
Osteoradionecrosis (ORN) remains one of the most serious and challenging oral complications following radiation-based head and neck cancer treatment. It is a severely delayed radiation-induced injury characterized by non-healing, bone tissue necrosis for at least three months.3
The most common site affected by ORN to occur is the mandible,5 where its incidence is between 2 and 22%.6 While there is a consensus regarding the clinical presentation of ORN, which consists of pain, drainage and fistulation of the mucosa or skin related to the exposed bone in an area that has been irradiated,2 there is significant debate about the mechanism by which it occurs.
Here, we present the case of a patient who experienced ORN following radiation treatment received 23 years before implant surgery.
Case Presentation
GD, an 85-year-old male, was referred our periodontal clinic by a local community dentist for intense jaw pain. GD is a non-diabetic whose comorbidities include hypertension, GERD, atrial fibrillation, and peripheral limb neuropathy. Surgical history includes bilateral TKAs. Medications include nifedipine, perindopril, metoprolol, rivaroxaban, pantoprazole, atorvastatin, gabapentin and oxazepam.
In 1999, GD had a growth on the left side of his neck about the size of half a golf ball. The biopsy was positive for squamous cell carcinoma. A resection was performed across his sternocleidomastoid muscle and jugular vein. In October 2000, a primary lump and multiple smaller masses with similar appearances began to appear bilaterally. GD received radiation treatment, which successfully allowed him to achieve remission. After five years of uneventful oncology follow-up, he was discharged from his oncologist’s care.
Regarding dental work before radiation treatment, the patient had a partial denture in the maxilla following a broken tooth around age 18. He also had extensive crown and bridge work in the mandible and saw his dentist regularly for periodontal maintenance.
Following radiation, the patient had several implants placed. In 2014, implants were placed at 11, 13, 15 and 45. He had an additional implant placed in 2021 at 46 and in quadrant two.
The patient reported that his implant at 46 had always had a gap underneath and was “wobbly” since placement. In October of 2022, it became infected and required removal by his dentist. He presented to us in June 2023.
Clinical Findings
The patient presented with severe jaw pain, which he reported as 9/10 in intensity. The jaw pain occurred four to five times daily for 45 minutes to an hour. In addition, he was experiencing numbness over their right lower lip that occurred randomly four to five times a day. He described the sensation as getting “tasered” or frozen. He qualified the sensation as feeling electrifying. It did not radiate and was localized to the lower right lip. These sensations would last for 30 minutes, and then they would go back to normal.
In addition, for approximately 4 to 5 weeks, once every four to five days, the patient would report a “gush of blood” when he would bend over. It would be gone after washing out his mouth, and it was unclear where it came from. The patient did not have any history of nosebleeds.
On physical examination, there was pain on palpation of the right cheek. In addition, there were two pus-producing fistulas in the 46 and 47 areas. (Fig. 1) There was no exposed bone.
Fig. 1

Diagnostic Assessment
Given the patient’s history of a mobile and subsequently failed implant (46) and a failing implant, it was logical to conclude that the patient initially had peri-implantitis at 46 before the implant was lost.
After that, given his intense jaw pain and draining fistulas in the 46 and 47 regions and his history of radiation therapy to the jaw, the differential diagnosis included osteoradionecrosis, osteomyelitis or a malignancy.
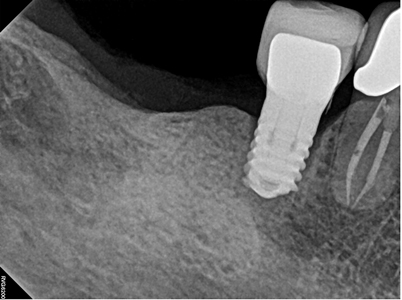
A CBCT revealed destruction of the cancellous bone and perforation of the cortex of the mandible. (Fig. 2) Figure 2 demonstrates the peri-implantitis at 45. The extent of the destruction of the bone in quadrant four is noted in Figure. 4.
Fig. 2

Fig. 3
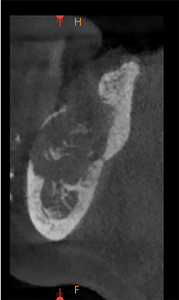
Fig. 4
Therapeutic Intervention
On his first visit, the patient was prescribed a 30-day course of cephalexin. When he returned for a follow-up two weeks later, his pain largely subsided, but his other symptoms remained. He was referred to an ENT specialist surgeon and oncologist for surgical management.
Discussion
The case presented here is consistent with the classical presentation of osteoradionecrosis. The site that was affected was the mandible, which is the most common site.4 Moreover, there was a history of surgical trauma, namely extractions and implant placement, to the area following radiation. The patient had an ill-fitting prosthesis rubbing against the ridge in quadrant four. All of these are risk factors for the development of osteoradionecrosis.3
Osteoradionecrosis and osteomyelitis are both conditions that affect bone, but different factors cause them and often require different approaches to diagnosis and treatment.
Osteoradionecrosis
Cause: Osteoradionecrosis occurs due to radiation therapy, often used to treat cancers. The radiation can damage healthy tissues and blood vessels, leading to a lack of oxygen and nutrients and eventually causing the bone to die
Location: Most commonly affects areas exposed to radiation, such as the jawbone in cases of head and neck cancer.
Symptoms: Pain, swelling, and exposed bone may be visible in the affected area. Sometimes, fistulas or pathological fractures can occur.
Onset: Symptoms can occur months or even years after radiation therapy.
Diagnosis: History of radiation to the area is critical for diagnosis. Imaging such as X-rays, CT scans, or MRIs may also be used.
Treatment: Surgical debridement, hyperbaric oxygen therapy, and antibiotics (if secondary infection is present) may be used. Surgical reconstruction might also be needed.
Osteomyelitis
Cause: Osteomyelitis is usually caused by bacterial infection, although fungi or other microorganisms can also cause it. The infection can occur due to various mechanisms, including direct inoculation of the bone (e.g., fracture, surgery), spread from nearby tissues, or via the bloodstream.
Location: Can affect any bone.
Symptoms: Fever, localized pain, and sometimes localized redness or heat are common.
Onset: Symptoms usually occur rapidly in acute cases but may be more insidious in chronic forms of the condition.
Diagnosis: Blood tests and imaging (X-rays, MRI, CT scans) are commonly used. Bone biopsy and culture may be needed to identify the causative organism.
Treatment: Long courses of antibiotics are generally the first line of treatment, and surgical debridement is often necessary to remove necrotic bone and tissue.
Understanding the underlying cause of the condition is essential for effective treatment. Both conditions can lead to severe complications if not properly managed.
There were several unique aspects of the case. Interestingly, the patient could tolerate five implants for a substantial period before developing osteoradionecrosis. Whereas most cases of ORN develop 6-12 months after radiotherapy,1 this patient developed ORN 23 years after the initial radiation and nine years after his first implant. Notwithstanding, the osteoradionecrosis began shortly after an episode of peri-implantitis.
This patient’s story highlights the importance of avoiding osseous surgery, including implants, in patients who have had radiation to the jaw.
Conclusion
In summary, the case presented here was of an 85-year-old male who received dental implants 14 years after radiation to the jaw. Nine years afterwards, he developed peri-implantitis and, subsequently, severe osteoradionecrosis. This case highlighted multiple risk factors for developing osteoradionecrosis: implant placement, an ill-fitting prosthesis, infection, and extraction. It also showcased an interesting scenario where the patient developed ORN 23 years after their radiation treatment was completed, highlighting there is no safe window for osseous surgery after radiation to the jaw. The case provides further evidence for avoiding dental implants and osseous surgery in patients with radiation to their jaws.
Oral Health welcomes this original article.
Acknowledgments: The authors thank Sandy Marchese for her assistance in preparing this paper.
References
- Epstein J, Wong F, Stevenson-Moore P. Osteoradionecrosis: clinical experience and a proposal for classification. J Oral Maxillofac Surg. 1987;45:104–111. doi: 10.1016/0278-2391(87)90399-5.
- Lyons A, Ghazali N. Osteoradionecrosis of the jaws: current understanding of its pathophysiology and treatment. Br J Oral Maxillofac Surg. 2008;46:653–660. doi: 10.1016/j.bjoms.2008.04.006.
- Nadella, K. R., Kodali, R. M., Guttikonda, L. K., & Jonnalagadda, A. (2015). Osteoradionecrosis of the Jaws: Clinico-Therapeutic Management: A Literature Review and Update. Journal of maxillofacial and oral surgery, 14(4), 891–901. https://doi.org/10.1007/s12663-015-0762-9
- Rathy, R., Sunil, S., & Nivia, M. (2013). Osteoradionecrosis of mandible: Case report with review of literature. Contemporary clinical dentistry, 4(2), 251–253. https://doi.org/10.4103/0976-237X.114882
- Schwartz HC, Kagan AR. Osteoradionecrosis of the mandible: scientific basis for clinical staging. Am J Clin Oncol. 2002;25:168–171. doi: 10.1097/00000421-200204000-00013.
- Store G, Boysen M. Mandibular osteoradionecrosis: clinical behavior and diagnostic aspects. Clin Otolaryngol Allied Sci. 2000;25:378–384. doi: 10.1046/j.1365-2273.2000.00367.x.
About the Authors

Abdul Arif is a second-year medical student studying at McMaster University. Prior to starting medical school, he completed an undergraduate degree at the University of Toronto, St. George Campus, specializing in biology, math and computer science. Abdul has a strong interest in the intersection of technology with healthcare.

Dr. Peter Fritz is an intrepid life-long, global learner. He leads an extraordinary, collaborative, empowered team of clinicians, scientists, explorers and artists who are all performing together to innovate the dental specialty of periodontics and to redefine the patient experience using their heads, hearts and hands.









