Distraction osteogenesis (DO) is a method of elongating a bone that was first described by the orthopedic surgeon Ilizarov. It was applied to long bones of the leg and significant lengthening was achieved.1 It was first described for the mandible in 1992 and was performed using an external device. The first case of maxillary DO using an internal device was reported in 1995. Since then, there have been many advances to the planning, surgical technique, and distractor development, which have resulted in smoother and more predictable results. The indications for maxillary DO include severe maxillary anteroposterior deficiencies (>10mm in non-cleft patients, >6mm in cleft patients), or as a treatment modality for actively growing patients with severe maxillary hypoplasia.2 The contraindications for maxillary DO include patient non-compliance or intolerance for the device, inability to follow up closely and monitor distraction progress, or a lack of bone stock or dentition for anchorage.
DO involves four separate phases. The first phase involves an osteotomy, in which the bone is surgically cut in a precise area and direction and a distractor applied. This is followed by the latency phase, where no movement or activation of the distractor is performed, and is typically 5-7 days. After this time period, the activation phase begins and the distractor is activated and turned daily to lengthen or “distract” the distal segment of the bone that has been cut. Once the desired position has been achieved, the final phase, known as the consolidation phase, is reached where the new bone is allowed to mature and fuse. The length of the consolidation phase varies for each case and patient, but traditionally has been thought to be 1 week long for each 1 mm of distraction.3
Maxillary DO can be done before or after skeletal maturity, but growth needs to be accounted for when planning the case and determining the final position of the maxilla. It’s also important to remember that the surgical endpoint of distraction cases may not be based on the desired final occlusion, as further surgery is often required in the form of conventional bimaxillary orthognathic surgery.
Although external distraction devices have been in practice a long time, technologic advances in internal distractors have made them far more common. The advantage of external devices include vector alteration, better control of three dimensional movements, and less risk for pressure necrosis. Disadvantages include decreased patient tolerance, psychological implications, cumbersome and bulky apparatuses, and risk of intracranial penetration. Internal distraction devices are less bulky, better tolerated by patients, and are easier to leave in for longer periods to allow for bony consolidation.4 Disadvantages include the fact that they are unidirectional, require adequate bone stock, and it can sometimes be difficult to plan the appropriate vectors for movement. However, virtual surgical planning and 3D-printed skull models have greatly helped with this limitation.
Case Presentation
This patient is a 19 M with a history of repaired left cleft lip and palate. His previous surgeries included primary closure of his cleft lip, palate, alveolar bone grafting, wisdom tooth removal, and multiple revision surgeries to his palate due to persistent fistulae. He was treated with conventional fixed orthodontics to level and align his maxillary and mandibular arches. He presents with significant maxillary hypoplasia, malar and paranasal flattening, decreased maxillary incisal show at rest and on smile, and a class III skeletal relationship and concave profile (Fig. 1).
Fig. 1A

Fig. 1B
His intra-oral photos show him to be in a permanent adult dentition with congenitally missing 12 and 22. He has -10mm of overjet, his maxillary midline is 4mm to the right, and a class III malocclusion is seen (Fig. 2).
Fig. 2

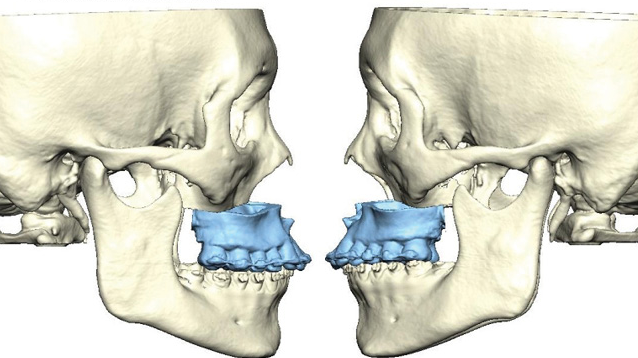
A CT scan of his maxillofacial complex and intra-oral scans of his dentition were obtained and the case was virtually planned using Individual Patient Solutions (IPS, KLS Martin, Jacksonville, USA) (Fig. 3). The KLS Martin Hyperdrive system was chosen due to it’s rigidity and adequate footplates for bony fixation. The anticipated amount of distraction based on the virtual plan required was 14mm, so an appropriate distraction arm was selected. Once the correct advancement and vector was chosen, a 3D-printed stereolithographic crystal skull model was obtained. Distractors were bent and adapted to the skull model according to the virtual plan, following the indented markings on the skull and being careful to avoid vital structures and dental roots (Fig. 4). Intra-oral photos show adaption of the distractors bilaterally, taking care to mark out the Lefort osteotomy line between the foot plates with a 701 bur (Fig. 5). The distractors were then removed, and a formal Lefort 1 osteotomy performed. An occlusal splint was temporarily wired to the maxilla to prevent fracture along the previous repaired alveolar cleft site during downfracture and mobilization (Fig. 6). This was removed after mobilization, and prior to re-fixation of the distraction devices and wound closure.
Fig. 3A
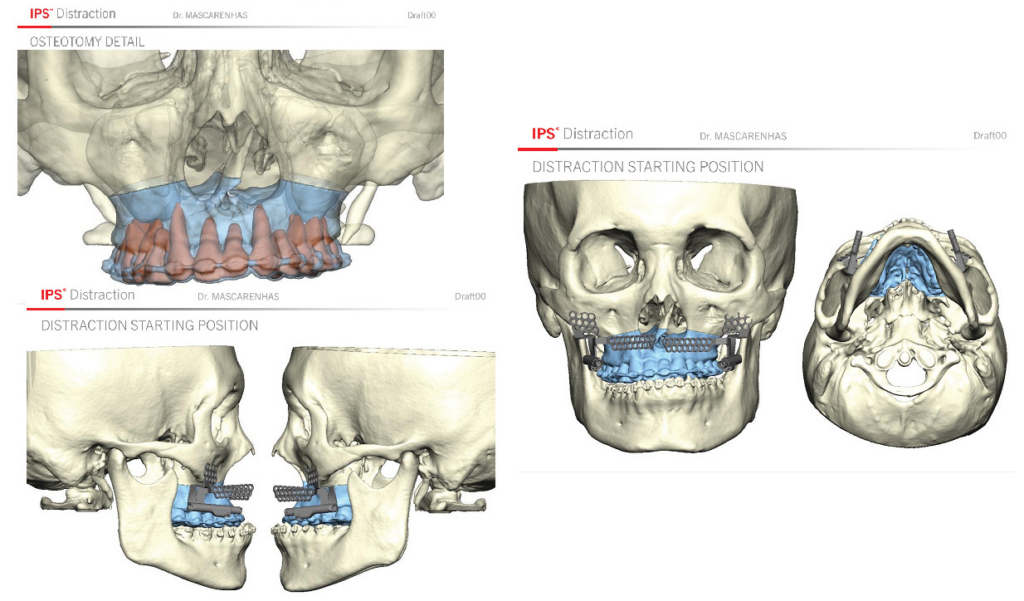
Fig. 3B
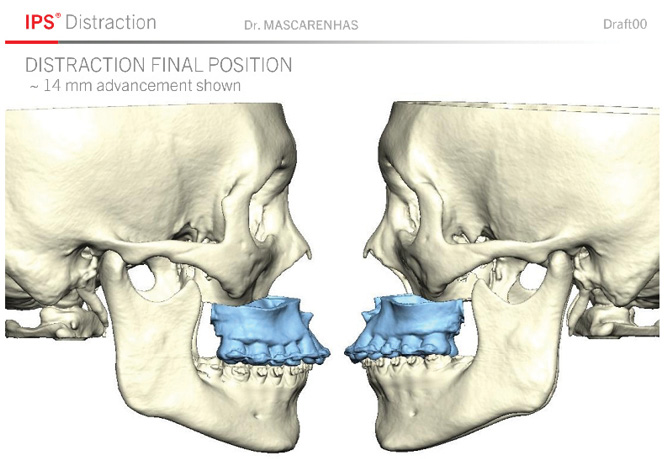
Fig. 4

Fig. 5A
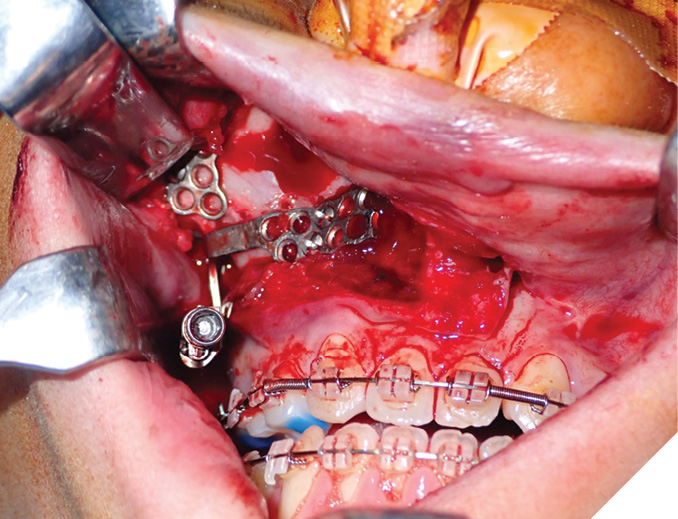
Fig. 5B
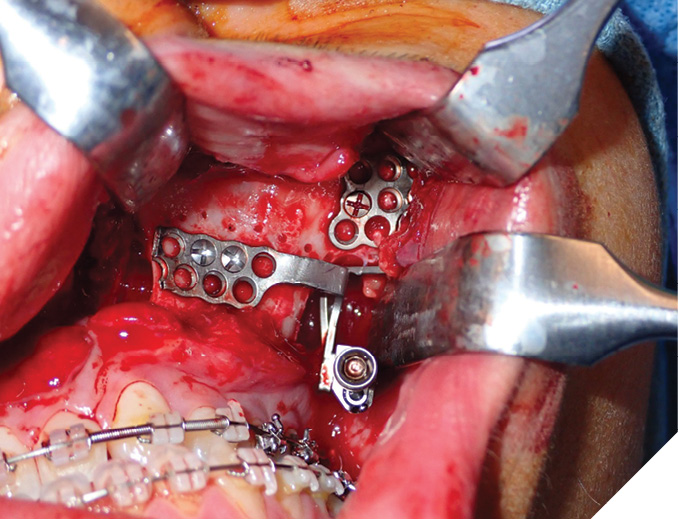
Fig. 6

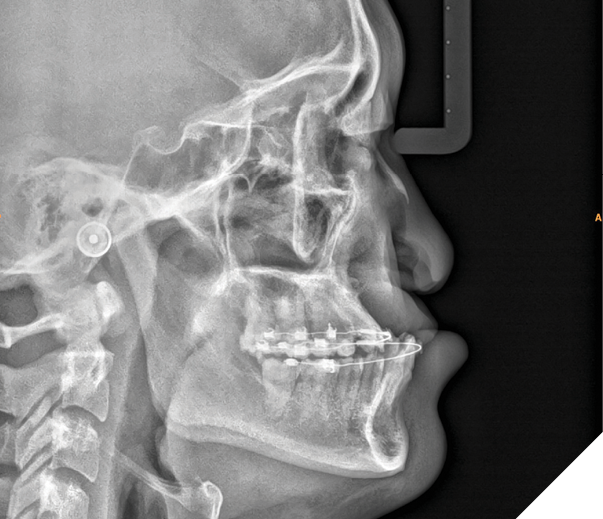
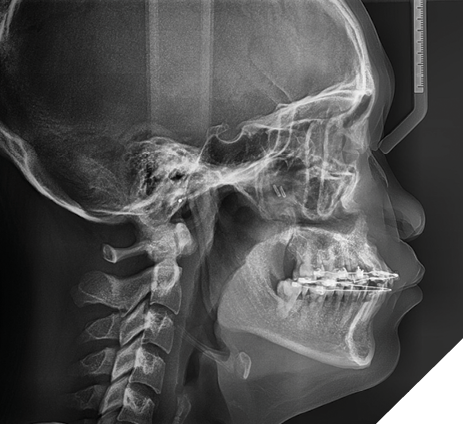
Post-operatively, we waited 7 days prior to initiating the distraction of the maxilla. This is known as the latency period. The maxilla was distracted 1mm bilaterally each day, divided into two sessions of 0.5mm each. The patient was instructed on how to turn the distractor and performed it at home twice daily. As shown from his post-operative intra-oral photographs, the maxilla can be seen to be advancing; however, the midline discrepancy to the right remained as we advanced the maxilla equally and symmetrically. Once edge to edge contact was achieved, we began asymmetrically distracting with 1mm BID on the right side and 0.5mm BID on the left. This led to an increase in the overjet, but also a correction of the midline (Fig. 7). His final lateral cephalometric x-ray shows the significant maxillary distraction achieved, and the resolution of his skeletal class III relationship (Fig. 8). Although the patient was originally planned for further orthognathic surgery, his final occlusion and skeletal relationship after maxillary distraction negated the need for any additional surgery. His distractors were removed after bony consolidation was complete, approximately 4 months post-operatively.
Fig. 7A

Fig. 7B

Fig. 7C

Fig. 7D

Fig. 7E

Fig. 8A

Fig. 8B
Although conventional orthognathic surgery is far more common than distraction osteogenesis, DO still has a vital role to play in specific circumstances, especially for those that suffer from cleft or craniofacial deformities. Incorporating modern virtual surgical planning and surgical techniques aids in making this once cumbersome procedure into a more routine, efficient process. 
Oral Health welcomes this original article.
About the Author

Dr. Wendall Mascarenhas is an Oral and Maxillofacial Surgeon who maintains a private practice in Brampton, ON. He is an Assistant Professor, University of Toronto, and an attending staff with the OMFS training program at Mt. Sinai Hospital. He is a supervisor of the Surgical Orthodontic clinic where he trains orthodontic and OMFS residents in orthognathic surgery.











