience a higher rate of implant failure, especially in the maxillary arch. The overall bone loss over time is significantly higher in smoking patients, which might be suggestive for a higher peri-implantitis risk. Hence, smoking cessation should be advised and maintained after implant placement from the perspective of peri-implant disease prevention.5,6
4. Removable Implant Complete Denture versus Fixed Implant Complete Denture
a. Fixed Implant Complete Denture (FICD), also known as Fixed detachable or Hybrid prosthesis, is a common treatment recommended to patients with edentulous maxillae. Points to consider are number and type of implants, material of the prosthesis, size of the prosthesis. One popular treatment modality is the All-on-X protocol, where 4 or more implants are placed and during the same appointment a prosthesis is fastened to the implants.7 The main indication of All-On-X standard care is an atrophic maxilla or mandible, with or without remnant hopeless tooth. It is necessary for the implant to have had an insertion torque of over 35 Ncm for immediate loading. The provisional prosthesis should provide rigidity, being non-flexible in order to avoid micro-movements, and should be strong enough to not fracture.7 Fracture of the prosthesis is one of the main disadvantages to this option. A non-concave acrylic base resting over soft tissue is recommended, facilitating hygiene. Prosthetic complications occur as a result of fractures of the provisional acrylic prostheses.7 The protocol started with 4 implants, but many clinicians favour the use of more than 4, hence the name All-on-X. Various materials and different fabrication techniques are now available as alternatives to traditional cast metal frameworks, for full-arch implant-supported rehabilitations.7,8 Further long-term studies are needed to validate the use of these materials and clarify their specific clinical indications and manufacturing protocols to optimize their clinical outcomes. According to some studies, patients treated with FICD fabricated with milled titanium frameworks in the edentulous maxilla presented comparable results to patients with conventional cast frameworks after 2 years in function. Monolithic zirconia prosthesis is an alternative for cases where chipping of porcelain or acrylic might occur. It is important that even though zirconia is a strong material, we follow proper prosthesis design guidelines to prevent fracture.7-9
b. Removable Implant Complete Denture (RICD): For this modality, we can treat our patients with single abutments such as stock abutments (e.g. locators, ball, etc.) or custom abutments (e.g. Atlantis® Conus).10 Single attachments prosthesis offer a somewhat less expensive alternative compared to bar-overdentures RICD. Many studies have compared outcomes of maxillary implant overdentures retained by use of either locator attachments or bar overdentures.10-12 Bone loss tends to be in an acceptable range for both groups after 1 year. However, less bone seems to be lost in the bar group. Both treatment options improve patient satisfaction. Prostheses with single abutments seem to be advantageous for their convenient cleaning and repair. In some studies, the locator system produced superior clinical results compared with the bar attachments in terms of peri-implant hygiene parameters, the frequency of prosthodontic maintenance measures, cost, and ease of denture preparation.10-12 However, longer-term prospective studies are required to confirm results.
5. Limited bone in the maxilla:
a. Sinus grafting versus short implants: Insufficient bone volume is a common problem encountered in the rehabilitation of the edentulous posterior maxilla with implant-supported prostheses. Bone volume is limited by the presence of the maxillary sinus together with loss of alveolar bone height. Sinus lift procedures increase bone volume by augmenting the sinus cavity with autogenous bone or commercially available biomaterials, or both.13 There is moderate quality evidence which is insufficient to determine whether sinus lift procedures in bone with residual height between 4 and 9 mm are more or less successful than placing short implants (5 to 8.5 mm) in reducing prosthesis or implant failure.13,14 However, there are more complications at sites treated with sinus lift procedures. Many trials have compared different sinus lift procedures and none of these indicated that one procedure reduced prosthetic or implant failures when compared to the other.
For atrophic posterior maxilla, short implants (≤6 mm) are a promising alternative to sinus floor elevation, with comparable survival rate and post-surgery reactions, but additional high-quality studies are needed to evaluate their long-term effectiveness. There seems to be no significant difference in implant survival rate and marginal bone resorption recorded for both the short implant and long implant with sinus graft. Hence, short implant is a suitable alternative to long implant with sinus graft, for the rehabilitation of posterior atrophic maxilla.15
b. Zygomatic implants: Zygomatic implant rehabilitation has demonstrated to be a reliable method with good mid-term results. The occurrence of post-surgical adverse events and need for laboratory repair of the prosthesis were found to be significant risk factors for implant loss. These risk factors may be prevented by means of detailed planning of the rehabilitation to be carried out, including post-operative care of the patients, so that treatment success using zygomatic implants can be achieved.16
c. Tilting posterior implants: In the immediately loaded rehabilitation of completely edentulous atrophic maxilla, tilting of implants did not induce any significant alteration in their survival and their corresponding marginal bone loss levels compared to conventionally placed axial implants after three years of function.17
6. How many implants should we place?
The number of implants required to support a maxillary overdenture in order to obtain optimal treatment outcomes in terms of implant survival, overdenture longevity and patient satisfaction still remains a controversial issue. The most frequent tendency is to place at least four implants, splinted or unsplinted. The survival rate of implants appears to be higher when at least four implants are placed to support the overdenture, compared to less than four implants. The survival rate of overdentures and the patient satisfaction are not influenced by the number of implants.18
An implant-supported maxillary overdenture (all studies ≥ 4 implants) provided with a splinted anchorage is accompanied with a high implant and overdenture survival rate, while there is an increased risk of implant loss when ≤ 4 implants with a non-splinted anchorage are used.18,19
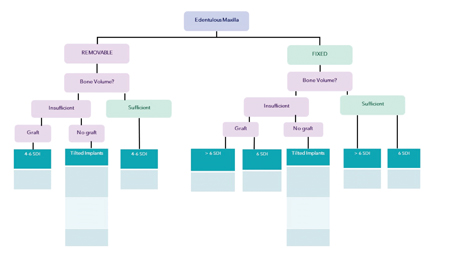
A very useful Decision Tree Chart was included in a Consensus Report on Recommendations for Implants supported full arch rehabilitations in edentulous patients published this year in the International Journal of Prosthodontics. (Fig. 1) This chart guides how many implants would be needed in a given situation whether we are providing the patient with either FICD or RICD, whether the patients were grafted or not.19
Fig. 1
7. Does opposing dentition play an important role?
There is moderate certainty of evidence, natural maxillary dentitions opposed to FICD do not affect long term survival rates differently than other maxillary prosthetic designs, such as removable partial dentures or removable implant prosthesis; however, natural dentition or fixed restorations as an antagonist may increase the risk of technical complications.19
8. What is the amount of bone reduction needed for FICD and RICD?
Based on the minimum material thickness required to achieve good mechanical stability, it is recommended that for single attachments prosthesis to have at least 10 to 11 mm vertical distance from implant platform to incisal edge of the prosthesis; and for fixed complete dentures or bar overdenture to have at least 15-17 mm vertical distance from the implant platform level to the incisal edge. This is a very important consideration since substantial bone reduction might need to be done before placement of implants, depending on the type of prosthesis/substructure selected.19
9. Should I be concerned with patients with parafunction?
Despite the documented excellent clinical performance of dental implants, concerns linger regarding the best way to protect the restored dentition in patients with bruxism. To better distribute occlusal loads to the rigid components of the prosthesis and to the interface between bone and implant during parafunctional movements, several dentists prescribe acrylic resin occlusal splints for nocturnal use by patients considered at risk. This recommendation is based mostly on expert clinical opinion. Other option available for the heavy bruxer is the use of botulinum toxin injections in the masticatory muscles, although there is conflicting evidence showing reduction in bruxism.20
10. Commitment to recall
Many studies have shown that it is the maintenance of periodontal health rather than a previous history of periodontitis that is the critical determinant of increased risk of peri-implantitis, highlighting the importance of effective periodontal therapy and maintenance in patients with a history of periodontitis.3,4,19 We need to stress this out to our patients who are seeking replacement of teeth with implants. Frequency of recall and maintenance appointments will vary depending on the patient’s oral hygiene, and other factors such as dexterity, xerostomia, smoking, etc.3,4,19
It is not possible to assess whether prosthetic design (removable or fixed), time of loading (immediate or conventional), implant location (maxilla or mandible), implant site grafting, or time of implant placement have any influence on the occurrence of peri-implant disease in patients restored with full arch, implant supported restorations.
Finally, it has been shown in different studies that establishing a sufficient amount of keratinized tissue along with full arch fixed/removable prostheses maintain peri-implant health.19
After reviewing the literature, some conclusions for treating planning a prosthesis for the edentulous maxilla are:
- Patient information about complications and treatment options must be thoroughly presented and discussed. General health of the patient is critical, including extreme frailty, mental disability, periodontitis, smoking history, and xerostomia.
- Four to six implants should be considered necessary for fixed and removable prosthesis in the edentulous maxilla to achieve support, and these should be distributed across the arch. Distribution of the implants in the arch will mandate the amount of posterior cantilever of the prosthesis.
- In cases of fixed prosthesis, 4 axial implants in the anterior and two tilted implants in the posterior region are an alternative to bone grafting. Zygomatic implants and short implants should also be considered instead of bone grafting since the complication rate is expected to be similar to standard implants.
- In cases where both removable and fixed treatment options are indicated, patient expectations and cost should be the determining factors for selecting a treatment modality.
- Natural dentition or fixed implant restorations as an antagonist may increase the risk of technical complications presumably due to higher occlusal forces.
- FICD revealed higher survival rates but also high technical complications. Chipping was one of the major complications for bilayered prostheses, such as metal ceramic, metallic-acrylic and veneered ZrO2. Use of high strength ZrO2 is a promising alternative for FICD.
- Limited prosthetic space may be considered as a reason for increased risk of failure of the prosthesis.
- The design of abutments, or suprastructures should consider plaque retention as a factor for inducing mucositis and peri-implantitis.
- A lack of keratinized gingiva around the implants (<2 mm) was also associated with a higher rate of biologic complications.
- Implant overdentures make it easier to maintain oral hygiene and also allows proper assessment of implants by the clinician. We should take this into account when discussing options with elderly patients with disabilities or dexterity problems.
For maxillary overdenture therapy, proper treatment guidelines are missing. There is a need for longitudinal studies comparing all the different parameters mentioned.
Inherent differences between fixed and removable prosthetic treatments are critical for clinicians to understand, as they often include key points for clinicians explaining the features of fixed/removable-implant prostheses to patients. Cases 1-7 show different treatment modalities for the edentulous maxilla for some of my patients.
Case 1
Overdenture retained by 4 SDI, with free standing abutments (Locators). The patient did not require bone grafting. Natural opposing dentition with a conventional removable partial denture.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Case 2
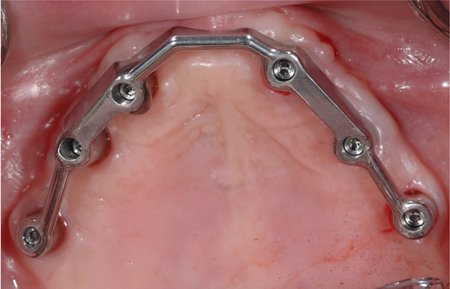
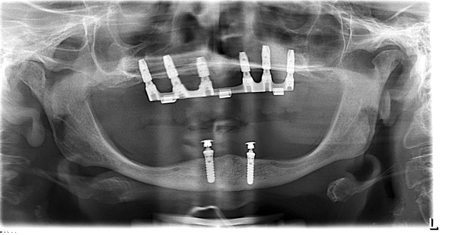
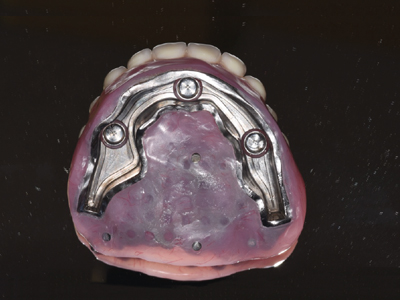
Overdenture retained by 6 SDI, splinted with a Hader bar. The patient did require bone grafting. Opposing dentition is a 2 implant overdenture.
Fig. 1
Fig. 2
Case 3
Double structure overdenture (obturator) retained by 1 SDI and 3 zygomatic implants. Implants splinted with a milled locator bar with free standing abutments. Bone was insufficient, but the patient did not have bone grafting. Opposing natural dentition with 2 implant crowns.
Fig 1
Fig. 2
Fig. 3
Fig. 4
Case 4
One-piece Fixed Complete Denture retained by 6 SDI. Prosthesis fabricated with porcelain fused to metal substructure. The patient required autogenous bone grafting before implant placement. Opposing natural partial dentition (soon to be rehabilitated).
Fig 1
Fig. 2
Fig. 3
Fig. 4
Case 5
One-piece Fixed Complete Denture retained by 6 SDI: 4 anterior axial and 2 posterior distally tilted implants. Prosthesis fabricated with monolithic zirconia. The patient had insufficient bone in the posterior region but no grafting was done. Opposing natural dentition.
Fig. 1
Fig. 2
Fig. 3
Case 6
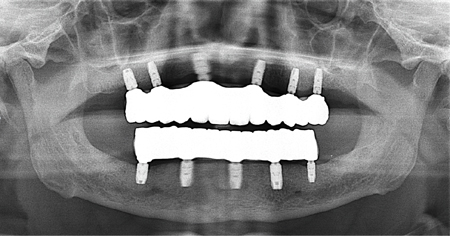
One-piece Fixed Complete Denture retained by 6 SDI. Prosthesis fabricated with monolithic zirconia. The patient had sufficient bone in both anterior and posterior regions. Opposing fixed implant-retained dentition, also in zirconia.
Fig. 1
Fig. 2
Fig. 3
Case 7
Three Fixed Partial Dentures retained by 7 SDI. Prostheses fabricated with porcelain fused to metal. The patient had insufficient bone in the posterior and some grafting was done. Opposing natural dentition with 3 implant crowns and a FPD implant supported.
Fig. 1
Fig. 2
Appreciation of the differences between fixed and removable prostheses is critical for patients and clinicians to make informed decisions. Also, educating patients on how their oral anatomy, medical history, habits and commitment to recall will have an impact on the long term success of their prosthesis.
Oral Health welcomes this original article.
References
- Messias A, Nicolau P, Guerra F. Different Interventions for Rehabilitation of the Edentulous Maxilla with Implant-Supported Prostheses: An Overview of Systematic Reviews. Int J Prosthodont. 2021 Suppl;34:s63-s84.
- Drago C, Carpentieri J. Treatment of maxillary jaws with dental implants: guidelines for treatment. J Prosthodont. 2011 Jul;20(5):336-47.
- Smeets R, Henningsen A, Jung O, Heiland M, Hammächer C, Stein JM. Definition, etiology, prevention and treatment of peri-implantitis—a review. Head Face Med. 2014 Sep 3;10:34.
- Pjetursson BE, Helbling C, Weber HP, Matuliene G, Salvi GE, Brägger U, Schmidlin K, Zwahlen M, Lang NP. Peri-implantitis susceptibility as it relates to periodontal therapy and supportive care. Clin Oral Implants Res. 2012 Jul;23(7):888-94.
- Windael S, Vervaeke S, De Buyser S, De Bruyn H, Collaert B. The Long-Term Effect of Smoking on 10 Years’ Survival and Success of Dental Implants: A Prospective Analysis of 453 Implants in a Non-University Setting. J Clin Med. 2020 Apr 8;9(4):1056.
- Hadadi AA, Mezied MS. Evidence-based analysis of the effect of smoking on osseointegrated implant outcome. Natl J Maxillofac Surg. 2021 May-Aug;12(2):133-138.
- Penarrocha-Diago M, Penarrocha-Diago M, Zaragozí-Alonso R, Soto-Penaloza D, On Behalf Of The Ticare Consensus M. Consensus statements and clinical recommendations on treatment indications, surgical procedures, prosthetic protocols and complications following All-On-4 standard treatment. 9th Mozo-Grau Ticare Conference in Quintanilla, Spain. J Clin Exp Dent. 2017 May 1;9(5):e712-e715.
- Jemt T, Bergendal B, Arvidsson K, Bergendal T, Karlsson U, Linden B, Palmqvist S, Rundcrantz T, Bergström C. Laser-welded titanium frameworks supported by implants in the edentulous maxilla: a 2-year prospective multicenter study. Int J Prosthodont. 1998 Nov-Dec;11(6):551-7.
- Delucchi F, De Giovanni E, Pesce P, Bagnasco F, Pera F, Baldi D, Menini M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials (Basel). 2021 Jun 12;14(12):3251. doi: 10.3390/ma14123251. PMID: 34204681; PMCID: PMC8231547.
- Lian M, Zhao K, Wang F, Huang W, Zhang X, Wu Y. Stud vs Bar Attachments for Maxillary Four-Implant-Supported Overdentures: 3- to 9-year Results from a Retrospective Study. Int J Oral Maxillofac Implants. 2019 July/August;34(4):936–946.
- Zou D, Wu Y, Huang W, Wang F, Wang S, Zhang Z, Zhang Z. A 3-year prospective clinical study of telescopic crown, bar, and locator attachments for removable four implant-supported maxillary overdentures. Int J Prosthodont. 2013 Nov-Dec;26(6):566-73.
- Boven GC, Meijer HJA, Vissink A, Raghoebar GM. Maxillary implant overdentures retained by use of bars or locator attachments: 1-year findings from a randomized controlled trial. J Prosthodont Res. 2020 Jan;64(1):26-33.
- Esposito M, Felice P, Worthington HV. Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Database Syst Rev. 2014 May 13;(5).
- Chaware SH, Thakare V, Chaudhary R, Jankar A, Thakkar S, Borse S. The rehabilitation of posterior atrophic maxilla by using the graftless option of short implant versus conventional long implant with sinus graft: A systematic review and meta-analysis of randomized controlled clinical trial. J Indian Prosthodont Soc. 2021 Jan-Mar;21(1):28-44.
- Yan Q, Wu X, Su M, Hua F, Shi B. Short implants (≤6 mm) versus longer implants with sinus floor elevation in atrophic posterior maxilla: a systematic review and meta-analysis. BMJ Open. 2019 Oct 28;9(10).
- Padovan LEM, Suzuki D, Kluppel LE, Vianna CP, Caldas W, Trojan LC. Factors influencing implant and prosthesis survival in zygomatic implant-supported fixed rehabilitation: a retrospective study. Odontology. 2021 Oct;109(4):965-972.
- Mehta SP, Sutariya PV, Pathan MR, Upadhyay HH, Patel SR, Kantharia NDG. Clinical success between tilted and axial implants in edentulous maxilla: A systematic review and meta-analysis. J Indian Prosthodont Soc. 2021 Jul-Sep;21(3):217-228.
- Raghoebar GM, Meijer HJ, Slot W, Slater JJ, Vissink A. A systematic review of implant-supported overdentures in the edentulous maxilla, compared to the mandible: how many implants? Eur J Oral Implantol. 2014 Summer;7 Suppl 2:S191-201.
- Schwarz F, Schär A, Nelson K, Fretwurst T, Flügge T, Ramanauskaite A, Trimpou G, Sailer I, Karasan D, Fehmer V, Guerra F, Messias A, Nicolau P, Chochlidakis K, Tsigarida A, Kernen F, Taylor T, Vazouras K, Herklotz I, Sader R. Recommendations for Implant-Supported Full-Arch Rehabilitations in Edentulous Patients: The Oral Reconstruction Foundation Consensus Report. Int J Prosthodont. 2021 Suppl;34:s8-s20.
- Mesko ME, Almeida RC, Porto JA, Koller CD, da Rosa WL, Boscato N. Should occlusal splints be a routine prescription for diagnosed bruxers undergoing implant therapy? Int J Prosthodont. 2014 May-Jun;27(3):201-3.
About the Author
 Dr. Aragon is a Prosthodontist who maintains a full-time private practice in London, Canada. She is an Adjunct Clinical Professor at the Schulich School of Dentistry and a Lecturer at the Faculty of Dentistry at the University of Toronto. She is also a Staff member at the Thames Valley Children’s Centre. E-mail: doctor@aragonprosthodontics.com www.aragonprosthodontics.com
Dr. Aragon is a Prosthodontist who maintains a full-time private practice in London, Canada. She is an Adjunct Clinical Professor at the Schulich School of Dentistry and a Lecturer at the Faculty of Dentistry at the University of Toronto. She is also a Staff member at the Thames Valley Children’s Centre. E-mail: doctor@aragonprosthodontics.com www.aragonprosthodontics.com