
The primary goal in endodontics is to save teeth and preserve long-term function. If a patient presents with a diseased or inflamed pulp, it must be removed from the root canal system in a manner that preserves tooth structure and restores occlusal function.1 Over the last ten years minimally invasive endodontics (MIE) is a concept that has been much discussed, researched and explored in the field of endodontics. MIE can be defined as preserving healthy coronal, cervical, and apical tooth structure during the access and shaping process of endodontic treatment.2 Smaller access cavity in conjunction with a smaller canal shape has been explored in order to preserve tooth structure and prevent tooth fracture. This is especially important in the senior community (over age 55) where there is a reduction of up to 50% in the tensile and fatigue strength in coronal dentin and an increase in incremental crack extension of up to 100 times.3,4 Traditional shaping can consist of a larger access, taper and apical size. MIE incorporates a reduced access cavity and smaller overall shape, but if not used in conjunction with an activated irrigation disinfection system may not be able to remove the infected pulp tissue adequately.5,6
Practicing MIE poses a question- “Can we create a smaller access, shape minimally while achieving maximal disinfection, and still obturate effectively creating a three dimensional hermetic seal?” For years the answer has been, “We don’t know.” So access and final canal shape continued to stay traditional so that the clinician could remove the infected pulp tissue, biofilm, microbes and have enough space for obturation materials.
The last ten years have brought an explosion of new irrigation devices (systems) that enhance disinfection compared to traditional standard needle irrigation (SNI).7-10 We now have commercially available products that “agitate and activate” the irrigation fluid in the canal system through several modalities. A few examples of these are sonic and ultrasonic activation, apical negative pressure with ultrasonic technology, acoustic streaming using different types of lasers, and multisonic sound wave acoustic streaming technology.
This article will discuss a minimally invasive shaping technique in conjunction with laser activated irrigation using an Erbium: Yttrium-aluminum-garnet (Er:YAG) laser.
In October of 2022 a new minimally shaping system came on the market. Designers Cliff Ruddle, John West, and Pierre Machtou took the ProTaper Gold (Dentsply Sirona) concepts and created a new file system that could appeal to the MIE community. The new file system called ProTaper Ultimate (Dentsply Sirona) (Fig. 1) reduced the file diameter size from 1.2 mm to 1 mm, reduced the number of files needed to finish the coronal and apical shape, and is the only file system to incorporate M-Wire, Blue-Wire and Gold-Wire metallurgy. According to the manufacturer, this new file system is more flexible and resistant to cyclic fatigue when compared to ProTaper Gold while creating smaller shapes and removing less pericervical dentin. ProTaper Ultimate consists of both a core set of files and auxiliary files that can be used to shape most anatomical canal size and variation.
Fig. 1

The core set of files in the ProTaper Ultimate system consists of the Slider, Shaper and Finishers. One of the more intriguing aspects of this new file system is a new type of nickel titanium shaping file called “The Slider.” The Slider is a file that incorporates a rather new concept in endodontics called “rotary negotiation.” The Slider has been designed to negotiate to working length without first exploring and securing the canal with hand files. It is designed to be the first file in (FFI) the canal. This is a complete paradigm shift in endodontics. In internal studies, Dentsply Sirona noted that 65% of the time the Slider advanced to working length without the use of a hand file. Read that sentence again and let it soak in. In the majority of cases the clinician can achieve negotiation to patency, an accurate working length, and an open glide path (3 major pillars of endodontics) all with one rotary file and often in just seconds. It requires a light touch and at times, multiple shaping passes. If the Slider does not advance to estimated working length after 4-5 engagement/disengagements, exit the canal, irrigate with sodium hypochlorite and then advance to pass #2. Usually the Slider will advance to working length and beyond in 1-3 passes. It is recommended to dip the tip of the Slider into file lubricant prior to canal entry and negotiation. If the Slider will not advance and it feels like it is hitting a “brick wall” then remove it from the canal and achieve negotiation by traditional means (#8 or #10 K hand file). In my clinical experience testing over 300 canals, the Slider advanced to working length 81% of the time. In the cases that I was unable to negotiate to working length there was typically an apical curve greater than 45 degrees.
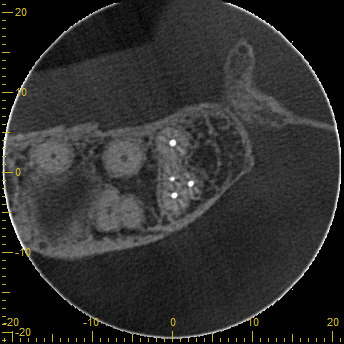
This new file system can potentially make minimally invasive shaping safer and more efficient. In cases where there is curvature and slimmer root structure, ProTaper Ultimate can be used to achieve minimal shape while preserving precious dentin and tooth structure. Combining this new minimally invasive shaping system with enhanced disinfection technology appears to amplify pulpal debridement (Figs. 2,3,4). This is the second component of MIE: pulpal and canal chemical debridement. As clinicians, we must combine mechanical debridement with chemical debridement to achieve ENHANCED disinfection.
Fig. 2A

Fig. 2B

Fig. 3A

Fig. 3B

Fig. 4A

Fig. 4B

Fig. 4C

Fig. 4D
In my office I have ultrasonic irrigation (EndoUltra-Vista), sonic activation (Smart Lite Pro Endoactivator- Dentsply Sirona) (Fig. 5), EndoVac negative apical pressure system (Kerr Endodontics), IVac negative apical pressure with ultrasonic energy (PacDent), the Pulp Sucker (Plan B Dental), multisonic sound wave technology (GentleWave- Sonendo) (Fig. 6), and laser activated disinfection (Lightwalker laser- Fotona) (Fig. 7). I have used all of these “enhanced” irrigation systems and find one of the easiest and most effective techniques is laser activated irrigation (LAI) using Shockwave Enhanced Emission Photoacoustic Streaming (SWEEPS) with the Lightwalker laser.
Fig. 5

Fig. 6

Fig. 7

SWEEPS is a technique that uses an Er:YAG laser that emits a dual pulse of photons from a laser tip into sodium hypochlorite, EDTA or distilled water that is present in the access cavity. In a study that compared hard tissue removal in mandibular molars after shaping using ultrasonic irrigation, Photon Induced Photoacoustic Streaming (PIPS) and Shockwave Enhanced Emission Photoacoustic Streaming (SWEEPS) it was found that SWEEPS was the most effective and removed 84.31% of accumulated debris verses 58.79% (PIPS) and 50.27% (UAI).11 The most convenient aspect of SWEEPS is you just replace standard needle irrigation (SNI) with a 30 second laser cycle between shaping passes. It’s easy to use, efficient and the laser tip DOES NOT extend down the canal. The shockwave created by the dual pulse pair advances from the pulp chamber down the canals. This technique is not only easy to master but is very efficient and intuitive to use. SWEEPS does not interfere with the endodontic treatment flow, and in my opinion, allows the clinician to practice MIE with a cleaner canal system in an efficient manner. The patient is happy with an efficient, effective treatment, your back and neck thank you and you are more productive in your practice.
Even better the time cost to use laser disinfection (SWEEPS) is ~7 minutes. In reality, it is even less, because the 2-4 SWEEPS cycles after access and during shaping just replaces SNI and only takes 15 seconds longer per cycle. In my practice, I often perform a 30 second SWEEPS cycle (20 mJ) after the access is complete and/or after coronal flare and then 2-4 SWEEPS cycles during shaping. Once shape is complete, the laser setting is “dialed back” to the Super Short Pulse (SSP) mode for the “final protocol.” SSP emits a single pulse and is effective at providing photon induced photo acoustic streaming (PIPS) once the minimal shape is complete. It has less power than the dual pulse pair that the SWEEPS setting emits. The final laser protocol consists of 3, 30 second cycles using 3-6% sodium hypochlorite with a 30 second rest between each cycle, then removing the sodium hypochlorite with a 30 second distilled water cycle, followed by 1, 30 second cycle of 17% EDTA or QMix. The final rinse is a 30 second cycle of distilled water. After the final protocol, take cone fit radiographs, adjust as needed, dry the canals and obturate with your technique of choice. The total time cost of the final protocol is ~4 minutes and 30 seconds. The total time cost to use SWEEPS laser disinfection during the root canal procedure is ~2-3 minutes (4-6 SWEEPS cycles).
The allure of laser disinfection is it is an open irrigation system verses other systems that are closed (Ex. GentleWave). An open irrigation system allows the clinician to adjust the protocol as necessary. If bleeding is noted during the final protocol steps, then stop laser disinfection and proceed with SNI or the SLP EndoActivator. If a case presents with short roots, the final protocol can be shortened or the millijoules can be turned down to lessen the laser power. If an extremely, long, curvy canal is encountered the protocol can safely be lengthened. The more you SWEEPS the better you understand the immense acoustic shockwave power that occurs inside the canals and the more skilled you will become at using laser activated irrigation (SWEEPS and SSP). For example, I treated a maxillary second molar with canal lengths at 24 (MB, DB) and 25 mm (Palatal). The canals were curved and difficult to fully negotiate. In this specific case, I used 8 SWEEPS cycles from post- access to the completion of shaping. I then performed the final protocol and was able to complete a very difficult case in one visit and achieve a nice endodontic result.
LAI with the SWEEPS method is one avenue available to the clinician to improve chemical debridement, biofilm and smear layer removal. It is a simple technique to learn and does not interrupt the flow of the endodontic procedure. It is an open irrigation technique and can be adjusted down in mJ (power) or duration (seconds). It is safe and provides an effective, efficient, and excellent way to practice MIE. In conjunction with the ProTaper Ultimate shaping system, laser activated irrigation provides the clinician an opportunity to participate in the field of minimally invasive endodontics in the hopes of preserving tooth structure, debriding the root canal system and retaining the function of the tooth.
Oral Health welcomes this original article.
References
- Gluskin, A.H., Peters C.I., Peters, O.A. Minimally Invasive Endodontics: Challenging Prevailing Paradigms. British Dental Journal 2014;216:347-353.
- OMukherjee P, Patel A, Chandak M, Kashikar R. Minimally Invasive Endodontics a Promising Future Concept: A Review Article. Int J Sci Stud 2017;5(1):245-251.
- Nazari A, Bajaj D, Zhang D, Romberg E, Arola D . On the reduction in fracture toughness of human dentin with age. J Mech Behav Biomed Mater 2009; 2: 550–559.
- Koester K J, Ager J W 3rd, Ritchie R O . The effect of aging on crack-growth resistance and toughening mechanisms in human dentin. Biomaterials 2008; 29: 1318–1328.
- Wu M K, Dummer P M, Wesselink P R . Consequences of and strategies to deal with residual post-treatment root canal infection. Int Endod J 2006; 39: 343–356.
- Siqueira J F, Araújo M C, Garcia P F, Fraga R C, Sabóia Dantas CJ. Histological evaluation of the effectiveness of five instrumentation techniques for cleaning the apical third of root canals. J Endod 1997; 23: 499–502.
- Huffaker S K, Safavi K, Spangberg L S, Kaufman B . Influence of a passive sonic irrigation system on the elimination of bacteria from root canal systems: a clinical study. J Endod 2010; 36: 1315–1318.
- Klyn S L, Kirkpatrick T C, Rutledge R E . In vitro comparisons of debris removal of the EndoActivator system, the F file, ultrasonic irrigation, and NaOCl irrigation alone after hand-rotary instrumentation in human mandibular molars. J Endod 2010; 36: 1367–1371.
- Peters O A, Bardsley S, Fong J, Pandher G, Divito E . Disinfection of root canals with photon-initiated photoacoustic streaming. J Endod 2011; 37: 1008–1012.
- Molina B, Glickman G, Vandrangi P, Khakpour M. Evaluation of root canal debridement of human molars using the GentleWave system. J Endod. 2015;41(10):1701-1705.
- Yang Q, Liu M.W., Zhu L.X., Micro-CT Study on the Removal of Accumulated Hard- Tissue Debris from the Root Canal System of Mandibular Molars when using a Novel Laser-Activated Irrigation Approach. Int Endod J 2020; 53(4): 529-538.
About the Authors

Dr. Reid Pullen graduated from USC Dental school in 1999 and served 3 years in the Army dental corps in Landstuhl, Germany. He attended the Long Beach VA endodontic residency and graduated in 2006. Dr. Pullen opened a practice limited to Endodontics in Brea, CA in 2007 and achieved board certification in 2013. His hobbies include surfing, JiuJitsu, reading and golf. Dr. Pullen is the founder of rootcanalacademy.com and the 2 Day Root Camp Boot Camp course.










