Implant therapy has become a predictable treatment option for tooth replacement with a 5-year survival rate of 97.1%.1 Despite this high survival rate, implant failure can still happen which would necessitate removal, or better said, explantation of the unsuccessful implant. Approximately 34% of failures occur within the first 5 years after placement and it could be due to biologic, mechanical, iatrogenic and/or functional reasons.2
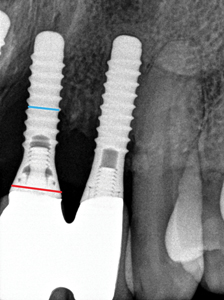
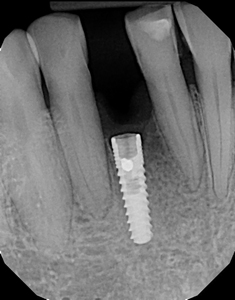
In reality, one may have a still osseointegrated implant which is not mobile and yet it’s considered as a failed implant which has to be removed. Examples of these situations are: advanced peri-implantitis (Biologic failure), (Fig. 1) poorly positioned implants which makes them either non-restorable or a challenge to aesthetics and fractured or damaged implants. (Fig. 2) Peri-implantitis which manifest itself as progressive bone loss around the implants is the main cause for implant failure.3 Perhaps the least challenging form of failure is when there is a total biologic failure with a complete loss of osseointegration in which case the failed implant can easily be removed using an extraction forceps.
Fig. 1
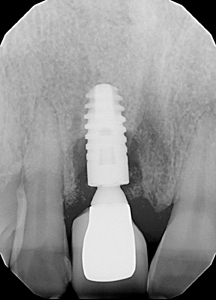
Fig. 2A

Fig. 2B

Unlike natural teeth, implants don’t become mobile as they lose bone support. Presence of only few apical threads surrounded by bone would mean that the implant is still osseointegrated and not necessarily easy to explant.
This article is a review of the available techniques for implant removal.
Reverse torque devices:
This method by far is the least invasive way of removing osseointegrated dental implants.4 These devices are designed based on the concept of unscrewing the implant while employing high levels of force in a counter clockwise direction. The threads on these removal devices are designed in a reversed fashion resulting in a greater clamping effect between the device and the implant as counter clockwise force is being applied. (Fig. 3)
Fig. 3A

Fig. 3B
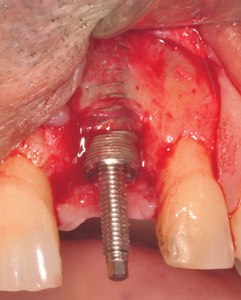
Fig. 3C
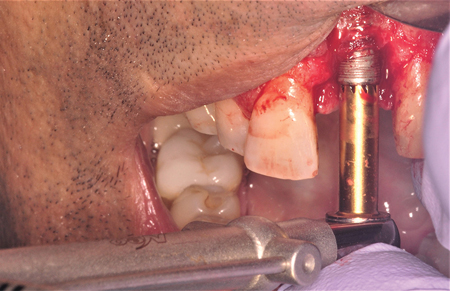
Fig. 3D

Fig. 3E

The amount of force required to unscrew an osseointegrated implant depends on several factors including implant shape (tapered being easier than cylindrical), surface characteristics,5 thread design,6 bone quality, and the amount of remaining apical bone around the implant. In general, due to presence of more dense bone, reverse torquing implants in mandible requires higher amount of force compared to that of maxilla. Also, this technique is more effective when no more than 4mm of bone at the implant’s apical part is left.3,7
In order to use this device the prosthesis must first be removed to provide access to the implant platform. Unlike screw-retained crowns, removal of cement retained prostheses could be time consuming and in some cases slightly challenging.
More-over, the internal threads of the implant must be intact to allow for engagement of the fixture remover screw. This method cannot be used on implants that rely on locking mechanisms such as Morse tapered designs with no abutment screw (e.g. Bicon implant system). (Fig. 4)
Fig. 4
Because of high torque levels, this technique is more effective in removing implants with internal connection as compared with those with external connection.
For implants with damaged internal threads a similar technique known as reverse screw technique can be used.8 However, there will be higher risk for implant fracture because of the wedging effect of the reverse screw inside the implant.
Trephine drills:
Using trephines is perhaps the oldest and yet one of the most aggressive methods of implant removal. Explanting osseointegrated implants with a trephine drill will require direct access to the implant with no prosthesis. (Fig. 4)
Beside removing too much bone there is also a potential risk for damage to adjacent teeth and release of titanium particles during implant removal using trephine drills (9); therefore, a proper drill size corresponding to the implant diameter must be used. In older non-platform switch implants, a straight healing abutment can be placed on the implant to guide the trephine drill.
There is a possibility for heat-induced bone necrosis particularly as one drills deeper into the apical portion of the implant.9,10 It is important to use sharp trephine with copious irrigation at a maximum speed of 800RPM.
Trephine drill is not the right choice for removal of tissue level implants with flared implant neck. (Fig. 5)
Fig. 5A

Fig. 5B

Fig. 5C

Piezo surgery:
Piezo surgery is a relatively conservative bone removal approach when compared to rotary devices. Using a high frequency piezo can make a precise cut around the implant to facilitate its removal when used in combination with the reverse torque device or forceps/elevator. Piezo’s selective bone cutting is particularly advantageous when the implant is close to a neurovascular structure.11
Electrosurgery:
Exposing bone to temperatures between 47 and 55 for one minute can cause irreversible tissue damage.12
Some clinicians have used electro-surgery for implant removal.13,14 In a case report study Cunliffe et al. used mono-polar electrosurgery (the type commonly used in dentistry) for 15 seconds on an osseointegrated implant and showed that implant removal torque dropped to below 30Ncm only one week after application.13
Electrosurgery can cause a rise in temperature in the bone immediately surrounding the implant. This would lead to bone necrosis resulting in failure of osseointegration. The potential drawback of this method is that for it to work, osteonecrosis needs to take place which may have negative consequences particularly if new implant placement in the same spot is being considered.
This method has so far been used only in case reports or experimental animal studies. One of the main challenges with this technique is the inability to control the amount of temperature rise in the bone-implant interface.12,15-19 as uncontrolled heat trauma can potentially lead to extensive bone necrosis and damage to surrounding anatomical structures.
Fig. 6
Laser:
Research supporting use of hard tissue laser for implant removal is scarce. In a case report study, authors reported using Er.Cr:YSGG laser to remove an implant. Hard tissue laser cuts bone in a conservative way through hydrokinetic effect while providing simultaneous hemostasis. Authors suggested that this method was less invasive as compared with other techniques for implant removal.20 Further clinical studies are needed to support use of laser in general for implant removal.
Combination techniques:
Occasionally clinicians may have to use a combination of explantation techniques in order to remove an implant.
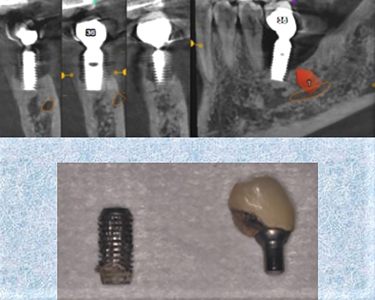
As expected, in many cases, using elevator and forceps alone is not very successful in removing osseointegrated implants. However, this method could be really useful when used in combination with resective techniques. The main indication is when there is proximity to adjacent roots and, for any of the reasons discussed earlier, a reverse torque implant removal device cannot be used. In this scenario explantation using other techniques may come with a high risk of damaging adjacent teeth. (Fig. 7)
Fig. 7
In situations like this, the clinician can use a long shank thin high speed bur or piezo to remove bone around the implant in the accessible areas and then carefully use an elevator to push the implant towards that direction and ultimately remove it with a forceps.
Likewise using the reverse torque implant removal technique alone may not be very effective if the remaining height of the still integrated implant is 4mm or greater. In these situations, reverse torque levels even as high as 200Ncm may fail to remove the implant. To overcome this, it is recommended to use trephines or thin high speed burs or piezo to remove additional 1-2mm of bone around the implant in order to reduce its removal torque.7
Conclusion:
Reverse torque technique remains the least invasive technique in removing failed osseointegrated implants. However, if the remaining bone height at the apical region of the implant is 4mm or more and/or removal torque exceeds 200Ncm, this technique should be combined with osseous resective techniques such as trephine drills, burs or piezo. Further studies are required to verify the effectiveness of electrosurgery and laser is removing osseointegrated implants.
Oral Health welcomes this original article.
Contact Information:
Email: termei@gtaperio.com
Address: GTA North Periodontics & Endodontics, 1650 Elgin Mills Rd. East, #305, Richmond Hill, ON L4S-0B2.
www.gtaperio.com
References
- Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A (2012) A systematic review of the survival and complication rates of implantsupported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res 23(Suppl 6):22–38.
- Esposito, M., Thomsen, P., Ericson, L. E., Sennerby, L., & Lekholm, U. (2000). Histopathologic observations on late oral implant failures. Clinical Implant Dentistry and Related Research, 2, 18–32.
- Solderer, A.; Al-Jazrawi, A.; Sahrmann, P.; Jung, R.; Attin, T.; Schmidlin, P.R. Removal of failed dental implants revisited: Questions and answers. Clin. Exp. Dent. Res. 2019, 21, 270.
- Froum, S., Yamanaka, T., Cho, S. C., Kelly, R., James, S. S., & Elian, N. (2011). Techniques to remove a failed integrated implant. Compendium of Continuing Education in Dentistry, 32(22–6), 28.
- Cho SA, Jung SK (2003) A removal torque of the laser-treated titanium implants in rabbit tibia. Biomaterials 24(26): 4859–4863.
- Misch, C. E., & Resnik R.. 2017. Misch’s avoiding complications in oral implantology—E-book.
- Balaji, S.M. Textbook of Oral & Maxillofacial Surgery; Elsevier India: Chennai, India, 2018; ISBN 9788131248744.
- Anitua, E., & Orive, G. (2012). A new approach for atraumatic implant explantation and immediate implant installation. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 113, e19–e25.
- Braegger, U.; Gigandet, M.; Vizek, J.; Hegnauer, U. Device for Detachment and Explantation of Bone Implants. U.S. Patent US20130071813A1, 21 March 2013.
- Petersen, J.Ø.; Cattaneo, P.M. US Device for Loosening, Insertion and Removal of Dental Implants. U.S. Patent 11184292.8, 4 September 2014.
- Messina, A. M., Marini, L., & Marini, E. (2018). A step-by-step technique for the piezosurgical removal of fractured implants. Journal of Craniofacial Surgery, 04, 04.
- Kniha, K.; Heussen, N.; Weber, E.; Möhlhenrich, S.C.; Hölzle, F.; Modabber, A. Temperature Threshold Values of Bone Necrosis for Thermo-Explantation of Dental Implants-A Systematic Review on Preclinical In Vivo Research. Materials 2020, 13, 3461.
- Cunliffe, J.; Barclay, C. Removal of a dental implant: An unusual case report. J Dent Implant 2011, 1, 22.
- Massei, G.; Szmukler-Moncler, S. Thermo-explantation. A novel approach to remove osseointegrated implants. Eur. Cells Mater. 2004, 7, 48.
- Eriksson, A.; Albrektsson, T.; Grane, B.; McQueen, D. Thermal injury to bone. A vital-microscopic description of heat effects. Int. J. Oral Surg. 1982, 11, 115–121.
- Eriksson, R.A.; Albrektsson, T.; Magnusson, B. Assessment of bone viability after heat trauma. A histological, histochemical and vital microscopic study in the rabbit. Scand. J. Plast. Reconstr. Surg. 1984, 18, 261–268.
- Li, S.; Chien, S.; Brånemark, P.I. Heat shock-induced necrosis and apoptosis in osteoblasts. J. Orthop. Res. 1999, 17, 891–899.
- Goetz, J.E.; Robinson, D.A.; Pedersen, D.R.; Conzemius, M.G.; Brown, T.D. Cryoinsult parameter effects on the histologically apparent volume of experimentally induced osteonecrotic lesions. J. Orthop. Res. 2011, 29, 931–937.
- Kniha, K.; Buhl, E.M.; Hermanns-Sachweh, B.; Al-Sibai, F.; Bock, A.; Peters, F.; Hölzle, F.; Modabber, A. Implant removal using thermal necrosis-an in vitro pilot study. Clin. Oral Investig. 2021, 25, 265–273.
- Smith LP, Rose T (2010) Laser explantation of a failing endosseous dental implant. Aust Dent J 55(2):219–222.
About the Author
 Dr. Reza Termei is a periodontist in Richmond Hill, Ontario. He is also a clinical instructor and a lecturer at the graduate and undergraduate levels at the Faculty of Dentistry, University of Toronto. Dr. Termei is a fellow of the Royal College of Dentists of Canada (RCDC) and Diplomate of the American Board of Periodontology. He is an examiner of the RCDC fellowship exam. He is also actively involved in running continuing dental education courses including implant trainings for dentists. Dr. Termei has served as former director and president of the Iranian Ontario Dental Association (IODA). He has also led several outreach dental mission trips to outreach communities abroad.
Dr. Reza Termei is a periodontist in Richmond Hill, Ontario. He is also a clinical instructor and a lecturer at the graduate and undergraduate levels at the Faculty of Dentistry, University of Toronto. Dr. Termei is a fellow of the Royal College of Dentists of Canada (RCDC) and Diplomate of the American Board of Periodontology. He is an examiner of the RCDC fellowship exam. He is also actively involved in running continuing dental education courses including implant trainings for dentists. Dr. Termei has served as former director and president of the Iranian Ontario Dental Association (IODA). He has also led several outreach dental mission trips to outreach communities abroad.












