Abstract
Temporomandibular disorders (TMD) are a broad term for pain and/or dysfunction in the masticatory musculature, temporomandibular joint (TMJ), and associated structures. Limitations in jaw mobility sound arising from the TMJ and orofacial pain are common reasons patients may seek dental care. While symptoms of TMD may be common, the pathophysiology of this condition is multifactorial and can contain a biopsychological component without any pathognomonic factors. Furthermore, different predisposing, initiating and perpetuating factors complicate correctly diagnosing this condition. While the mortality of TMD is negligible, its impact on the quality of life is unmeasurable. Intervention at an early stage of TMD can help mitigate patient symptoms and potential exacerbation into a chronic phase. Therefore, dental practitioners must be able to recognize, diagnose and adequately manage patients with TMD. Furthermore, current best evidence supports using conservative first-line therapies to manage most TMD cases. This article aims to report up-to-date recommendations/understanding in the aetiology, diagnosis and management of TMD.
Temporomandibular disorder is a broad term characterized by craniofacial pain involving the head and neck joint, masticatory muscles, or muscle innervations.1,2 TMD is the most common non-odontogenic orofacial pain, with anywhere from 15-30% of the population presenting with some form of TMD.3,4 The lack of consensus on the actual prevalence of TMD stems from the heterogeneity in the diagnostic criteria used by systematic reviews in the past. Regardless, the pain associated with TMD motivates close to 7% of the population to seek treatment annually.5 The incidence of TMD varies concerning age and sex. However, incidence spikes from 20 to 40 and is twice more common in women.6 As mentioned, TMD describes a collection of disorders. Hence, management strategies vary significantly concerning the subtype of TMD. Management of these conditions can be challenging and often result in a multidisciplinary approach when first-line conservative treatment modalities fail.7 Therefore, it is imperative that dental professionals recognize risk factors, correctly diagnose, and understand what treatments are adequate for their patients to arrest or delay the progression of this disease.
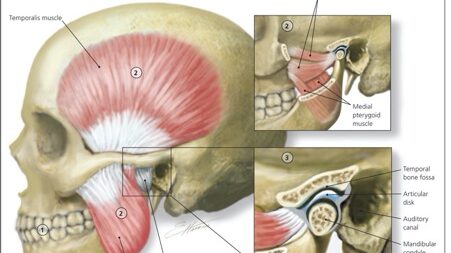
Fig. 1

Anatomy
The TMJs forms via the bony articulation of the condylar process of the mandible and the glenoid fossa/articular eminence of the squamous part of the temporal bone.9 The osseous structures in articulation are lined by fibrocartilage and separated via an articulating disc. This creates two joint cavities lined by synovial fluid, a substance similarly found in ball and socket joints. In addition, synovial membranes outline the two joint cavities outlined by the articulating disc and its corresponding bony counterpart. This unique anatomy creates a ginglymoarthroidal joint (hinge and translation movements).10 The muscles of mastication facilitate joint function: the temporalis, masseter, and medial pterygoid muscles are adductors, while the lateral pterygoid muscles are the primary abductors of the mandible. However, the bony endpoints, extrinsic and intrinsic ligaments, and the occlusal relationship between maxillary and mandibular dentition limit the TMJ function.9 Sensory innervation to the TMJ arrives from the auriculotemporal and masseteric nerves splitting from the mandibular branch of the trigeminal nerve. At the same time, motor innervation also arises from the mandibular branch of the trigeminal nerve. The arterial blood supply is facilitated by the superficial temporal artery branching of the external carotid, while the venous drainage is through the venous plexus surrounding the capsule.11 These joint functions via the bilateral coordination of the two TMJs connected via a single bone(mandible). Therefore, the two joints cannot function independently of each other. Furthermore, the articular disc creates two separate joint cavities within the joint capsule. Since the two TMJs functions are tied together, it can be considered four joints operating as a single unit.
Fig. 2

Aetiology/Pathophysiology/Risk Factors
It is well known that symptomatic TMD has a complex aetiology where a singular cause is unlikely to be identified for a patient. Similarly, other chronic pain disorders (low back pain, migraines) with complex aetiologies have adopted a biopsychological model.12 This model aids in understanding, diagnosing, and ultimately managing chronic pain, such as in TMD.13 This model comprises biological, psychological and social domains where an issue in one domain affects the other two domains.13 This cause-and-effect relationship is derived from the fact that each of the domains comprises a variety of risk factors that can interact with the other domains.14 Such risk factors comprise predisposing, initiating and perpetuating factors related to the development of TMD. Many comorbid conditions like fibromyalgia, depression, and irritable bowel syndrome are examples of predisposing factors.15 Initiating factors, on the other hand, may cause a TMD (jaw injury, migraine).16 Lastly, perpetuating factors will sustain a TMD once established (increase in comorbid conditions, changes to masticatory patterns).17
Examples of macro-trauma range from significant head and neck trauma to lengthy dental procedures. Aggressive surgical removal of third molars and inadvertent inferior alveolar nerve blocks into the medial pterygoid are also considered macro-trauma risk factors. Micro-trauma, on the other hand, includes parafunctional habits like a nail, cheek, and lip biting, posturing a class 2 malocclusion into a class 1 or bruxism.18 While bruxism is a vital risk factor for TMD, it should be noted that the two can exist independently.19 For the development of TMD, trauma is an important factor, as it can be both a predisposing and initiating factor.
TMD is linked with other chronic pain conditions. Conditions ranging from fibromyalgia, irritable bowel syndrome, lower back pain, migraine, chronic regional pain syndrome, chronic fatigue syndrome, tension-type headache, chronic pelvic pain, post-surgical and other neuropathic pain have all been linked to TMD.18,20,21 Furthermore, comorbid conditions can alter the TMJ’s shape and lead to disruption of normal joint function and result in a TMD. Examples of these diseases include arthritis, juvenile idiopathic arthritis, psoriatic arthritis, systemic lupus erythematosus, osteoarthritis and neoplasia, scleroderma, Lyme’s disease, ankylosing spondylitis and idiopathic condylar resorption.22-24
Psychological conditions have been shown to have an enormous impact on the potential development of a TMD. Appropriate history taking for post-traumatic stress disorder, depression, and anxiety should all be noted as they can modify pain perception and complicate the management of TMD.25,26 Stress is both an initiating and perpetuating factor, as persistent stress can develop muscle tension due to clenching, prompting a potential TMD. Clenching and bruxing in excess, nocturnal and diurnal clenching can cause TMD pain and other symptoms like headaches. These symptoms often manifest as attrition and wear facets; however, this alone should not be used as a diagnostic tool.
While the exact pathophysiology of TMD is inconclusive, various pathways have been studied to explain how biological, psychological and social domains can interact to cause TMD. Genetic, endocrine and inflammatory pathways have been studied to highlight common biomarkers seen in patients with TMD potentially.27,28 Several genes (SCN1A, ACE2, PTGS1, APP, MPDZ) have been linked to TMD concerning their role in altered pain perceptions. Catecholamine-O-methyltransferase (COMT) is a common enzyme responsible for regulating endocrine pathways involved with epinephrine, norepinephrine and dopamine. Reduced COMT activity can leave these hormones unregulated and lead to painful TMD symptoms.29 Lastly, both an increase in pro-inflammatory(MCP-1)and a reduction in anti-inflammatory(Omectin-1) mediators have been shown to play a substantial role in TMD.30,31
It is clear that TMD does not follow a simple biological or physical aetiology; instead, it is the incorporation of biological, psychological, and social factors that interact together. Therefore, it is crucial to take a complete medical history and thorough exam to determine how these factors may contribute to a potential TMD, but more importantly, come to a formal diagnosis and appropriate treatment plan.
Fig. 3

Signs/Symptoms and Classification
Clinicians’ ability to recognize common signs, as well as their ability to interpret patient symptoms, are an important tools in correctly diagnosing and managing TMD. While signs and symptoms of TMD can vary based on the patient and subtype of TMD, Table 1 references a few common features dentists should be aware of. Pain is one of the most common symptoms; however, it also has an extremely variable presentation.32 Pain can present in the muscles of mastication, TMJs, or both, with intensities ranging from mild to severe and frequency of episodes ranging from a few a day to a few a month.5 Following pain, limitation in jaw movement and joint noises are the frequently reported symptoms of TMD. The second most reported symptom is a restriction of jaw movement. Interincisal opening less than 40mm is commonly caused by muscle hypertrophy of strain; however, disc displacement can also limit the patients’ opening. When the latter is the cause of the restriction of movement, the deviation can also be noticed on opening.33 Joint sounds can occur during opening, closing or both and usually indicate articular disc displacement. The timing of the noise can also correlate to the severity of the TMD; the earlier the joint noise is in motion generally signifies a more mild version of the disease.34 However, clicking related to disk displacement does not necessarily signify TMD. A large-scale study showed up to 25% of patients had clicking in their TMJ without any associated pain.35 As shown in Table 1, the signs and symptoms of TMD are variable. Furthermore, there are other less common symptoms that dentists should be aware of during a patient’s exam, such as sleep disturbances, tinnitus, a reduction is hearing, sharp pain in ear(s), paresthesia/swelling of the face, pain on swallowing, and retro-orbital pain.3,8,32,36
Table 1: Common Sign and Symptoms of TMD.
| Signs | Symptoms |
| Tender muscles of mastication | Facial pain |
| Limited opening or deviated opening | Limited range in jaw movement |
| Crepitus/clicking | Joint sounds |
| Masseteric hypertrophy | Headache |
| Tenderness over TMJ | Pre-auricular pain |
| General dental sensitivity to percussion | Difficulty eating |
| Clenching/Bruxing | Clenching/Bruxism |
The classification of TMD can be complicated as many of the subclasses of TMD have variable overlaps, and patients may present with multiple forms of TMD. Regardless, from a taxonomic perspective, the main branches of TMD are temporomandibular joint disorders, masticatory muscle disorders, and headaches attributed to TMD. There are many subtypes of TMD; however, for this article, the emphasis will be placed on the twelve most common TMD, including myalgia, myofascial pain, local myalgia, myofascial pain with referral, arthralgia, headache attributed to TMD, degenerative joint disease, subluxation, and the four-disc displacement disorders.8,37,38
Diagnosis
The criteria needed to reach a reliable TMD diagnosis have changed as researchers gain more insight into the disease and run various reliability and validity testing. Previous TMD diagnoses relied on the Helkimo Index, which was then improved to create the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD).13,39 After further validation/reliability studies and the addition of further subclassifications of TMD, a new and improved Diagnostic Criteria for Temporomandibular Disorders(DC/TMD) was created.37,40 The DC/TMD is a comprehensive tool for researchers and clinicians to communicate TMD’s nuances properly. This tool provides a methodical approach to appropriately examine patients on a physical level (Axis 1) and for psychosocial/comorbid factors (Axis 2). When a patient presents to your office complaining of pain involving the TMJ or you suspect some form of TMD, appropriate steps should be taken to manage them. A TMD screening tool should first be used as a quick assessment to determine if further investigation is needed. If confirmed, a complete history should be taken, followed by a structured physical evaluation.
There are various TMD screening tools available for use in practice, most of which are questionnaires which can be carried out quickly by various dental team members.41-43 However, the DC/TMD recommends using the TMD Pain Screener (Table 2), which has been shown to have a 99% sensitivity and 98% specificity rating.36,44 These questionnaires aim not to reach a definitive diagnosis but to determine if further investigation is needed. With respect to Table 2, the scoring should be as follows: ‘a’ responses = 0 points; ‘b’ responses = 1 point; ‘c’ response = 2 point. A total score of 2 or more suggests further investigation for a potential TMD is needed.
Table 2: TMD Pain Screener.
| Question | Response | |
| 1 | In the last 30 days, on average, how long did you have any pain in your jaw or temple area on either side last? | (a)No Pain (b)From very brief to more than a week, but it does stop (c)Continuous |
| 2 | In the last 30 days, have you had pain or stiffness in your jaw on awakening? | (a) No (b) Yes |
| 3 | In the last 30 days, did the following activities change any pain (that is, make it better or make it worse) in your jaw or temple area on either side? Chewing hard or tough food Opening your mouth or moving your jaw forward or to the side Jaw habits (i.e clenching, grinding, chewing gum) Other activities (i.e talking, kissing or yawning) | (a) No (b) Yes |
If the TMD pain screener finds further assessment is needed, a thorough history should be taken concerning their potential TMD. A complete medical workup should be conducted to rule out any other chronic pain/facial pain diagnoses contributing to the TMJ pain. Furthermore, recent stressful or anxious events could be an initiating or perpetuating factor that should be investigated during the history-taking process. This part of the exam is essential, and enough time should be given to get to know the patient and get an accurate history. An appropriate history leads to a precise diagnosis and favourable management for the patient. Table 3 shows a list of questions that can be asked about a person’s medical record based on the common symptoms of TMD. The follow-up questions can give insight into the history of pain and potentially guide management. For example, if a patient has a parafunctional habit, this contributing factor should be optimally eliminated before administering more aggressive treatment options.
Table 3: Potential Follow-Up Questions Based on Presentation
| Finding | Follow up questions | |
| Pain | Were there any triggers when the pain first started? (What do you think triggered the pain?) History of trauma? (To elicit Macro-trauma (e.g. physical injury) versus micro-trauma (e.g. parafunction such as gum chewing) Describe the pain in your own words When did the pain first start? Is the pain there all the time? Is the pain episodic or continuous? If there are episodes, how often do the episodes last? If there episodes, how frequently do they occur? Is there a pattern to when the pain occurs? (i.e., every morning, during the day) Can you rate the pain on a scale of 0-10? How is the pain NOW? when it’s very bad, and when it’s manageable? What causes the pain to start? What makes the pain worse? What makes the pain better? Can you point to the area of pain? | |
| Joint Noises | Do you have any joint noises? Do you have an earache or ear noises? Did the noises appear after a traumatic event?- | |
| Limited Jaw movement | Do you have headaches? If so, duration, timing, location and frequency of headaches. Do you avoid any foods because of facial pain? Locking – does it occur after a joint noise? How often does it occur How long does it take to ease and what eases it? Can the jaw be manipulated open/closed? | |
| Headache | Do you have headaches? If so, duration, timing, location and frequency of headaches. | |
| Parafunctional Habits | Are you aware of tooth grinding, clenching, chewing gum, chewing pens or nail biting? Is this during the day or night or both? | |
| Other | Have you lost weight because of the pain? Do you have trouble sleeping? Do you have airway problems or sleep apnea? Have you been experiencing significant stress or anxiety recently? Do you have or have you ever had any chronic pain conditions in the past (chronic low back pain, Migraines, Fibromyalgia) Previous treatment for facial pain? |
Physical Assessment: Axis 1
After getting a complete history, a physical assessment should be completed to use the DC/TMD to reach a diagnosis. It is essential to understand that there is much overlap in physical symptoms. Furthermore, diagnoses are not mutually exclusive in the DC/TMD. There are numerous tools available for physically assessing TMD patients. However, a few critical aspects should be investigated during the assessment.32,45,46 Table 3 provides an example circuit to evaluate your patients. It highlights the vital regions that should be examined during a TMD assessment. Palpation of the TMJ, the surrounding area, and muscles of mastication are important for Axis 1 of the DC/TMD to arrive at a diagnosis. General appearance assessments like facial asymmetries could imply an alteration in condylar anatomy, while hypertrophic muscle of mastication could indicate some parafunctional habit.
Furthermore, an intra-oral exam should be completed to investigate parafunction further or rule out odontogenic origins of pain. Axis 2 of the DC/TMD is a combination of various questionnaires for psychosocial assessment. It is complex and not intended for use by the general practitioner but by researchers/clinical specialists to gain insight into any potential contribution of a psychosocial component to the aetiology of the patient’s TMD.37
Table 4: Checklist for Physical Examination
| Location | Yes/N | Pain | Familiar Pain | Measurement | Joint Sound | Details |
| General Appearance | ||||||
| Facial asymmetry | R/L | |||||
| Muscular hypertrophy | R/L | |||||
| Jaw posturing | R/L | |||||
| Nail Biting | R/L | |||||
| Mandibular movements | ||||||
| Deviation | R/L | |||||
| Deflection | R/L | |||||
| Max opening with pain | R/L | |||||
| Max opening without pain | R/L | |||||
| Max assisted opening | R/L | |||||
| Right lateral excursion | R/L | |||||
| Left lateral excursion | R/L | |||||
| TMJ | ||||||
| Open palpation | R/L | |||||
| Closed palpation | R/L | |||||
| Peri-oral region palpation | R/L | |||||
| Muscles of Mastication | R/L | |||||
| Temporalis | R/L | |||||
| Masseter | R/L | |||||
| Lateral Pterygoid | R/L | |||||
| Intra-oral | ||||||
| Attrition, wear facets, fractured teeth or restorations | R/L | |||||
| Reduced VDO | R/L | |||||
| Loss of posterior support | R/L | |||||
| Linea alba/scalloping of lateral boarder of tongue | R/L |
Oral Health welcomes this original article.
References
- Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008 Dec 18;359(25):2693-705.
- Reny de Leeuw, Gary D. Klasser. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management. 2018.
- Kapos F p., Exposto F g., Oyarzo J f., Durham J. Temporomandibular disorders: a review of current concepts in aetiology, diagnosis and management. Oral Surg. 2020;13(4):321-34.
- Valesan LF, Da-Cas CD, Réus JC, Denardin ACS, Garanhani RR, Bonotto D, et al. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig. 2021 Feb;25(2):441-53.
- Velly AM, Anderson GC, Look JO, Riley JL, Rindal DB, Johnson K, et al. Management of painful temporomandibular disorders: Methods and overview of The National Dental Practice-Based Research Network prospective cohort study. J Am Dent Assoc 1939. 2022 Feb;153(2):144-57.
- Maixner W, Diatchenko L, Dubner R, Fillingim RB, Greenspan JD, Knott C, et al. Orofacial pain prospective evaluation and risk assessment study—the OPPERA study. J Pain. 2011 Nov;12(11 Suppl):T4-11.e1-2.
- Ahmad M, Schiffman EL. Temporomandibular Joint Disorders and Orofacial Pain. Dent Clin North Am. 2016 Jan 1;60(1):105-24.
- Gauer RL, Semidey MJ. Diagnosis and Treatment of Temporomandibular Disorders. Am Fam Physician. 2015 Mar 15;91(6):378-86.
- Hatcher DC. Anatomy of the Mandible, Temporomandibular Joint, and Dentition. Neuroimaging Clin N Am. 2022 Nov;32(4):749-61.
- Tamimi D, Jalali E, Hatcher D. Temporomandibular Joint Imaging. Radiol Clin North Am. 2018 Jan;56(1):157-75.
- Piette E. Anatomy of the human temporomandibular joint. An updated comprehensive review. Acta Stomatol Belg. 1993 Jun;90(2):103-27.
- Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977 Apr 8;196(4286):129-36.
- Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord Facial Oral Pain. 1992;6(4):301-55.
- Bair E, Gaynor S, Slade GD, Ohrbach R, Fillingim RB, Greenspan JD, et al. Identification of clusters of individuals relevant to temporomandibular disorders and other chronic pain conditions: the OPPERA study. Pain. 2016 Jun;157(6):1266-78.
- Bonato LL, Quinelato V, De Felipe Cordeiro PC, De Sousa EB, Tesch R, Casado PL. Association between temporomandibular disorders and pain in other regions of the body. J Oral Rehabil. 2017 Jan;44(1):9-15.
- Sharma S, Wactawski-Wende J, LaMonte MJ, Zhao J, Slade GD, Bair E, et al. Incident injury is strongly associated with subsequent incident temporomandibular disorder: results from the OPPERA study. Pain. 2019 Jul;160(7):1551-61.
- Meloto CB, Slade GD, Lichtenwalter RN, Bair E, Rathnayaka N, Diatchenko L, et al. Clinical predictors of persistent temporomandibular disorder in people with first-onset temporomandibular disorder: A prospective case-control study. J Am Dent Assoc 1939. 2019 Jul;150(7):572-581.e10.
- Wu J, Huang Z, Chen Y, Chen Y, Pan Z, Gu Y. Temporomandibular disorders among medical students in China: prevalence, biological and psychological risk factors. BMC Oral Health. 2021 Oct 26;21(1):549.
- Manfredini D, Lobbezoo F. Sleep bruxism and temporomandibular disorders: A scoping review of the literature. J Dent. 2021 Aug;111:103711.
- Furquim BD, Flamengui LMSP, Conti PCR. TMD and chronic pain: a current view. Dent Press J Orthod. 2015;20(1):127-33.
- Golanska P, Saczuk K, Domarecka M, Kuć J, Lukomska-Szymanska M. Temporomandibular Myofascial Pain Syndrome-Aetiology and Biopsychosocial Modulation. A Narrative Review. Int J Environ Res Public Health. 2021 Jul 23;18(15):7807.
- Mercuri LG. Osteoarthritis, osteoarthrosis, and idiopathic condylar resorption. Oral Maxillofac Surg Clin N Am. 2008 May;20(2):169-83, v-vi.
- Bradshaw BT, Jones KM, Westerdale-McInnis JM, Gaff HD. Orofacial Manifestations of Lyme Disease: A systematic review. J Dent Hyg JDH. 2021 Aug;95(4):23-31.
- Pellicano C, Leodori G, Floridia S, Colalillo A, Gigante A, Rosato E, et al. Reciprocal effects of scleroderma and temporomandibular dysfunction between patient cohorts. Cranio J Craniomandib Pract. 2021 Dec 28;1-8.
- Sójka A, Stelcer B, Roy M, Mojs E, Pryliński M. Is there a relationship between psychological factors and TMD? Brain Behav. 2019 Sep;9(9):e01360.
- Fisher E, Law E, Dudeney J, Palermo TM, Stewart G, Eccleston C. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2018 Sep 29;9(9):CD003968.
- Smith SB, Mir E, Bair E, Slade GD, Dubner R, Fillingim RB, et al. Genetic variants associated with development of TMD and its intermediate phenotypes: the genetic architecture of TMD in the OPPERA prospective cohort study. J Pain. 2013 Dec;14(12 Suppl):T91-101.e1-3.
- Shrivastava M, Battaglino R, Ye L. A comprehensive review on biomarkers associated with painful temporomandibular disorders. Int J Oral Sci. 2021 Jul 29;13(1):23.
- Brancher JA, Bertoli FM de P, Michels B, Lopes-Faturri A, Pizzatto E, Losso EM, et al. Is catechol-O-methyltransferase gene associated with temporomandibular disorders? A systematic review and meta-analysis. Int J Paediatr Dent. 2021 Jan;31(1):152-63.
- Jayaseelan VP, Arumugam P. A Computational Data Mining Strategy to Identify the Common Genetic Markers of Temporomandibular Joint Disorders and Osteoarthritis. Glob Med Genet. 2022 Jun;9(2):159-65.
- Harmon JB, Sanders AE, Wilder RS, Essick GK, Slade GD, Hartung JE, et al. Circulating Omentin-1 and Chronic Painful Temporomandibular Disorders. J Oral Facial Pain Headache. 2016;30(3):203-9.
- Shah A, Naqvi A. Temporomandibular disorder: A guide for general dental practitioners. Prim Dent J. 2022 Sep;11(3):118-25.
- Maini K, Dua A. Temporomandibular Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 Dec 27]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK551612/
- Poluha RL, De la Torre Canales G, Bonjardim LR, Conti PCR. Clinical variables associated with the presence of articular pain in patients with temporomandibular joint clicking. Clin Oral Investig. 2021 Jun;25(6):3633-40.
- Dworkin SF, Huggins KH, LeResche L, Von Korff M, Howard J, Truelove E, et al. Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls. J Am Dent Assoc 1939. 1990 Mar;120(3):273-81.
- Beaumont S, Garg K, Gokhale A, Heaphy N. Temporomandibular Disorder: a practical guide for dental practitioners in diagnosis and management. Aust Dent J. 2020;65(3):172-80.
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28(1):6-27.
- Peck CC, Goulet JP, Lobbezoo F, Schiffman EL, Alstergren P, Anderson GC, et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J Oral Rehabil. 2014 Jan;41(1):2-23.
- Helkimo M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven Tandlakare Tidskr Swed Dent J. 1974 Mar;67(2):101-21.
- Yap AU, Zhang MJ, Zhang XH, Cao Y, Fu KY. Viability of the quintessential 5 temporomandibular disorder symptoms as a TMD screener. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022 Jun 1;133(6):643-9.
- Borges REA, Mendonça L da RA, dos Santos Calderon P. Diagnostic and screening inventories for temporomandibular disorders: A systematic review. CRANIO®. 2021 Jul 18;0(0):1-7.
About the Author

Rickson Valtellini holds a Bachelor of Engineering and is a fourth-year dental student at the University of Toronto faculty of dentistry.

Aviv Ouanounou is an associate professor of Pharmacology & Preventive Dentistry at the Faculty of Dentistry, University of Toronto, and a clinical instructor and Treatment Plan Coordinator in the university clinics. He is the recipient of the 2014-2015 Dr. Bruce Hord Master Teacher Award for excellence in teaching and the 2018-2019 National W.W. Wood Teaching Award for Excellence in Dental Education. He is a Fellow of the International College of Dentists, American College of Dentists and Pierre Fouchard Academy. Dr. Ouanounou maintains a private practice in Toronto and is the corresponding author for this article. Reach him at aviv.ouanounou@dentistry.utoronto.ca









