
Abstract
A full arch, implant-supported fixed prosthesis can be successfully used to rehabilitate an edentulous arch. Despite high success rates, biological complications due to peri-implant mucositis and peri-implantitis can threaten the survival of one or more of the implants, and may result in prosthesis failure with devastating consequences for the patient. In order to minimize risk of failure, maintenance of the prosthesis and implants should be performed by the patient and a dental professional on a regular basis. This paper reviews several important considerations for maintenance of full arch screw-retained, fixed implant-supported prostheses.
An implant-supported fixed prosthesis is an effective method of rehabilitating an edentulous arch having been documented to exhibit both high short-term and long-term survival rates.1 However, both mechanical and biological complications may lead to treatment failire.2 Biological complications involve adverse inflammatory reactions within the soft and hard tissues surrounding the implant, and include peri-implant mucositis and peri-implantitis.2 Peri-implant mucositis refers to inflammation of the soft tissues only, and generally can be reversed with proper intervention.3 If left untreated however, peri-implant mucositis may progress to peri-implantitis with resultant resorption of peri-implant crestal bone.3 According to one study, peri-implant mucositis occurs at 19 to 65% of implants, while peri-implantitis threatening implant survival occurs at 1 to 47% of all implants.4 Francetti et al. reported that peri-implantitis occurred in 14% of full arch implant-supported prosthesis cases by 10 years in function.5 In order to prevent these biological occurrences, fastidious daily patient homecare and periodic professional maintenance are of utmost importance.
Prosthesis designs including favorable emergence profiles of abutment units and easily accessible inter-implant pontic sections that allow access for meticulous patient homecare are essential. Following treatment completion, regular professional maintenance care should be scheduled initially at least every 6 months or more frequently for patients who have difficulty with adequate daily homecare or with patients who have experienced significant changes in health status such as onset of diabetes.6-8 A checklist of items needing attention at each recall is provided in Table I.
Table I: Recall Data Checklist
| A. General Health | Have there been any changes in systemic health or medications taken since the last assessment? |
| B. Patient Feedback/Concerns | Are there reported episodes of soft tissue bleeding/swelling/ discomfort since the last visit? |
| C. Assessment of Function | Has the patient experienced issues such as difficulty in chewing, food impaction or discomfort during function? Are there signs of excessive occlusal wear or damage to the prosthesis and/or evidence of cheek or tongue biting? |
| D. Oral Hygiene | Are there visible levels of dental plaque/calculus accumulation around the implant abutments or prosthesis? Does daily homecare elicit bleeding or discomfort? |
| E. Peri-implant Soft Tissue Assessment | Are there signs of mucositis, gingival swelling or bleeding upon peri-implant probing? Are there any significant changes in peri-implant pocket depth? Are there any signs of purulence with or without probing? |
| F. Radiographic Assessment | Are there signs of crestal bone loss in carefully taken radiographs? Has earlier bone loss progressed? |
A maintenance appointment for a screw-retained, full arch implant-supported prosthesis should include the following components. Firstly, the patient should be questioned about any concerns with comfort and function of the prosthesis. The occlusion should then be assessed using articulating paper to ensure uniformly distributed contacts. Since the majority of full arch, implant-supported prostheses are difficult for patients to clean, the prosthesis should be removed periodically. This requires removal of the restorative material filling the screw access holes to allow loosening the prosthetic screws. Care should be taken to record which implant each screw belongs to and all screws examined for signs of bending and wear. If need be, damaged screws should be replaced with new ones. Once the prosthesis is removed, the clinician will be able to assess the true efficiency of patient hygiene and more accurately assess any peri-implant pocketing and inflammation.
The intaglio surface of the prosthesis should be examined for plaque and calculus accumulation and any cracks or signs of wear. If the intaglio surface contains areas which are food traps, it may be appropriate to consider refining it with a drill or utilizing a material to fill in any concavities (Fig. 1C). If the retaining screws do not require replacement, the retrieved screws should be cleaned with gauze and 70% ethanol followed by soaking in chlorhexidine (0.12% solution or stronger). All implant abutments should be checked for movement and torqued if need be. After a 30-second oral rinse with chlorhexidine, all abutments should be meticulously cleaned. Cleaning protocols can include airflow, ultrasonic or piezo scaling devices using plastic-tips and/or titanium or plastic-tipped scalers. Meanwhile, the prosthesis should be meticulously cleaned and disinfected using hand and ultrasonic scalers, acrylic-cleaning solutions in an ultra-sonic bath, steam disinfection, and/or scrubbing with 70% ethanol or chlorhexidine. All prosthetic screw chambers (“chimneys”) should be scrubbed with micro-brushes and ethanol.
Table II: Full Arch Dental Prosthesis Maintenance Checklist
| Complete Recall Data Checklist |
| Removal of Prosthesis |
| Peri-implant Soft Tissue Assessment |
| Prosthetic assessment (including evaluating intaglio surface) |
| Check and clean abutments |
| Clean prosthesis |
| Check and clean prosthetic screws |
| Re-insert prosthesis |
| Evaluation occlusion |
| Seal prosthetic screw access holes |
Following re-insertion of the cleaned prosthesis, all retention screws should be tightened using torque forces in keeping with the recommendations of the appropriate implant manufacturer and implant platform design. The screw heads should then be protected with Teflon tape and re-sealed with a temporary restorative material of choice. The use of composite resin requires drilling out at every maintenance appointment which is time-consuming and can result in damage to the prosthesis. An alternative option is the use of a temporary material such as Clip Flow (Voco), which can be removed with a scaler and does not require the use of a drill. Finally, the occlusion should be re-checked and the patient’s feedback on the occlusion noted. Lastly oral hygiene and home care instructions should be reviewed.
Future maintenance appointments should be determined based on the patient’s level of home care and presence of food, plaque and calculus under the prosthesis. Five sample cases follow.
Case 1: A 75-year old male presented with full arch, implant-supported mandibular prosthesis. Upon prosthesis removal, evidence of poor oral hygiene was noted with abundant soft deposits on its intaglio surface associated with surface concavities (Fig. 1B) which were corrected by filling them with acrylic, and polishing the area with a lathe and polishing paste. (Fig. 1C)
Fig. 1A

Fig. 1B

Fig. 1C

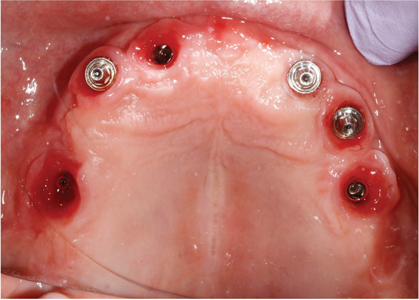
Case 2: A 60-year-old female presented with full arch, fixed prostheses in both maxilla and mandible. The prostheses were designed with a combination and fixed and removable components and not cleansable due to the presence of flanges. They had not been removed for maintenance during the previous 7 years. Upon removal of the fixed prostheses, the intaglio surface was seen to have extensive deposits. (Fig. 2A) The implants also were covered with hard and soft deposits and as a result the peri-implant gingiva was inflamed and hyperplastic. (Fig. 2B) All implants in this case showed severe peri-implant bone loss and the entire case failed.
Fig. 2A

Fig. 2B

Case 3: A 75-year old male presented with a full arch, fixed prosthesis in the maxilla after 1 year in function. (Fig. 3A) Upon removal of the fixed prosthesis, the prosthesis, abutments and prosthetic screws were cleaned with chlorohexidine 0.12%.
Fig. 3A

Fig. 3B

Fig. 3C
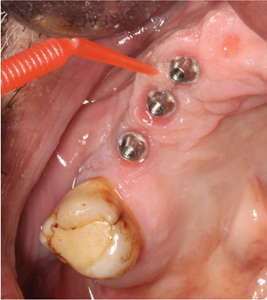
Fig. 3D

Fig. 3E

Case 4: A 68-year old patient presented for a 6-month maintenance of his full arch maxillary implant prosthesis. His prosthesis design allowed good access for daily homecare and upon its removal the peri-implant soft tissues appeared healthy while its intaglio surface also was reasonably clean.
Fig. 1

Fig. 2

Fig. 3

Fig. 4

Case 5: A 50-year old male with a fixed, full arch maxillary prosthesis presented for maintenance care. The prosthesis was supported by two different implant systems with three implants having multi-unit abutment assemblies and the other three implants with internal connection abutments connecting directly to the prosthesis. (Fig. 5A) There was severe soft tissue inflammation around the implants that did not utilize multi-unit assemblies. (Fig. 5B)
Fig. 5A

Fig. 5B
Discussion
Full arch, screw-retained, implant-supported prostheses can be life-altering for individuals who have become fully edentulous. However, once inserted, they do need periodontic professional maintenance especially if access for daily homecare is impaired by the implant design or patient dexterity deficits. Without such professional care, peri-implant soft tissue health will most likely deteriorate with possible inflammation-driven peri-implant bone loss and even implant loss. How often these prostheses will need to be removed and decontaminated will depend on multiple factors including patient dexterity and compliance with recommended oral hygiene measures, patient age and risk of bacterial aspiration pneumonia and patient overall health and lifestyle. Practitioners providing full arch implant-supported restorations need to recognize their important role in maintaining long-term implant and patient health.
Oral Health welcomes this original article.
References
- Kwon T, Bain PA, Levin L. Systematic review of short- (5-10 years) and long-term (10 years or more) survival and success of full-arch fixed dental hybrid prostheses and supporting implants. J Dentistry 42: 1228-1241, 2014.
- Papaspyridakos P, Chen, C-J, Chuang, S-K, Weber, H-P, Gallucci, G. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int J Oral Maxillofac Impls 27: 102-110, 2012.
- Monje A, Aranda L, Diaz KT, Alarcón MA, Bagramian RA, Wang HL, et al. Impact of maintenance therapy for the prevention of peri-implant diseases. J Dent Res 95: 372-399, 2016.
- Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol 42 (Suppl 16): S158-S171, 2015.
- Francetti L, Cavalli N, Taschieri S, Corbella S. Ten years follow-up retrospective study on implant survival rates and prevalence of peri-implantitis in implant-supported full-arch rehabilitations. Clin Oral Impl Res 30: 250-258, 2019.
- Bidra A, Daubert D, Garcia L, Kosinsky T, et al. Clinical practice guidelines for recall and maintenance of patients with tooth-borne and implant-borne dental restorations. JADA 147: 67-74, 2016.
- Pirc M, Dragan IF. The Key Points of Maintenance Therapy for Dental Implants: A Literature Review. Compend Cont Educ Dent 38 (4): April 2017.
- Todescan S, Lavigne S, Kelekis-Cholakis A. Guidance for the maintenance care of dental implants: Clinical review. J Canadian Dent Assoc 78: c107, 2012.
- Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, et al. Primary prevention of peri-implantitis: Managing peri-implant mucositis. J Clin Periodontol 42 (Suppl 16): S152–S157, 2015.
- Mombelli A. Maintenance therapy for teeth and implants. Periodontology 2000 79: 190-199, 2019.
About the Authors

Joanne Lin is a dental student at the University of Toronto (2T5). She completed her undergraduate degree at the University of Guelph studying Neuroscience.

Dina Zahedi completed her DDS and specialty certificate in Periodontology from New York University (2019). She is a part-time clinical instructor at University of Toronto.

Jaffer Kermalli completed his DDS and MSc specializing in Periodontology at the University of Toronto (2011). He is a part-time instructor at the University of Toronto, an examiner for the Royal College of Dentists of Canada and the Past President of the Ontario Society of Periodontists.

Professor Douglas Deporter has been a Faculty member since 1976 and published extensively on dental implantology. His latest book “Immediate Molar Implants” was published by Quintessence in 2022.









