Introduction
Rehabilitation of completely edentulous maxillary and mandibular arches should satisfy form, function and esthetics. Such rehabilitations can be carried out either with or without implants. Although contemporary rehabilitation of completely edentulous situations is inclining towards dental implants, the demand for conventional removable prosthodontics is still high owing to surgical, economic and patient’s medical limitations.
Literature has shown patients’ dissatisfaction with removable complete dentures is essentially related to loss of retention (85,9%).1,2 Furthermore, it has been found that the key factor for patients’ satisfaction is a clinically stable mandibular denture.3,4,5 Achieving stability in ridges which are severely atrophied may be challenging.
Occlusion plays a pivotal role in achieving ideal stability for dentures in addition to retention, and support.6 It is defined as static relationship between the incisive and the masticatory surfaces of the maxillary and mandibular teeth or analogues of teeth (GPT-9). Although, there are various occlusal schemes that a dentist can choose from when rehabilitating completely edentulous situations with atrophied ridges, not all schemes satisfy esthetics. For example, concepts like the neurocentric occlusion or the monoplane occlusal scheme lacks the necessary esthetics when put to function. Lingualized occlusion on the other hand is a popular occlusal scheme that not only is indicated in severely atrophied ridges, but also satisfies form, function and esthetics for dentures. In addition to all these, proper lab communication also plays a key role in establishing a satisfactory esthetic outcome. With the advent of Digital smile designing and dental photography, dental technicians are given ample information to achieve best esthetics.
This article is a case presentation on a complete denture rehabilitation for a severely atrophied mandibular ridge opposing a moderately resorbed maxillary ridge.
Case report:
A 60-year-old Female patient had reported to the office with a chief complaint of dissatisfied old complete dentures. She was classified as ASA type 1 wearing complete dentures for the past 15 years. Facial assessment with her existing dentures revealed a loss of vertical dimension with decreased lower third of her face along with lack of labial fullness and no incisal visibility. Existing dentures lacked retention, stability and had a worn down acrylic cuspal morphology. Intra-oral assessment revealed a severely atrophied mandibular ridge (Atwood class IV bilateral posterior region and Class V in the interforaminal anterior region). Maxillary ridge was moderately resorbed with a U-shaped arch. Figs. 1,2 Soft palate was favorable with a Class 1 (House) palatal throat form and a normal resting tongue position. Favorable undercuts were present in maxillary anterior region and bilateral retromylohyoid region.
Fig. 1

Fig. 2

The patient was informed of all the possible treatment modalities available; since she could not afford implant treatment, rehabilitation with conventional complete dentures was considered.
Preliminary impressions were recorded using an Irreversible hydrocolloid (Alginate) Patterson Algitec Alginate Impression Material-Regular set. A customized tray design was proposed to follow the principle of selective pressure technique employing Boucher’s spacer design incorporated with tissue stops.
Final impression technique: Custom trays were assessed clinically for its fit and clearance. Border molding was carried out using Heavy Body PVS- Single step Border molding (Exafast NDS GC America) and final wash impression was made using Light Body Consistency PVS (Genie VPS impression material). Fig. 3 Master cast was obtained and acrylic record base and occlusal rims were fabricated.
Fig. 3

Jaw relation and facebow transfer: During Jaw relation appointment, the occlusal rims in the maxillary arch were adjusted according to the esthetic principles. Photographs were taken to carry out 2D Virtual Smile design using Adobe Photoshop CC software. First photograph was taken to visualize the amount of incisal exposure at rest. Fig. 4 Another image was taken to visualize the amount of occlusal rim visibility when posing a broad smile. Fig. 5 The reference lines, namely, midline, low lip line, high smile line and canine lines were marked on the wax occlusal rims. In the region of central incisors, the vertical length from the edge of the occlusal rims to the high smile line was 12mm. And the intercanine arch length was 46 mm in the occlusal rims. These measurements help in calibrating the rulers in Adobe photoshop software. 2d Frontal smile design was carried out with a triangular mold teeth form templates to fit within the measurements. The smile design was shown digitally to the patient and she was satisfied with the esthetic proposal. Figs. 6,7 In the meanwhile, Lower occlusal rims were seated and adjusted to achieve the desired Vertical and horizontal relation. Finally, Orientation jaw relation was recorded using Hanau Springbow and the models were mounted in a Semi-adjustable articulator (Hanau Wide Vue II) for further teeth arrangement. Fig. 8
Fig. 4

Fig. 5

Fig. 6

Fig. 7

Fig. 8

The denture technician was then communicated clearly with necessary pictures, 2D digital smile design and the desired type of occlusion. Based on the Virtual Smile Design assessment, measurements on the occlusal rims, face shape and arch shape a triangular mold from Vita Physiodens T6L was used for anteriors. As the occlusion was planned for a Lingualized set up, corresponding Vitapan linguoform teeth mold were used for complete set-up. The occlusal contacts were centralized in the occlusal fossa of the lower arch confining to the principles of Lingualized set up. Figs. 9,10
Fig. 9

Fig. 10
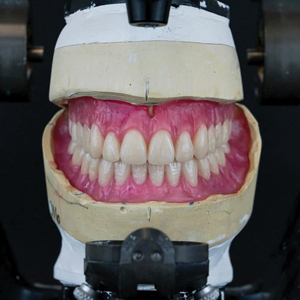
During try-in appointment, patient’s desired esthetic requirements and phonetics were checked along with the verification of jaw relation. Fig. 11 The final dentures were processed using injection molding process. Figs. 12,13,14 The occlusion was verified during denture insertion appointment where an ideal lingualized occlusal contacts were established. Figs 15, 16 After 24 hours, first follow-up showed minor sore spots near the retro-mylohyoid region and denture adjustment was done. 1 week follow-up, revealed no other sore spots and the patient was completely satisfied with the esthetics, retention and stability of her new dentures. Figs. 17,18
Fig. 11

Fig. 12

Fig. 13

Fig. 14

Fig. 15

Fig. 16

Fig. 17

Fig. 18

Discussion:
Management of resorbed ridges is difficult especially in atrophic mandible because of smaller denture bearing area than maxillary ridge and other anatomical limitations. Careful treatment planning and execution is important to achieve success in such rehabilitations. It all starts with an ideal impression which acts as the foundation for any successful prosthesis.
Although there are many theories of impressions for complete denture fabrication, the philosophy employed in this case was based on selective pressure theory proposed by Boucher. It is fundamentally based on loading the denture bearing areas that can withstand pressure and relieving areas that cannot withstand the functional load.7 The concept of selectively applying pressure is based on the variance in histology of the denture bearing mucosa.8 There are numerous customized tray designs proposed to follow the principle of selective pressure technique. The present technique follows Boucher’s concept of spacer design, of placing 1 mm baseplate wax all over the maxilla except the posterior palatal seal area and Sharry’s concept of placing four tissue stops in the molar and cuspid region.0 Similarly for the mandibular arch a 1mm wax spacer was placed in the entire crest portion of the ridge except retromolar pad and buccal shelf area as they act as the stress bearing areas.10
Elastomeric impression material has the advantage of single step border molding using heavy body consistency PVS and accurately recording the minute details during final impression using light body consistency PVS as employed in this case. In literature, various authors have recommended the use of elastomeric impression materials for border molding and final impressions. Lu et al.11 and Applebaum et al.12 concluded that polyvinylsiloxane impression materials are well suited for making complete denture impressions.
Prosthodontic rehabilitation is a team effort involving the patient, dentist, assistants and technician. Without proper co-ordination the outcome might not be as expected. In this case, the 2D smile design gave all the necessary information like the form of her required teeth, the expected anterior teeth arrangement visualized along with her smile curve, and her lip dynamics and ease of choosing the artificial teeth from mold chart. The technician had a clear perspective as to what he is expected to do in this rehabilitation. When such clarity is lacking, the chances for repeated try-ins are high especially from an esthetic stand point. This might cause unnecessary frustration to the dentist, technician and the patient. A virtual design will definitely make the patient comfortable and aware on what to expect during their esthetic try-in. Similarly, the technician can easily choose the artificial teeth mold and the design can help him arrange the anterior teeth accordingly. Also, the dentist can visualize the treatment outcome with a virtual design and gives him clarity in choosing the desired characterizations. Overall, this digital tool helps to bridge the communication between the team members.
The software employed by the author Adobe Photoshop CC is a versatile photo editing software that can be put to maximum use in dentistry for designing a smile digitally and planning a case for an esthetic smile makeover. The software is readily available and simple to use for clinicians, and, in the authors’ experience, results can be obtained that are comparable to other smile designing software programs. Digital rulers built in to the software to measure the distance to point accuracy are an added feature. However, calibration needs to be done to the desired measurement scale (either in “mm” or in “cm”).13
There are numerous occlusal schemes for complete denture rehabilitation for atrophied ridges. The choice of lingualized occlusion can be justified based on the fact that they satisfy esthetics along with form and function. This concept was first introduced by Gysi in 1927. His arrangement showed linear cusps of maxillary artificial teeth entering in contact with shallow mandibular teeth depressions.14,15 Later on, Payne in 1941 used a 30-degree maxillary tooth to attain a Lingualized occlusion on shallow mandibular depressions. These mandibular teeth had no cuspal morphology.16 With the advancement in artificial teeth choices over time, Pound used a similar set up as explained by Payne with the use of a 20 degree semi anatomic teeth for the mandibular arch in addition to 30-degree maxillary teeth.17,18 The cuspal forms used in this case is similar to the one proposed by Pound.
Some of the main advantages19,20 of this scheme are:
- Aesthetics and function are combined in this occlusal scheme
- Mandibular teeth centralize vertical forces as the palatal cusps of maxillary teeth rests on the central fossae of mandibular posteriors.
- Better food bolus penetration
- When bilateral balanced occlusion is used with Lingualized occlusion (Lingualized Balanced Occlusion), it provides more stability and favorable stress distribution in parafunction and excursive movements than balanced occlusion alone.
Conclusion:
Lingualized occlusion has been advocated and effectively followed by many practitioners especially with the availability of various acrylic tooth molds. The author’s experience has supported this concept and seems appropriate to use digital tools to enhance the desired esthetic outcome in addition to the benefits of controlling force distribution for better retention and stability using this occlusal concept.
Oral Health welcomes this original article.
Acknowledgement: The author would like to acknowledge Jeffrey M Luk, RDT, Shawlabgroup GTA for his lab expertise. The prosthodontic outcome of this case would not have been possible without the teamwork.
References
- Bilhan H, Geckili O, Ergin S, Erdogan O, Ates G. Evaluation of satisfaction and complications in patients with existing complete dentures. J Oral Sci 2013; 55(1):29–37, http://dx.doi.org/10.2334/josnusd.55.29.
- Bilhan H, Geckili O, Ergin S, Erdogan O, Ates G. Complication rates and patient satisfaction with removable dentures. J Adv Prosthodont 2012;4(2):109, http://dx.doi.org/10.4047/jap.2012.4.2.109.
- Alfadda SA. The relationship between various parameters of complete denture quality and patients’ satisfaction. J Am Dent Assoc 2014;145(9):941–8, http://dx.doi.org/10.14219/jada.2013.48.
- Fenlon MR, Sherriff M. Investigation of new complete denture quality and patients’ satisfaction with and use of dentures after two years. J Dent 2004;32(4):327–33, http://dx.doi.org/10.1016/j.jdent.2004.01.007.
- Anastassiadou V, Robin Heath M. The effect of denture quality attributes on satisfaction and eating difficulties. Gerodontology 2006;23(1):23–32, http://dx.doi.org/10.1111/j.1741-2358.2006.00094.x
- Lang BR. Complete denture occlusion. Dent Clin North Am 2004;48(3):641–65, http://dx.doi.org/10.1016/j.cden.2004.03.006
- Duncan JP, Raghavendra S, Taylor TD, A selective-pressure impression technique for the edentulous maxilla J Prosthet Dent 2004 92(3): 299-301.10.1016/j.prosdent.2004.06.00115343168.
- Jacobson TE, Krol AJ, A contemporary review of the factors involved complete dentures. Part III: Support J Prosthet Dent 1983 49(3):306-13.10.1016/0022-3913(83)90267-6.
- Shetty S, Nag PVR, Shenoy K, The selective pressure maxillary impression: A review of the techniques and presentation of an alternate custom tray design J Indian Prosthodont Soc 2007 7(1):08-11.10.4103/0972-4052.32509.
- Jain AR, Dhanraj M (2016) A Clinical Review of Spacer Design for Conventional Complete Denture. Biol Med (Aligarh) 8: 307. doi: 10.4172/0974-8369.1000307.
- H. Lu, B. Nguyen, and J. M. Powers, “Mechanical properties of 3 hydrophilic addition silicone and polyether elastomeric impression materials,” The Journal of Prosthetic Dentistry, vol. 92, no. 2, pp. 151–154, 2004.
- E. M. Applebaum and R. V. Mehra, “Clinical evaluation of polyvinylsiloxane for complete denture impressions,” The Journal of Prosthetic Dentistry, vol. 52, no. 4, pp. 537–539, 1984.
- Manoj Kumar Sundar, Venkataraman Chelliah. Ten Steps to Create Virtual Smile Design Templates with Adobe Photoshop® CS6 Compend Contin Educ Dent. 2018 Mar;39(3): e4-e8.
- Savitha K, Srinivas L. Occlusal schemes for complete dentures—a review article. Bhavnagar Univ J Dent 2013;3(1):67–72.
- Gysi A. Special teeth for cross-bite cases. Dent Digest 1927; 33:167–71.
- Phoenix RD, Engelmeier RL. Lingualized occlusion revisited. J Prosthet Dent 2010;104(5):342–6, http://dx.doi.org/10.1016/S0022-3913(10)60153-9
- Pound E. Personalized denture procedures. Anaheim: Denar Corp; 1973.p.4.
- Pound E. Utilizing speech to simplify a personalized denture service. J Prosthet Dent 1970;24(6):586–600.
- Becker CM, Swoope CC, Guckes AD. Lingualized occlusion for removable prosthodontics. J Prosthet Dent 1977;38(6):601–8.
- Gronas DG, Stout CJ. Lineal occlusion concepts for complete dentures. J Prosthet Dent 1974;32(2):122–9.
About the Author
 Dr. Manoj Kumar Sundar graduated from Dr.MGR Medical University, Tamil Nadu, India and went on to complete his Masters in Prosthodontics from Rajiv Gandhi University of Health Sciences, Karnataka, India. He is a DSD member, Fellow and Master–International Congress of Oral Implantologists, Member of American Academy of Implant Dentistry and ITI. He has published several articles in peer-reviewed journals, such as the Journal of Prosthodontic Research, Compendium of Continuing Education in Dentistry etc. He currently practices as a General dentist in Toronto, Ontario with special interest towards complex prosthodontic rehabilitation, smile designs and implant dentistry. Email: manojs87@gmail.com
Dr. Manoj Kumar Sundar graduated from Dr.MGR Medical University, Tamil Nadu, India and went on to complete his Masters in Prosthodontics from Rajiv Gandhi University of Health Sciences, Karnataka, India. He is a DSD member, Fellow and Master–International Congress of Oral Implantologists, Member of American Academy of Implant Dentistry and ITI. He has published several articles in peer-reviewed journals, such as the Journal of Prosthodontic Research, Compendium of Continuing Education in Dentistry etc. He currently practices as a General dentist in Toronto, Ontario with special interest towards complex prosthodontic rehabilitation, smile designs and implant dentistry. Email: manojs87@gmail.com
RELATED ARTICLE: Management of a 12-Year-Old-Male with a Class III Malocclusion and Canine Impaction












