Abstract
Although immediate implant placement and provisionalization are now considered the standard of care and the preferred patient option for transitioning from edentulism or unrestorable teeth to implant rehabilitation, several clinical factors and patient characteristics can contraindicate this approach. As a result, it is still frequently necessary for clinicians to undertake—and for patients to endure—the multiple procedures associated with conventional implant therapies. Given the multiple surgeries, appointments, potential complications, and lengthy Extraction-to-Final Restoration Time (EFR-Time) linked to conventional implant placement and restoration protocols, a more streamlined procedure is imperative. Fortunately, the 5-in-1 technique represents a clinically efficient and predictable method for performing extractions, immediately placing implants, undertaking immediate sinus lifts when necessary, completing bone grafting, and placing a healing abutment and/or provisional restoration, all in one surgical appointment. This article elucidates the 5-in-1 Technique and how the protocol enhances the predictability and efficiency of providing patients with optimal, single-appointment implant treatments that significantly reduce EFR-Time.
Key words
5-in-1 technique, EFR-Time, Osseotransportation, Step-locking, Lateral grooves, Lateral flutes, sinus implant, one drill, Onedrill™, one drill implant
Dental implants have demonstrated remarkable success for nearly four decades in providing support for single and/or multiple unit restorations, affording patients the advantages of restored bite force, occlusal stability, comfort, and esthetics akin to those found in natural teeth. Unfortunately, the traditional implant placement and restoration protocol often entail multiple appointments, surgical and clinical procedures, and extended healing times that could extend over a period of 18 to 24 months or even longer.
Although immediate implant placement and provisionalization are regarded as the standard of care and the preferred patient option for transitioning from edentulism or unrestorable teeth to implant rehabilitation, certain clinical factors and patient characteristics make this approach unsuitable. As a result, it is still frequently necessary for clinicians to undertake—and for patients to endure—the multiple procedures associated with conventional implant therapies.
Under the traditional protocols, unrestorable teeth are extracted, followed by a healing period of 1 to 3 months. However, prolonged edentulism and/or extractions may lead to deficient bone volume and altered anatomy, which can have a negative impact on implant osseointegration and esthetics, and contribute to functional implant complications and failures.1
Therefore, pre-prosthetic bone grafts for preservation and augmentation is frequently necessary to maintain gingival tissue position, avert esthetic compromises, and ensure optimal implant placement, positioning, primary stability, and long-term osseointegration.2 This procedure typically demands an additional 3-to-8 months of healing, prolonging the treatment time to potentially 11 months, and involving further surgical interventions.
Bone grafts often entails one surgical procedure for harvesting chin or ramus bone blocks, followed by another surgery to place and stabilize the bone graft with pins.3 The placement of bone particulates and a membrane to fill any remaining gaps between the bone block and native bone may also be required.3 Assuming that all bone has successfully matured during the healing period, an implant can then be placed in the bony housing, aiming for primary stability.
However, these procedures are susceptible to various challenges. Autogenous bone harvesting through surgery at a donor site necessitates an adequate bone supply for harvesting; subsequent grafts may experience resorption, and multiple surgeries can exacerbate patient discomfort.4,5 Membranes could be exposed or lost, leading to incomplete bone growth and potentially resulting in treatment failure.2 Dehiscence, bone exposure, and soft tissue collapse can also contribute to bone block graft failure.2,6
Surprisingly, if implant placement proceeds after a bone graft, the osteotomy procedure itself necessitates the removal of approximately 50% of the grafted bone to accommodate and stabilize the implant. Subsequently, an additional 3-to-6 months of healing time is required for implant-to-bone osseointegration, after which yet another surgery is necessary to expose the implant and place an abutment.1
Although research substantiates an overall maxillary implant survival rate of 91%, the invasion of dental implants into the maxillary sinus cavity is a frequent complication caused by sinus pneumatization, a resorbed osseous ridge, and compromised bone quality and quantity, which is typically thin, porous, and lacking in volume.7-10 As inadequate alveolar bone height/volume and maxillary sinus anatomy can complicate the predictable placement of conventional implants and subsequent restoration,7-10 a sinus lift and vertical bone height augmentation may be required, along with the customary 4-to-12-month healing period prior to implant placement.11,12
Sinus lift and vertical bone height augmentation techniques have included, but are not limited to, open sinus lift procedures, in which autogenous cancellous bone is used for sinus augmentation.1,3,12 Open sinus lift procedures are notoriously clinically demanding, invasive, and traumatic, leading to postoperative swelling, pain, and discomfort for the patient.7,12
Only after ensuring sufficient bone quality and quantity, along with the integrity of the sinus membrane, if appropriate, can implant placement proceed. This has historically involved first locating and exposing the implant surgical site, then using a large round bur to smooth and flatten the occlusal surface of the crest of the alveolar ridge to prepare the implant site. Subsequently, a pilot hole is drilled, after which a series of drills with varying diameters are used to gradually expand the pilot hole until the width and depth approximate – but remain slightly smaller than – the diameter and length of the selected implant. After drilling the osteotomy, a countersink drill is used to widen the hole to the same diameter as the selected implant, and a tap is then used to create a thread within the site to allow insertion of the passive dental implant into the crestal bone.
Following 3-to-4 months of osseointegration, a second-stage surgery is performed to uncover the implant and place an abutment; after another 2 weeks-to-1-month of healing, the restoration is attached to the abutment to complete the dental implant-restoration complex. However, the process of uncovering the implant for abutment placement could reveal a loss of keratinized tissue, thereby necessitating a full-thickness flap, repositioning connective tissue graft, or free gingival graft surgical procedure.
Considering the multiple surgeries, appointments, potential risks for complications, and the lengthy Extraction-to-Final Restoration Time (EFR-Time) associated with the conventional implant placement and restoration protocol, a more streamlined procedure is imperative. Fortunately, advancements in dental implants, osteotomy armamentarium, materials, and protocols have facilitated the development of the “5-in-1 Technique,” which drastically shortens the EFR-Time from 18 months or more to a single visit. This article elucidates the “5-in-1 Technique” and how the protocol enhances the predictability and efficiency of providing patients with optimal, single-appointment implant treatments that significantly reduce EFR-Time.
5-in-1 Technique
The “5-in-1 Technique” embodies a clinically efficient and predictable approach for conducting extractions, immediate implant placements, socket preservation, sinus lifts when required, and the placement of a healing abutment or immediate provisional restoration without the need to reposition or manipulate soft tissue, all within a single surgical appointment. The authors have practiced and refined this technique for the past 13 years, tailoring the day-to-day protocol to suit each individual sicario and unique clinical case requirements.
The 5-in-1 Technique empowers dentists to offer patients a treatment with stability, functionality, and esthetics in a single surgery and appointment, sparing them the need to undergo multiple procedures,12-14 or endure prolonged discomfort. Consequently, the EFR-Time is significantly reduced from 18 to 24 months to just one appointment.
1. Extraction: With the 5-in-1 Technique, extractions are conducted by first administering local anesthesia, after which care is taken to extract unrestorable teeth and their roots using extraction elevators and forceps in a minimally invasive fashion. All residual root fragments, debris, and granulomatous tissue are then carefully cleaned from the socket using a curette.
2. Osteotomy and Implant Placement: A pivotal aspect of the 5-in-1 Technique is the use of a high-efficiency fluted, lateral-cutting drill (Onedrill™ OsseoFuse®) specifically designed for rapid dental implant placement in the crestal bone, reducing operation time significantly (e.g., as little as 50 seconds per implant site with a flapless protocol).12,15 Engineered to eliminate the need for changing drill armamentarium, minimize errors, and enhance the predictability of implant treatment success, the Onedrill™features a stopper positioned at the base of the latch engagement, an initial drill, and a drill guide located at the apical/distal end, as well as a series of different diameter active drill body sections extending proximally from the initial drill to the base of the stopper in stepped increments of increasing diameter (i.e., from the smallest to the largest) (Figs. 1 & 2).12,15,16 Once the required implant size is determined, a corresponding size Onedrill™ can be selected to complete the osteotomy from start to finish.
Fig. 1 & 2
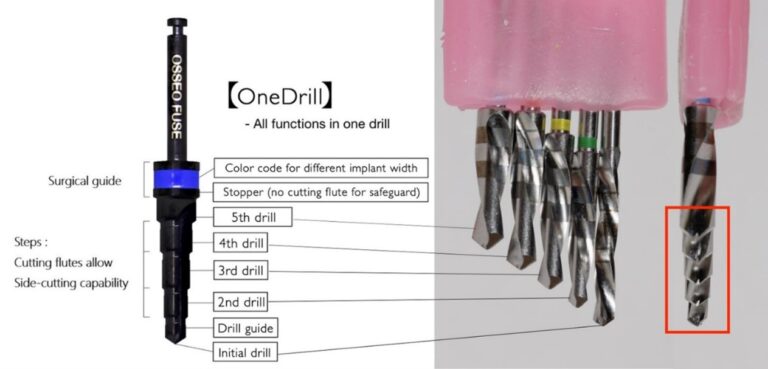
The initial drill and drill guide serve to facilitate location marking while preventing any skipping or digressive motion. The drill’s safeguard design (i.e., stopper) also ensures that the surgeon does not drill too deep. Subsequently, the first “step” of the Onedrill™ acts as the second drill, featuring an increased diameter equivalent to the second drill used in the traditional method, thereby eliminating the need to switch to another drill. The same principle applies to the subsequent “steps” along the trajectory of the Onedrill™. As the Onedrill™progresses through the osteotomy site, it effectively shapes the osteotomy bone into multiple steps of both over-drilled and under-drilled areas. These bony “steps” form the foundation for the “step-locking” concept, which establishes primary stability when immediately placing dental implants.
The step-locking concept is achieved when the tapered implant body, with sharp active threads and lateral cutting grooves (e.g., OsseoFuse® HexaPlus™ dental implants; OsseoFuse® SinusFuse® dental implants), is inserted. The tapered implant body shaves off the portion of the under-drilled autogenic bony “steps” of the osteotomy site during the insertion process (Fig. 3). As the implant is inserted and torqued into position, the shaved-off bone powder from the under-drilled zone is redistributed into the over-drilled zone, thereby releasing pressure and “step-locking” the implant into its optimal stability. It is crucial that the body of the implant fixture, when placed, does not compress the under-drilled areas of the osteotomy site.
Fig. 3
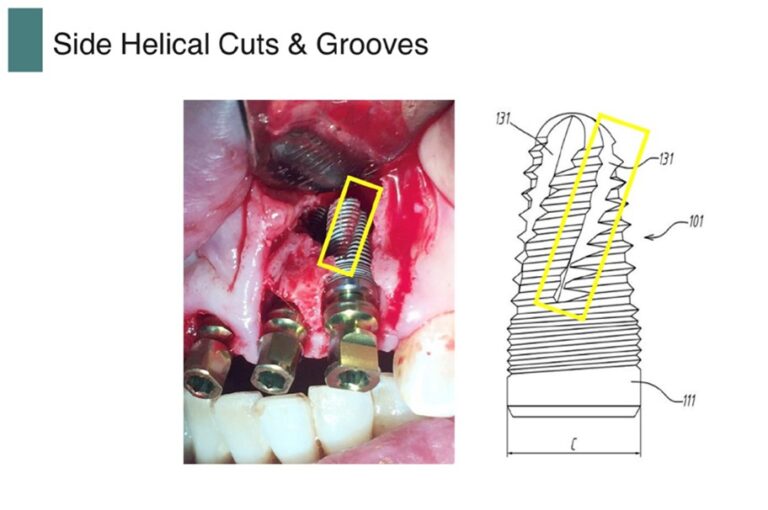
Additionally contributing to step-locking and primary stability with the 5-in-1 Technique is how the implant’s lateral cutting grooves and flutes complement and integrate with the unique cutting design of the Onedrill™. The lateral cutting flutes function akin to sharp knife threads, mechanically locking any bone in close contact with them, while the deep lateral grooves act as a reservoir for the autogenous bone. Furthermore, the implant itself serves as a final drill with a self-tapping function. In instances of implant failure, the Onedrill™ system incorporates a fail-safe protocol whereby the unsuccessful dental implant is simply extracted, and the socket is meticulously cleaned before promptly replacing the implant with one boasting a diameter two sizes larger from the same product line, all within the same visit. This stands in contrast to the conventional approach involving implant removal, bone grafting, and a subsequent waiting period of 3-4 months to ensure the bone’s suitability for another implant placement. This protocol distinctly presents a reliable contingency plan for cases where implant integration falls short. As the entire Onedrill™ system operates on a unified platform, a single abutment design seamlessly accommodates all fixture diameters.17
The merits of this protocol extend to enhanced patient contentment and optimized time management due to the possibility of same-day replacement. Moreover, it garners dentist satisfaction through its unified platform attribute, negating the necessity for abutment replacement when transitioning to a wider implant. Instead, the same abutment can be seamlessly employed for an implant of expanded diameter.17 Moreover, this approach only marginally extends the overall EFR-Time, as opposed to the prevailing norm among implant systems. If a dentist were to adhere to the conventional protocol, resulting in a substantial extension of the EFR-Time, it could potentially impact patient acceptance and undermine the trust vested in the dentist.
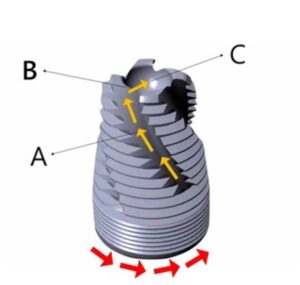
3. Osseotransportation (Sinus Lift): In cases where sinus lifts are required, the 5-in-1 Technique incorporates the use of a specially designed sinus implant (OsseoFuse® SinusFuse®). This sinus implant allows dentists to place dental implants at sites with as little as 2mm of native bone. An osteotomy is drilled into the crest of the alveolar ridge, stopping roughly 0.5mm from the maxillary sinus floor. Designed specifically for implant placement beneath the sinus membrane, the threaded sinus implant (OsseoFuse® SinusFuse®) features multiple reverse helical lateral cutting grooves that shave the autogenous bone during insertion (Fig. 4A). Subsequently, the autogenous bone particles are transported apically from the reversed helical lateral cutting grooves and are collected in the specially designed, concave dish-like reservoir at the apex of the implant (Fig. 4C).8,12,18-22 The unique cutting design at the apex of the implant effectively up-fractures the sinus cortical floor into the last 0.5mm (Fig. 4B), while simultaneously lifting the sinus membrane via the reservoir with excess autogenous bone. This instant harvest and simultaneous transportation of autogenous bone from one site to another, without exposure to the external environment, is referred to as Osseotrasportation. These features ensure safety during the sinus augmentation procedure and contribute to the enhanced build-up of the bone layer between the Schneiderian membrane and the sinus implant, promoting greater bone-to-implant surface contact.
Fig. 4
4. Bone Grafting: Given the characteristics of the drill and implants utilized in the 5-in-1 technique, along with their capacity to relocate bone powder to promote primary stability, there is no need for invasive bone grafting procedures. In fact, since the implant itself occupies 50% of the recessed space, less bone graft material is necessary. Once maximal primary stability is attained, only a minimal amount of anorganic bovine bone grafting material (Bio-Oss®, Geistlich Pharma North America, Inc.) is required to fill any remaining areas not occupied between the implant fixture and native bone.
5. Abutment and Provisionalization: With the maximum primary stability of the implant achieved, a wide healing abutment or provisional restoration can be promptly placed, eliminating the necessity for a second stage uncovering surgery, the potential for future keratinized tissue loss, and the need for subsequent soft tissue grafts. Besides providing the patient with functionality and esthetics, the immediate provisional restoration also acts as an external membrane/periodontal dressing, safeguarding the gingival tissues surrounding the implant. This further prevents food particles and external pressure (e.g., tongue and cheeks) from irritating the bone graft site and provides added stabilization.
Case #1
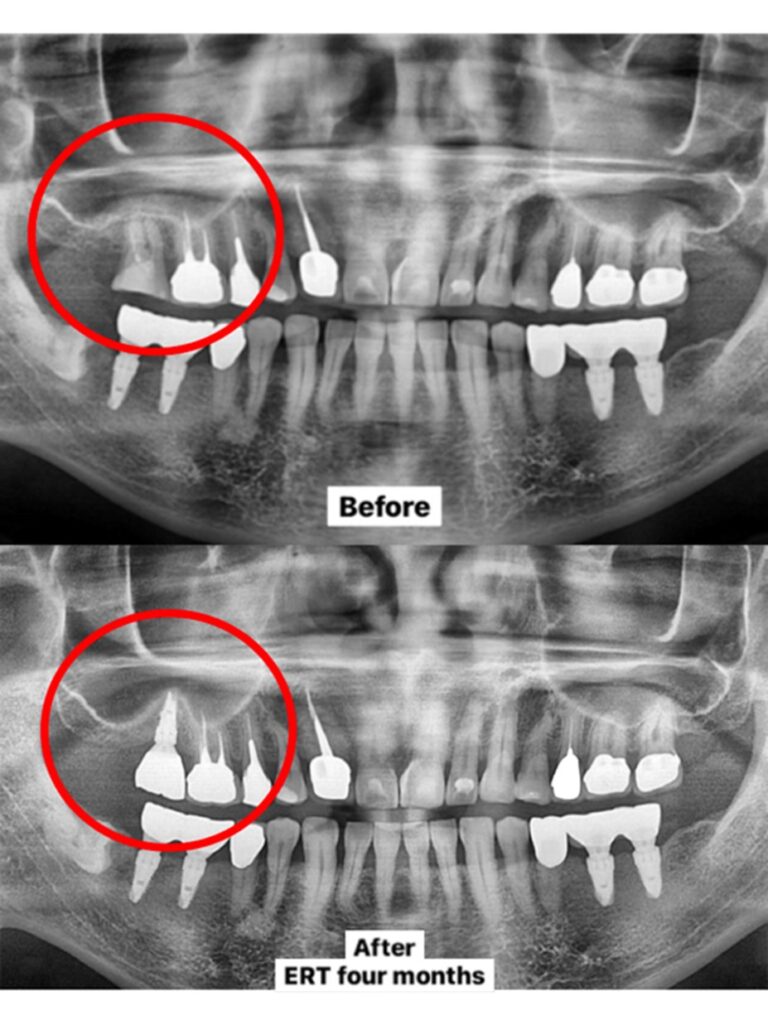
A 58-year-old male, who had previously undergone implant procedures at #18, #19, #30, and #31 and expressed satisfaction with the outcomes, presented with a vertical fracture on tooth #2 following multiple unsuccessful attempts at root canal therapy, leading to severe pain. A comprehensive medical history, intraoral, and radiographic examination were conducted, unveiling the proximity of the sinus floor to the root tip (Fig. 5).
Fig. 5

The patient consented to undergo the 5-in-1 technique, encompassing extraction, implant placement, sinus lift, bone graft, and the placement of a wide gingival healing abutment. Local anesthetic was administered using one carpule of lidocaine, following which tooth #2 was extracted, and the socket was meticulously cleaned of granulomatous tissue. The osteotomy was performed using a one implant drill system (Onedrill™ OsseoFuse® 4.5×10), drilling 0.5mm short of the sinus floor. Subsequently, a 4.5×10 sinus implant (OsseoFuse® SinusFuse®) was inserted to up-fracture the sinus floor. During implant insertion, the specialized sinus implant fixture transported the patient’s autogenic bone to the concave dish-like reservoir of the implant, simultaneously elevating the Schneiderian membrane.
Furthermore, due to the selected implant’s step-locking capabilities, it achieved primary stability, allowing for the placement of a minimal amount of anorganic bovine bone grafting material (Bio-Oss®, Geistlich Pharma North America, Inc.) to fill any remaining areas not occupied between the implant fixture and native bone. This also facilitated the immediate placement of a wider healing abutment, securing the bone graft material while assisting in the formation and preservation of the keratinized tissue surrounding the implant. Consequently, additional surgeries were unnecessary (Fig. 6), effectively reducing the total EFR-Time to only 4 months (Fig. 7).
Fig. 6

Fig. 7
Case #2
A 50-year-old female executive at a prominent corporation, who grappled with dental phobia, sought treatment for generalized moderate and localized severe periodontitis. Thorough intraoral and radiographic examinations revealed that the majority of severely infected, periodontally involved, and unrestorable teeth exhibited class two and three mobility (#1-4; #17, #19; #23-25, #26; #30 and #31) (Fig. 8). The patient expressed the desire for all procedures to be carried out in a single appointment and willingly agreed to undergo the 5-in-1 Technique treatment plan.
Fig. 8
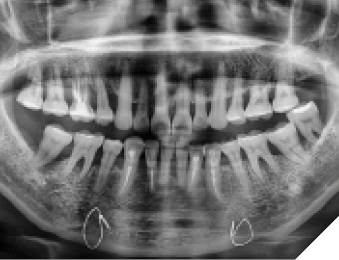
Local anesthesia was administered, following which preliminary impressions were taken to create immediate provisional restorations. All unrestorable teeth were extracted, and the infected sockets were meticulously cleaned, with the sites receiving topical tetracycline treatment.
The osteotomies and any necessary sinus lifts were performed using the one drill implant system (Onedrill™ OsseoFuse®). Subsequently, the appropriate implants (OsseoFuse® SinusFuse®; OsseoFuse® HexaPlus™) were inserted based on site requirements and torqued to 50ncm. It is noteworthy that each drill size corresponds to a specific tapered implant size, thereby optimizing their respective abilities to achieve step-locking and maximal primary stability (Fig. 9).
Fig. 9
As part of the sinus lifting procedure, and to fill any gaps between the native bone and implants, anorganic bovine bone grafting material (Bio-Oss®, Geistlich Pharma North America, Inc.) was employed, obviating the need for membrane barriers or sutures. In select sites, a flap was created to facilitate scaling and root planning of the remaining but periodontally compromised teeth.
Provisional restorations (Luxatemp, DMG) were positioned in esthetic areas, while wide healing abutments (OsseoFuse® Temporary Abutment) were affixed in the posterior regions, aiding in the preservation of the keratinized tissue (Fig. 10).
Fig. 10

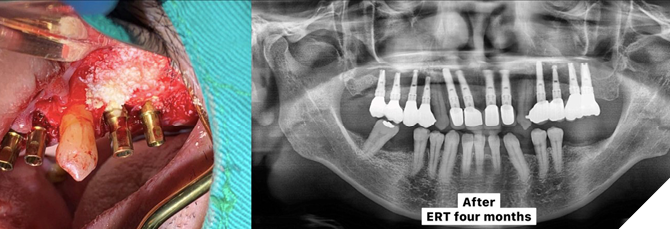
Four months after the completion of the 5-in-1 Technique, final impressions were taken, obviating the necessity for a second surgery or additional local anesthesia (Fig. 11). The final restorations were provided one week later, resulting in a total treatment time of only 5 months from the extractions to the placement of the final crowns. Throughout this period, the patient could enjoy the advantages of provisional restorations and maintain her regular daily routine. Consequently, the once dental phobic patient is now enthusiastic about undergoing future cosmetic dental procedures.
Fig. 11

Case #3
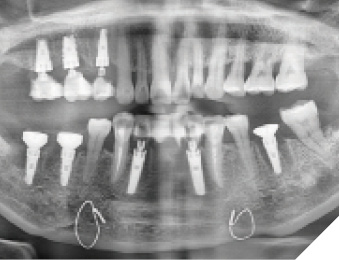
A 53-year-old male presented with several missing and other unrestorable teeth. He was a heavy smoker with a demanding travel schedule, leaving him with limited time for dental care. He expressed the desire for comprehensive oral rehabilitation but emphasized the completion of his maxillary arch first, in a single appointment, with immediate provisional restorations to preserve his business and social functions.
Comprehensive medical history, intraoral, and radiographic examinations were conducted, revealing sites with residual roots (Fig. 12). It was decided that the 5-in-1 Technique would be employed to extract all unrestorable teeth (#1, #7-10, #12, and #13) as well as the missing teeth (#2-5, #14-16), perform sinus lifts, bone grafts, immediately place implants, and provide the patient with provisional restorations. Teeth #6 and #11 would remain on the maxillary arch.
Fig. 12

Local anesthesia was administered, preliminary impressions were taken to create immediate provisional restorations, and all unrestorable teeth and root tips were extracted. Osteotomies and any necessary sinus lifts (at #2, #3, #14, and #15) were performed using the one drill implant system (Onedrill™ OsseoFuse®), after which the appropriate implants (OsseoFuse® SinusFuse®; OsseoFuse® HexaPlus™) were inserted based on site requirements and torqued to 50 ncm (Fig. 13 & 14).
Fig. 13 & 14
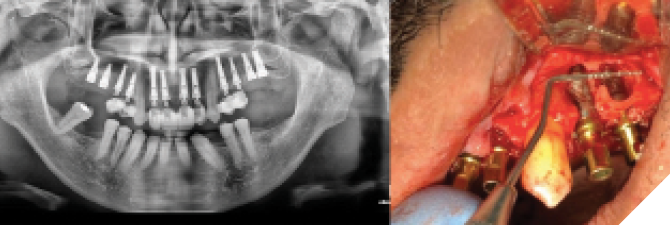
As part of the sinus lifting procedure, and for filling any gaps between the native bone and implants, bone graft material (Bio-Oss®, Geistlich Pharma North America, Inc.) was utilized, rendering artificial membranes unnecessary. Healing and/or immediate provisional abutments were affixed (OsseoFuse® Temporary Abutment), and provisional restorations (Luxatemp, DMG) were installed, providing protection to the periodontal tissues from external pressures and ensuring cross-arch stabilization. The placement of healing and/or immediate provisional abutments also contributed to the preservation of keratinized tissue, eliminating the need for a second uncovering surgery (Fig. 15).
The patient received postoperative home care instructions and returned for regular follow-ups and any necessary adjustments to ensure a balanced occlusion. Ultimately, he expressed satisfaction with the definitive restorations (Fig. 16).
Fig. 15 & 16
Conclusion
The 5-in-1 technique epitomizes a clinically efficient and reliable approach for conducting extractions, immediate implant placement, necessary immediate sinus lifts, bone grafting, and the placement of healing abutments and/or provisional restorations, all within a single surgical appointment. The paramount advantages of implementing the 5-in-1 Technique encompass a streamlined single-stage surgical procedure, wherein extraction, implant placement, bone augmenting material placement, and simultaneous fixed provisional restoration placement occur simultaneously. This approach obviates the need for bone block grafts, stabilization pins, and membranes, as the implant attains optimal primary stability through the step-locking concept, acting as a tinting screw/large scaffold for the bone graft material.
The technique empowers dentists to deliver a one-surgery treatment, exemplifying stability, functionality, and esthetics, without subjecting patients to multiple procedures or prolonged discomfort, as supported by previous studies. While future clinical investigations are imperative to validate the long-term efficacy of this approach, strict adherence to the presented protocol enables the immediate placement and provisional restoration of an implant, meeting the growing demand for immediate extraction/implant/provisionalization options. By employing this technique, the comprehensive treatment of this area, inclusive of extraction, bone graft/sinus lift, implant placement, and restoration, can be accomplished within a span of only 3-5 months, signifying a significant reduction in the overall EFR-Time. 
Oral Health welcomes this original article.
References
- Mahesh L, Kurtzman GM, Bali P, Kumar VR. Preserving the buccal plate with a novel bone graft material for immediate implants in the esthetic zone. Journal Implant & Advanced Clinical Dent. 2019;11(3): 6-12.
- Checchi V, Gasparro R, Pistilli R, Canullo L, Felice P. Clinical classification of bone augmentation procedure failures in the atrophic anterior maxillae: esthetic consequences and treatment options. Biomed Res Int. 2019; 2019: 4386709.
- Cordaro L, Torsello F, Accorsi Ribeiro C, et al. Inlay-onlay grafting for three-dimensional reconstruction of the posterior atrophic maxilla with mandibular bone. International Journal of Oral and Maxillofacial Surgery. 2010;39(4):350–357.
- Chiapasco M, Zaniboni M. Failures in jaw reconstructive surgery with autogenous onlay bone grafts for pre-implant purposes: incidence, prevention and management of complications. Oral and Maxillofacial Surgery Clinics of North America. 2011;23(1):1–15.
- Sbordone L, Toti P, Menchini-Fabris GB, et al. Volume changes of autogenous bone grafts after alveolar ridge augmentation of atrophic maxillae and mandibles. International Journal of Oral and Maxillofacial Surgery. 2009;38(10):1059–1065.
- Barone A, Varanini P, Orlando B, Tonelli P, Covani U. Deep-frozen allogeneic onlay bone grafts for reconstruction of atrophic maxillary alveolar ridges: a preliminary study. Journal of Oral and Maxillofacial Surgery. 2009;67(6):1300–1306.
- Ardekian L, Levit L, Michael L. Acute sinusitis and implant failure following novel minimally invasive hydraulic sinus lift: a case report. Clin Surg. 2018; 3: 1882.
- Chen L, Cha J. An 8-year retrospective study: 1,100 patients receiving 1,557 implants using the minimally invasive hydraulic sinus condensing technique. J Periodontol. 2005 Mar;76(3):482-91.
- Chen L, Cha J, Chen H-C, Lin HL. Sinus perforation: treatment and classifications. The Journal of Implant & Advanced Clinical Dentistry. 2011; 3(1):19-30.
- Chen L, Cha J. Dental implant migration into two different maxillary sinus cavities. The Journal of Implant & Advanced Clinical Dentistry. 2011; 4(4):21 -25.
- Stern A, Green J. Sinus lifts procedures: an overview of current techniques. Dent Clin North Am. 2012;56(1):219-33.
- Chen L, Cha J. Achieving predictable hydraulic sinus condensing using an innovative functional sinus implant: a case report. Compend Contin Educ Dent. 2020;41(5):278-283.
- Degidi M, Nardi D, Daprile G, Piattelli A. Buccal bone plate in the immediately placed and restored maxillary single implant: a 7-year retrospective study using computed tomography. Implant Dent. 2012 Feb;21(1):62-6.
- Clementini M, Tiravia L, De Risi V et al. Dimensional changes after immediate implant placement with or without simultaneous regenerative procedures: a systematic review and meta-analysis. J Clin Periodontol. 2015 Jul;42(7):666-77.
- Chen L, Cha J. OsseoFuse One Drill System: a 6-year retrospective follow-up of over 250 implants. Journal Implant & Advanced Clinical Dent. 2017;9(6):6-15.
- Chen L, Chen N, Chen A, Chen A, Chen N, Chen N. “A One-Drill System for Predictable Osteotomy and Immediate Implant Placement”. EC Dental Science 22.1 (2023) 114-128.
- Leon Chen and Niq Chen. “Immediate Reimplantation at Failed Osseointegration Sites: A Drilling and Systematically Increasing Implant Width Protocol to Ensure Primary Stability”. EC Dental Science 22.5 (2023): 22-35.
- Chen L, Cha J, Chen HC. Two different clinical indications using hydraulic sinus condensing (HSC) technique: ten years follow-up. Dent Implantol Update. 2009 May;20(5):33-8.
- Chen L. Correcting maxillary sinus deficiencies. Dent Implantol Update. 2008 Oct;19(10):65-70.
- Li J, Lee K, Chen H, Ou G. Piezoelectric surgery in maxillary sinus floor elevation with hydraulic pressure for xenograft and simultaneous implant placement. J Prosthet Dent. 2013 Nov;110(5):344-8.
- Kim YK, Cho YS, Yun PY. Assessment of dentists’ subjective satisfaction with a newly developed device for maxillary sinus membrane elevation by the crestal approach. J Periodontal Implant Sci. 2013 Dec;43(6):308-14.
- Gatti F, Gatti C, Tallarico M, et al. Maxillary sinus membrane elevation using a special drilling system and hydraulic pressure: A 2-year prospective cohort study. Int J Periodontics Restorative Dent. 2018 Jul/Aug;38(4):593-599.
About the Authors

Leon Chen is the founder and CEO of The Dental Implant Institute in Las Vegas. He is also the developer of the patented Hydraulic Sinus Condensing (HSC™) technique, as well as other techniques. Additionally, he is a Fellow and Diplomate of the International Congress of Oral Implantologists. He serves on multiple advisory boards, lectures extensively throughout the United States and internationally, and is an award-winning humanitarian.

Aleq Chen is in private practice in Madrid. He is the executive assistant at The Dental Implant Institute in Las Vegas and OsseoFuse Onedrill Dental Implant System. He is actively designing algorithmic software for immediate implants.

Nina Chen actively participates in dental conferences worldwide and works at The Dental Implant Institute in Las Vegas. She graduated from Universidad Europea de Madrid in Spain and is currently pursuing a postdoctoral program in periodontics at New York University College of Dentistry.

Niq Chen is the CTO of The Dental Implant Institute in Las Vegas and a graduate of Universidad Europea de Madrid. He is currently enrolled in a postdoctoral program in periodontics at Columbia University College of Dental Medicine.

Nasdaq Chen is the CFO of The Dental Implant Institute in Las Vegas and OsseoFuse Onedrill Dental Implant System. He is actively engaged in developing algorithmic software for immediate implants.