An accurate endodontic diagnosis is based on a variety of clinical tests, including thermal and electric pulp testing, percussion, bite stick, periodontal probing, and palpation. However, each of these subjective tests is prone to both false positive and false negative responses that could result in the inability to get an accurate diagnosis or the treatment of an incorrect tooth. As a result, many clinicians place an undo amount of importance on radiographic imaging. Unfortunately, the diagnostic information gained by periapical imaging is also limited by subjective interpretation as clinicians do not agree about radiographic findings.1
Historically, as film speeds increased, there was a decrease in radiation exposure to the patient but no improvement in overall image quality. With the transition to digital imaging, radiation was further reduced, and workflow was improved because the computer eliminated the need for image development. But again, the diagnostic quality of the image was not improved. With traditional imaging, a periapical radiolucency may not be visible until the lesion is 7 mm in size and contacts the cortical plate of bone.2,3 Additionally, the ability to detect a periapical lesion with traditional imaging is influenced by tooth location and the resulting thickness of the cortical plate.4 Clinically, this means it is more difficult to see a radiolucency at the root end of a mandibular molar than at the apex of a lateral incisor.
To improve image quality and diagnostic accuracy, cone beam computerized tomography (CBCT) was introduced into the North American dental market in the early 2000s, but it didn’t gain widespread popularity for the better part of a decade. As the name implies, a cone-shaped X-ray beam is generated as the scanner rotates around the patient. A computer algorithm then reconstructs the data into a three-dimensional data set for interpretation. A small field of view CBCT is the imaging modality of choice for diagnosis in patients who present with contradictory or nonspecific clinical signs and symptoms associated with untreated or previously endodontically treated teeth.5 The volume of information generated by a scan takes considerable time to evaluate, incidental findings are common, and the hardware is expensive.
Although the amount of information generated from a CBCT volume can positively influence diagnosis and treatment planning, CBCT is associated with a higher radiation dose, metal artifacts, and scatter, which limit some applications, including visualization of cracks and vertical root fractures.6,7 Therefore, clinicians should ensure the benefits of the CBCT outweigh the risks before taking the scan and that another imaging modality would not provide equal diagnostic information.
Stationary Intraoral Tomosynthesis (sIOT) is a newly introduced imaging technology intended to change how dentists acquire and interpret radiographic images (Fig. 1). SIOT is designed to improve intraoral imaging without the limitations of CBCT. Developed by Surround Medical Systems, the Portray® sIOT uses a carbon nanotube array to capture multiple images with a single exposure from multiple sources within the X-ray tube (Fig. 2 – black arrow). In essence, there are seven X-ray sources within the tube, and a single shot generates a series of images that are then manipulated by a computer algorithm, like CBCT, to generate an image stack that allows visualization of the field through or around the teeth, but there is no axial view with sIOT. Each reconstruction stack contains roughly 45 buccal to lingual slices, with each slice representing 0.5 mm of object thickness. Each reconstruction also allows rotation of a 2D image plus or minus 6 degrees to open interproximal contacts, thus facilitating the diagnosis of interproximal caries and eliminating the need for retakes when contacts are overlapped. The Portray system is also able to take a standard 2D image should the need arise; however, with the introduction of sIOT, the need for standard 2D images will likely become obsolete.
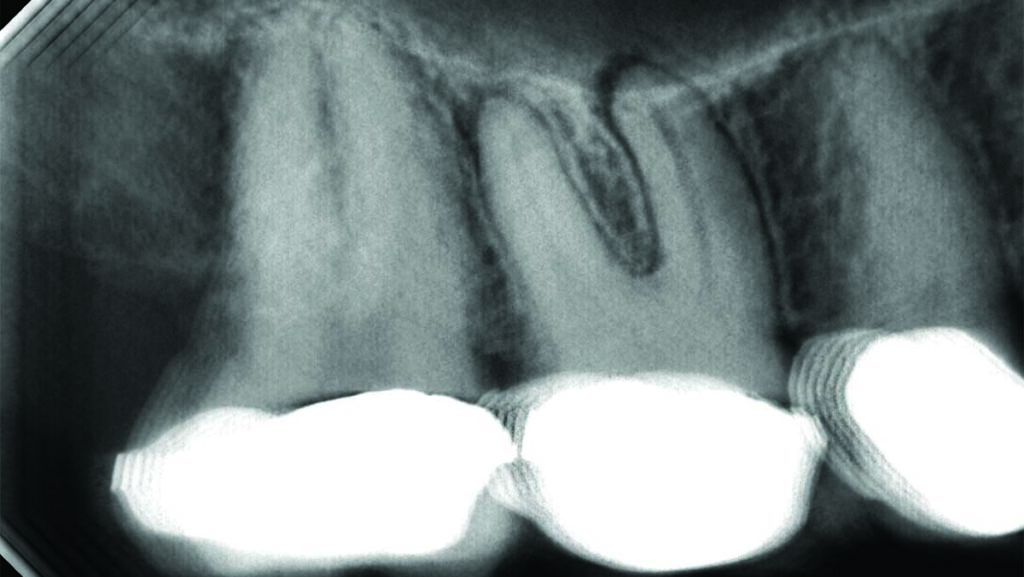
Fig. 1

Fig. 2
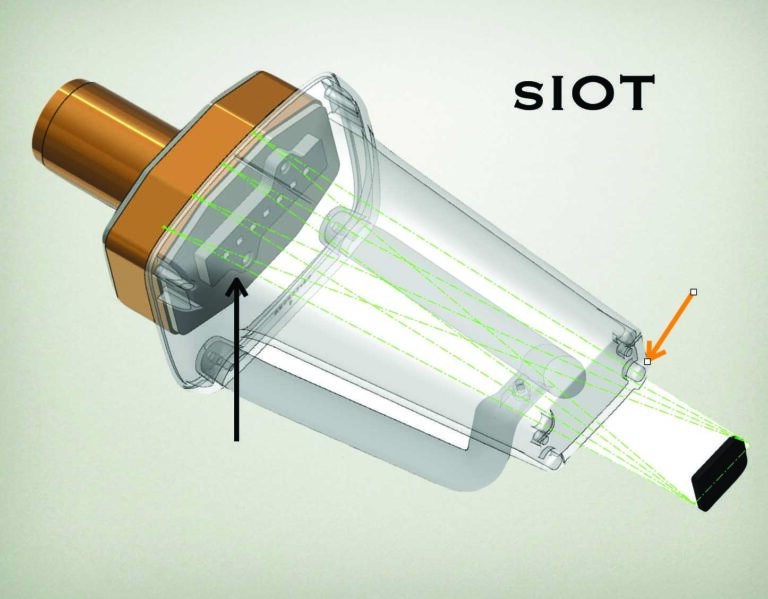
The image sensor is coupled to the tube head with four magnets (Fig. 2 – orange arrow). This standardizes the X-ray source to sensor distance, allowing the computer to determine buccal-lingual distances. As a result, it is possible to scroll through the image stack to visualize palatal roots of maxillary molars without superimposition of the sinus or buccal roots – resulting in better lesion detection at the root apices when considering endodontic treatment (Fig. 3).
Fig. 3A

Fig. 3B
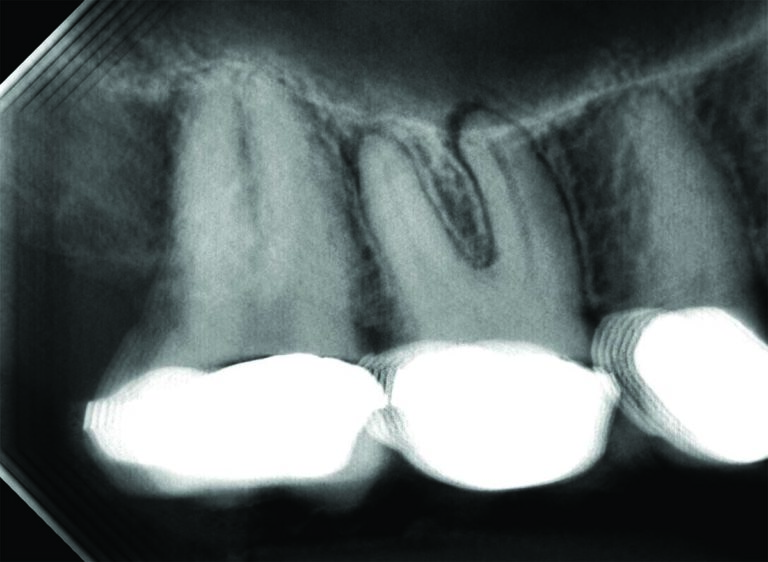
Image acquisition is virtually identical to periapical imaging because it is a standard size 2 digital sensor. Film placement is the same as for traditional two-dimensional periapical images. As a result, no special training is necessary to acquire the image. However, because the tube is indirectly attached to the sensor via magnets, the need for retakes is eliminated if the film placement is accurate. There is no motion blur to the images because there is no movement of the x-ray source, as would be the case with CBCT, and there is no scattering of the X-ray beam due to movement around metal restorations or implants. The image is immediately available, and the resolution is identical to standard two-dimensional digital imaging. The viewing software is intuitive, and no special training is required for the dentist or staff to review the image stack. As a result, the clinical workflow is identical to that of 2D imaging.
One disadvantage of sIOT compared to periapical imaging is the initial cost of changing systems. However, with increased caries detection, periapical lesion identification and periodontal diagnosis, the return on investment is significant, and cost should not be considered a barrier for clinicians who want to practice at the absolute highest level. The amount of information on an sIOT compares favourably to periapical imaging, but more information is available on a CBCT, especially when considering the axial view that is available on a CBCT. However, this is not without significant concerns for many clinicians. Even with a small field CBCT, many incidental findings are likely to be present on a CBCT. Clinicians are responsible for all information visible on the CBCT, and any subtle pathology that is not identified exposes the dentist to significant liability. As a result, a complete and thorough reading of the entire volume requires a disruption in workflow.
The radiation dosage of sIOT is comparable to intraoral imaging and considerably less than a CBCT. A standard digital periapical image has a radiation dosage near 9.5 uSV, roughly one day of background radiation. A single sIOT image has approximately 12 uSV or 1.5 days of background radiation. A full mouth series of digital images would be approximately 85 uSV the equivalent of 10 days of background radiation. CBCT would have a range of dosages from a small field CBCT with 84 uSV to a large field of view with a mean dosage of 212 uSV.
The technology is so new at this point that clinical studies have not yet verified how much better sIOT will prove to be compared to conventional periapical imaging. However, the ability to rotate the sIOT image should prove to be far superior for interproximal and recurrent caries detection compared to standard periapical imaging because of the opportunity for improved visualization of the contacts. Periapical lesion detection should also be much improved compared to conventional imaging because of the ability to slice through the image stack in the buccal-lingual direction. Additionally, the ability to slice through the image stacks in a buccal-lingual direction allows for better evaluation of crestal bone height in the detection of periodontal disease. Currently, there is no imaging technology that readily shows vertical root fractures and cracks. The reduction in metal artifacts and the ability to slice through and around teeth with sIOT may result in increased crack detection as well as earlier identification of resorptive defects.
Currently, most clinicians don’t know what sIOT is or what the potential of sIOT might be. However, sIOT is being taught at a handful of dental schools in the United States. This should result in clinically relevant studies confirming its value and benefits compared to other imaging modalities. Software and hardware upgrades are likely to yield even better and quicker image acquisition and quality. Lastly, the image analysis will likely be coupled with artificial intelligence tools, allowing practitioners to evaluate the image stacks more quickly with increased diagnostic accuracy. Although still unproven due to the lack of peer-reviewed clinical studies, early anecdotal evidence suggests sIOT will prove to be a superior imaging modality compared to conventional imaging when it comes to interproximal caries detection, periodontal and endodontic diagnosis and the identification of cracks and vertical root fractures. 
Oral Health welcomes this original article.
Disclaimer: The author is a consultant and stockholder in Surround Medical systems.
References
- Goldman M, Pearson AH, Darzenta N. Endodontic success–who’s reading the radiograph? Oral Surg Oral Med Oral Pathol. 1972 Mar;33(3):432-7.
- Bender IB, Seltzer S: Roentgenographic and direct observation of experimental lesions in bone. Part I. J Am Dent Assoc 1961; 62:152.
- Bender IB. Factors influencing the radiographic appearance of bony lesions. J Endod 1982 Apr;8(4):161-70.
- Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: II. 1961. J Endod. 2003 Nov;29(11):707-12.
- AAE and AAOMR Joint Position Statement: Use of cone beam computed tomography in endodontics 2015 update. J Endod 41:1393, 2015.
- Ee J, Fayad MI, Johnson BR. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod. 2014 Jul;40(7):910-6.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, Hashir MMJ, Arockiam S, Uma Maheswari TN, Natanasabapathy V. Diagnosis of Vertical Root Fractures by Cone-beam Computed Tomography in Root-filled Teeth with Confirmation by Direct Visualization: A Systematic Review and Meta-Analysis. J Endod. 2021 Aug;47(8):1198-1214.
About the Author

Dr. David Landwehr earned his DDS at the University of Minnesota. He also received an MS degree and certificate in oral and maxillofacial pathology from Ohio State University and specialty training in endodontics from the University of Michigan. He was the Chief of Endodontics for the Meriter Hospital general practice residency for more than ten years. Dr. Landwehr has been a private practice clinician for more than twenty years. He authored the chapter titled “Lesions That Mimic Endodontic Pathosis” for the most recent edition of Cohen’s Pathways of the Pulp. His teaching focuses on techniques used daily in his clinical practice that are efficient, predictable, and evidence based.











