
Abstract
Purpose: Fracture of dental implants, though uncommon, presents significant clinical consequences. The case reports presented explore the fracture of four dental implants in three patients. All were of the Astra Osseospeed® design with internal conical connections. All fractured at the level of the prosthetic connection, providing insight on potential contributing factors.
Methods: Three patients all received regular diameter, internal conical connection implants to replace missing bicuspid or molar teeth. One received a single implant for a mandibular molar, one received two implants to support a posterior mandibular 3-unit prosthesis, and the final patient received two single implants, one to replace a maxillary bicuspid and the other for a mandibular molar.
Results: Patient one received an Astra EV implant in 2019 and presented repeated episodes of screw bending and loosening, progressive bone loss over a two-year period, and fracture and implant removal. The second patient received two Astra EV implants in 2018 to support a fixed 3-unit prosthesis. Gradual crestal bone loss and recurrent prosthetic loosening resulted in the eventual fracture of both implants. The third patient received two separate posterior Astra implants in 2017, and despite initial stability, complications arose, including peri-implantitis and fractures.
Conclusions: This case series highlights the importance of recognizing fracture risk at the level of the prosthetic platform of internal, conical connection implants following or in association with which may be associated with crestal bone loss.
Keywords (MeSH): Bone loss; Case reports; Dental implant; Implant fracture.
Given the widespread use of threaded, endosseous dental implants to replace lost and hopeless teeth, it is surprising that fracture of these small medical devices is not a more common finding. One early study of 157 Straumann implants reported 1.9% fracture out to 40 months in function.1 Another assessment of 18,700 implants of various designs showed a 1-year fracture rate of 1.46% of which 94.6% happened at premolar and molar sites.2 More commonly, abutment screws or prosthesis gold screws fractured first, and this may be an early warning of future implant fracture risk.3 Habits like bruxism and the use of cantilevers can increase the risk of implant fracture.4 This report describes a series of three patients who all had at least one internal conical connection implant that fractured at the level of the prosthetic connection. In total, four of the five implants placed fractured and had to be removed.
Materials and methods
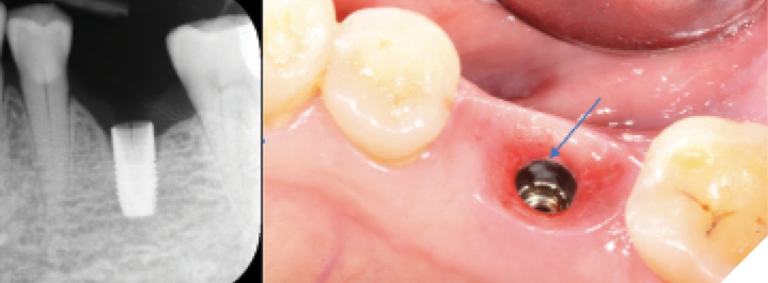
All patients had provided written consent, allowing authorized individuals to have access to their health information and dental records for teaching, publication and research purposes. Patient one was a 75-year-old male who had a regular diameter, 9mm-long Astra Tech EV Osseospeed® implant (Dentsply/Sirona) placed in August 2019 with a primary torquing value of 40 Ncm and a healing abutment placed immediately (Fig. 1A). The implant was restored in December of that year with the crown torqued down to 25 Ncm and placed in implant-protected occlusion (Fig. 1B). The following two years were uneventful until a recall exam by the patient’s dental student revealed minor mobility of the implant crown and some mesial bone loss in July 2021 (Fig. 1C). The crown and its retaining screw were removed, inspected by a periodontal resident and re-inserted with torque 25Ncm. In August of 2021, the patient returned again with mobility of the implant crown. Upon removal and inspection, the implant screw was bent and was replaced and torqued again to 25 Ncm. In January of 2022, the patient returned with mobility once more. Upon inspection, the implant screw appeared bent and, therefore again, was replaced and retorqued. When in September of 2022, the patient returned for routine follow-up, no mobility or heavy contact points or interferences in maximum intercuspation or excursive movements were found. However, slight pain to palpation was recorded buccally without evidence of erythema, edema, fluctuance or signs of acute infection but some bone loss distally (Fig. 1D). The patient returned in October of that year complaining of mobility and low-grade pain of 2 months’ duration. Intraoral exam revealed normal probing depths but extreme sensitivity to percussion. Once the implant crown was removed, a fracture line was observed in the buccal wall of the internal implant platform (Figs. 1E & 1F). Final treatment involved implant removal, socket preservation grafting and eventual placement of a new implant.
Fig. 1A

Fig. 1B

Fig. 1C

Fig. 1D

Fig. 1EF
Patient two was a 64-year-old female who had received two regular diameter, 9mm-long Astra EV implants in early 2017. Both implants were placed epi-crestally and were intended to support a 3-unit fixed prosthesis (Fig. 2A). Primary stability of 35Ncm was achieved, and healing abutments placed with subsequent uneventful healing. Five months later, a porcelain-fused-to-metal, 3-unit screw-retained fixed prosthesis was successfully installed with the manufacturer-recommended torque values of 25 Ncm. Both implant-protected occlusion and satisfactory interproximal contacts were ascertained. The patient then was lost to follow-up for 14 months, during which no reported maintenance procedures were performed. At this 14-month post-restoration recall exam, no significant issues were identified. However, it was observed that approximately 2mm of crestal bone loss had occurred at the mesial aspect of the distal implant (Fig. 2B). The patient returned as requested to the referring dentist with the suggestion of regular 6-month maintenance care. Two years later, she presented with complaints of prosthesis looseness during the previous ten months. Tightening of the implant screws resolved the issue, and she resumed regular 6-month maintenance visits with her referring dentist. Then, in January 2023, she returned with progressive bone loss at both implants (Fig. 2C). Clinical examination did not reveal signs of inflammation or infection, and probing depths remained <3mm. Later re-examination of this radiograph suggested that a crack was already an issue at the distal aspect of the mesial implant. To address the ongoing bone loss, a 3-month regimen of scaling and root planing with localized Arrestin® was recommended, but the Arrestin® was declined by the patient for financial reasons. Then, in May 2023, the prosthesis loosened and both radiographic and clinical examinations revealed fractures of both implants (Figs. 2D & E).
Fig. 2A
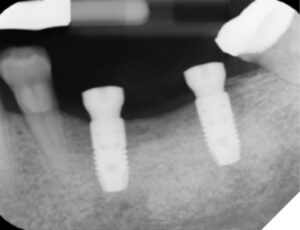
Fig. 2B

Fig. 2C

Fig. 2D

Fig. 2E

They were explanted with socket grafting procedures done for later re-implantation.
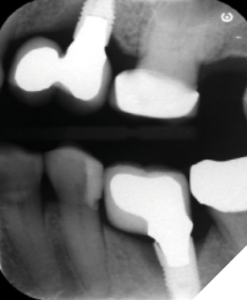
The third patient, a woman with Type II diabetes, was also treated in 2017, at which time two regular diameter Astra implants were used. The first was 6mm in length and placed in the maxillary left second bicuspid site (Fig. 3A), and the other was 9 mm long and placed at the mandibular left first molar site (Fig. 3B). Both had excellent primary stability (35 Ncm) with healing abutments placed. The maxillary implant was placed distally in the edentulous area with the plan of supporting a mesial cantilever pontic (Fig. 3C). The molar implant also was positioned distally in the edentulous area and, as a result, later required a crown that was over-contoured mesially and resembled a cantilever (Fig. 3D). In late March 2018, the patient presented with non-specific pain in the mandibular left region. The gingiva surrounding both implant crowns appeared inflamed but tested negative with percussion and displayed normal probing depths. The patient’s oral hygiene and periodontal condition had deteriorated since her last visit. Re-contouring of the crown was suggested but never done. She had recently fainted, and as a result, her MD had ceased all anti-hypertensive and oral hypoglycemic medications for a month with the aim of re-calibrating her medicinal regime. After this re-calibration, she was coached further for improved hygiene but was then lost to follow-up during the pandemic and not seen for four years (March 2022), at which time she presented with loosening of both prostheses. New radiographs (Figs. 3E and 3F) of both implants revealed greater bone loss compared to 2018, yet there were no signs of bleeding on probing or purulence. The crowns were re-torqued to 35 Ncm; but then, in December 2022 she returned as her dentist had detected a mesial fracture of the molar implant. (Fig. 3G) At that appointment, both implants displayed severe bleeding on probing and suppuration with more than 75% bone loss mesially at the maxillary 6mm-long implant and 50% bone loss mesial to the molar implant. The patient reported poor control of her diabetes (HbA1C of 8%) and had not been following the recommended homecare routines. Diagnosis of peri-implantitis at both implants was noted, and as well a fracture of the molar implant had occurred. Both were planned for removal.
Fig. 3AB
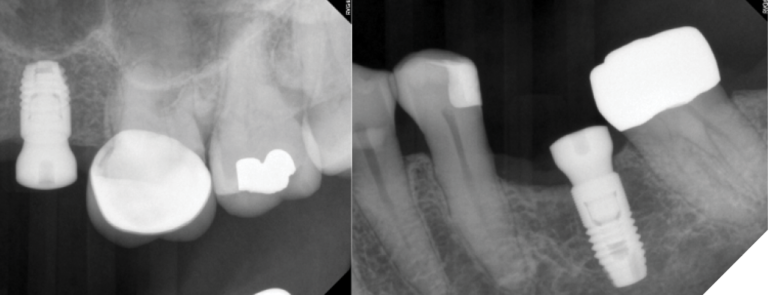
Fig. 3CD
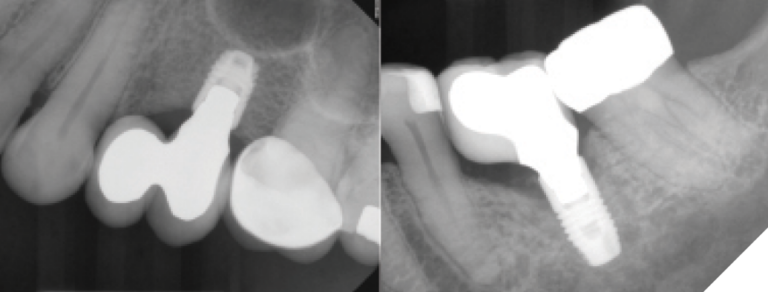
Fig. 3E
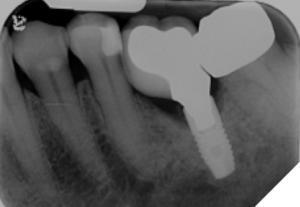
Fig. 3FG
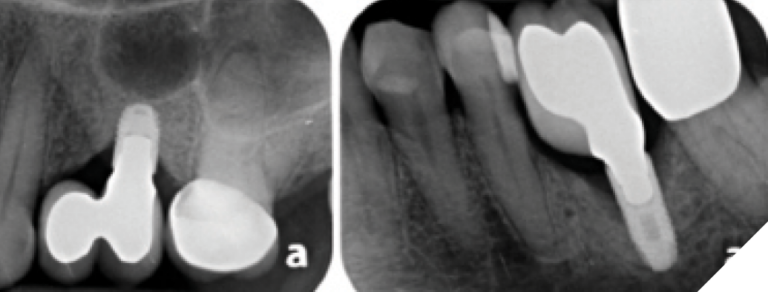
Fig. 3H
Discussion
A common thread with all four fractured implants reported here was that they all experienced one or more episodes of earlier crown loosening, a common precursor and warning sign of potential implant fracture.5 They had all been used to replace molar or bicuspid teeth. As well, crestal bone loss appeared to have preceded the fractures. Peri-implant crestal bone loss has been associated with multiple factors6 including implant design, depth of placement (epi- or sub-crestal), prosthesis emergence profile and passivity of fit, whether or not platform switching was used, micromotion, microbial deposits at the implant-abutment connection of bone level implant designs, gingival phenotype, occlusal overload, access for daily homecare and professional maintenance, smoking cigarettes and medical conditions such as poorly controlled diabetes type 2.
The Astra implant design has coronal micro-threads to help minimize crestal bone loss7 and an internal conical prosthetic connection with platform switching. As with other internal conical connection bone-level implants, it has been documented that sub-crestal implant placement of 1 to 2mm can all but eliminate crestal bone loss.8 In the cases presented here, the implants were not submerged sub-crestal. An internal conical connection also adds stability at the implant–abutment interface, but results in stress concentration under oblique loading near this interface.9 This is in contrast to early endosseous bone level implants like that of Brånemark, which had external hex prosthetic connections with risk of micromotion, was generally placed epi-crestal, and frequently showed stress concentration at the most coronal two to three threads with peri-implant crestal bone loss of ≥2mm. However, internal conical connections can make metal fatigue behavior inferior to that of external hex connections10 because of reduced side wall thickness of the implant body at the level of the prosthetic connection,11, 12 especially with standard diameter implants as used here.8 Cho et al. provided 3D FEA findings on stress distribution of internal conical connection implants of diameters 3.5mm to 5mm.13 As side wall thickness of the implant body at the level of the prosthetic connection increased with increasing implant diameter (0.325mm to 0.825mm wall thickness with implant diameters 4 and 5mm respectively), stress at the implant-abutment interface decreased. There is, of course, the possibility that implant surface micro-cracks in our three patients could have appeared first without detection and subsequently led to crestal bone loss and more recognizable crack formations,14 but this was not possible to determine. One study of 100 implants removed following biological complications found that 60% had micro-cracks when carefully scanned.15
In a report by Chrcanovic et al.4 of 10,099 implants from a variety of manufacturers, the overall fracture rate was 0.44% between years two and eight. Their Astra Osseospeed® fracture rate was 1.43%, and as with our three patients, fractures happened in the thin wall at the level of the prosthesis connection. Bruxism increased the overall failure by an incredible 1,819.5%, while every 1 mm increase in implant diameter led to a decrease in fracture risk of 96.9%.4 Hamilton et al.16 recently published a paper documenting two fractures similar to those reported here. The first had been used to replace a maxillary second bicuspid tooth and had a history of frequent prosthetic screw loosening, suggesting occlusal overload, while the second was that of a maxillary central incisor with increasing crestal bone loss. Use of wider diameter implants with thicker wall thickness might have reduced fracture risk.4
As mentioned already, Linkevicious et al.8 have shown that placing implants with internal conical connections like the Astra design sub-crestal by at least 1.5mm significantly reduces crestal bone loss. None of the implants reported here had been placed sub-crestal, and this may have been a factor with the observed bone loss, although other contributing factors such as over-contoured crowns, cantilever effects, suboptimal homecare, bruxism and diabetes also may have been involved. Having lost bony support, the thin walls of the coronal connection may then have predisposed to fracture during off-axis loading. At least one of the three patients reported here had a long-standing history of bruxism, which others have reported to be present in at least 80% of patients diagnosed with implant fracture.17 
Oral Health welcomes this original article.
Conflict of Interest Statement: The authors declare no conflicts of interest or financial support in the presentation of this manuscript.
Author Contribution Statement: All three authors contributed to the realization of this manuscript and approved it before submission. RDV and DWW reviewed the patient records; DAD was responsible for the manuscript’s conception, interpretation and final preparation.
References
- Levine RA, Clem DS, 3rd, Wilson TG, Jr., et al. Multicenter retrospective analysis of the ITI implant system used for single-tooth replacements: results of loading for 2 or more years. Int J Oral Maxillofac Implants 1999;14:516-520.
- Tabrizi R, Behnia H, Taherian S, et al. What are the incidence and factors associated with implant fracture? J Oral Maxillofac Surg 2017;75:1866-1872.
- Gealh WC, Mazzo V, Barbi F, et al. Osseointegrated implant fracture: causes and treatment. J Oral Implantol 2011;37:499-503.
- Chrcanovic BR, Kisch J, Albrektsson T, et al. Factors influencing the fracture of dental implants. Clin Implant Dent Relat Res 2018;20:58-67.
- Alsubaiy EF. Abutment screw loosening in implants: A literature review. J Family Med Prim Care 2020;9:5490-5494.
- Linkevicius T. Zero Bone Loss Concepts: A Path to Crestal Bone Stability Quintesence 2019.
- Al-Thobity AM, Kutkut A, Almas K. Microthreaded implants and crestal bone loss: A systematic review. J Oral Implantol 2017;43:157-166.
- Linkevicius T, Puisys A, Linkevicius R, et al. The influence of submerged healing abutment or subcrestal implant placement on soft tissue thickness and crestal bone stability. A 2-year randomized clinical trial. Clin Implant Dent Relat Res 2020;22:497-506.
- Lee H, Park S, Noh G. Biomechanical analysis of 4 types of short dental implants in a resorbed mandible. J Prosthet Dent 2019;121:659-670.
- Gil FJ, Herrero-Climent M, Lazaro P, et al. Implant-abutment connections: influence of the design on the microgap and their fatigue and fracture behavior of dental implants. J Mater Sci Mater Med 2014;25:1825-1830.
- Bing L, Mito T, Yoda N, et al. Effect of peri-implant bone resorption on mechanical stress in the implant body: In vivo measured load-based finite element analysis. J Oral Rehabil 2020;47:1566-1573.
- Hanif A, Qureshi S, Sheikh Z, et al. Complications in implant dentistry. European journal of dentistry 2017;11:135-140.
- Cho SY, Huh YH, Park CJ, et al. Three-dimensional finite element analysis of the stress distribution at the internal implant-abutment connection. Int J Periodontics Restorative Dent 2016;36:e49-58.
- Shemtov-Yona K, Rittel D. An overview of the mechanical integrity of dental implants. BioMed research international 2015;2015:547384.
- Shemtov-Yona K, Rittel D. On the mechanical integrity of retrieved dental implants. Journal of the mechanical behavior of biomedical materials 2015;49:290-299.
- Hamilton A, Putra A, Nakapaksin P, et al. Implant prosthodontic design as a predisposing or precipitating factor for peri-implant disease: A review. Clin Implant Dent Relat Res 2023.
- Stoichkov B, Kirov D. Analysis of the causes of dental implant fracture: A retrospective clinical study. Quintessence Int 2018;49:279-286.
About the Authors

Rickson D. Valtellini, DDS, Graduate Periodontics, Faculty of Dentistry, University of Toronto, Toronto, ON M5G 1G6.

Dempsey W. Wood, DMD, Graduate Periodontics, Faculty of Dentistry, University of Toronto, Toronto, ON M5G 1G6.

Douglas A. Deporter, DDS, Dipl Perio, PhD, Discipline of Periodontology, Faculty of Dentistry, University of Toronto, Toronto, ON M5G 1G6. E-mail: douglas.deporter@dentistry.utoronto.ca. https://orcid.org/0000-0003-2531-8747; Tel: 416-864-8208; Fax: 416-979-4755











