Abstract
Third molar removal complication rates can be as high as 30%. Risk assessment tools may lower these rates. Artificial intelligence (AI) driven prediction models are a promising approach to predict possible unfavorable outcomes and cone-beam computed tomography imaging may play an important role. AI prediction models are showing excellent results in research settings. To be implemented in clinical practice they will need to overcome some robustness, security, liability, and practical issues. If they do, AI prediction models can be integrated in electronic patient record systems by alerting clinicians in case of an imminent unfavorable outcome so it can be avoided.
Clinical Relevance
Artificial intelligence driven risk assessment tools will lower complications in third molar surgery.
Objective
After reading, you will comprehend commonly used AI terminology, the current and future use of AI and machine learning applications in third molar surgery and possible obstacles for its implementation.
Safety is of paramount importance in our rapidly evolving healthcare system. Numerous medical risks occur every day, and to mitigate them, risk assessment strategies are increasingly being used.1 Several risks may arise during third molar removal, one of the most commonly performed dentoalveolar surgical procedures.2 These can be found in the areas before, during, and after surgery and may involve trigeminal nerve injuries, prolonged postoperative pain, infection, hemorrhage, oroantral communications and fractures. To mitigate these risks and avoid unfavorable outcomes, a probability assessment of the likelihood of occurrence is crucial. Advanced statistical models are used for this and with the rise of artificial intelligence (AI), powerful prediction tools are becoming available for clinical care. Ideally, risk assessment is performed automatically based on electronically registered patient data and is integrated in a warning system that alerts the clinician when a high probability of an unfavorable outcome is present. This allows the clinician to act appropriately.
A great example are the automatic early warning scores for hospitalized patients , allowing doctors to detect deterioration of their patients in realtime.3 Based on certain patient parameters that are registered in the hospital such as blood pressure, respiratory rate and heart rate, the electronic health record system calculates such an early warning score and prompts the nurse to contact the treating physician when a high score is registered on the system. These types of systems are being developed in different branches of healthcare and are a clear example of the integration of data science in clinical practice. The current paper will discuss the importance of risk assessment in third molar management, the role of AI systems and their integration into clinical practice.
Importance of Risk Assessment in Third Molar Surgery
The complication rate after wisdom tooth extractions varies but can be as high as 30%, according to some resulting in a high return of patients to the practitioner’s office after surgery.2 Vranckx et al reported a revisitation rate of 20% in a group of 6010 patients who had one or more wisdom teeth removed.4
Many authors have already tried to determine the degree of difficulty of a third molar extraction and therefore the risk associated with this procedure.4–9 The primary factors contributing to this are determined preoperatively, such as age, ethnicity, body mass index, gag reflex, and presence of anxiety. Dental factors such as crown and root morphology, horizontal and vertical position, bone density and proximity of the inferior alveolar nerve (IAN) also play an important role. The Pell and Gregory classification on depth of impaction and the Rood and Shehab classification on predicting IAN injury are the best known risk classification systems for injury to this nerve in relation to third molar surgery.10,11
The occurrence of IAN injury is one of the most feared complications. This occurs in about 2% of all third molar extractions but can vary greatly depending on the location of the wisdom tooth and increases with age.12 Once nerve damage has occurred it can be temporary or permanent with a significant impact on the patient’s quality of life.13 To prevent this nerve damage, a preoperative panoramic radiograph is classically used. Depending on the position of the wisdom tooth with respect to the mandibular canal, an additional conebeam computed tomography (CBCT) can be made. Until now, it could not be demonstrated that CBCT reduces the risk of IAN damage.14 However, we must realize that many studies had too little power and methodological bias to be able to draw this conclusion. Others have shown the relevance of CBCT in specific cases as it might change surgical management.15 Some guidelines on wisdom tooth extraction recommend CBCT in cases of overlap of the mandibular canal on panoramic imaging.16,17 Moreover, low radiation dose protocols of CBCT are continually improving.18,19 Thus, in light of the as low as diagnostically acceptable (ALADA) principle, a new discussion is possible about the use of three-dimensional CBCT which obviously contains more diagnostic information compared to a two-dimensional orthopantomogram (OPT).20 These developments are driving a relance in risk prediction research in which artificial intelligence (AI) and machine learning (ML) developments are playing an important role.
Artificial Intelligence and Machine Learning
AI, ML and deep learning (DL) research is growing abundantly. These terms are closely related but not interchangeable. AI is an umbrella term for automating intellectual tasks normally performed by humans. ML and DL are some of the tools to achieve this goal. Machine learning tries to represent a dataset by means of an algorithm. In conventional statistics this algorithm can easily be calculated, whereas in ML the algorithm is generated by training a subset of the data. The variables that are being used to train the model or algorithm are called features. The most commonly used AI terminology is explained in Table 1.
Table 1: Commonly used machine learning and artificial intelligence terminology.
| Machine learning term | Epidemiology term |
| Attribute, feature, predictor or field | Independent variable |
| Input and output | Independent (exposure) and dependent (outcome) variables |
| Classifier estimator | Model |
| Learner | Model fitting algorithm |
| Dimensionality | Number of explaining variables |
| Label | Value of dependent variables, outcomes |
| Imbalanced data | Data set which some cases or risk categories occur much less frequently than the others |
| Loss function | Error measure |
| Data munging or data wrangling | Data preparation |
To develop the best ML algorithm, we can use different teaching methods, such as guiding it with examples (supervised learning), letting it figure things out on its own (unsupervised learning), using a mix of both (semi supervised learning), or rewarding it for good decisions (reinforced method). In supervised models, the training data is labeled, meaning the features and outcome (target) are known. In unsupervised models the algorithm tries to detect patterns in the dataset without being informed on the target. Semi supervised learning combines both methods being that not all features have an associated target. This can be useful for very large datasets where labelling the whole dataset would be too time consuming. Finally, reinforcement learning focusses on improving a task by trial and error. Artificial neural networks and deep learning are ML methods mimicking biological neural networks. Several layers of nodes (resembling cell bodies) are connected (resembling dendrites and synapses). The nodes are then weighted against each other depending on their ability to provide the desired outcome.21
Current State of the Art
Risk prediction using ML techniques is possible both in the preoperative, perioperative and postoperative setting for patients having wisdom tooth surgery (Fig. 1).
Fig. 1
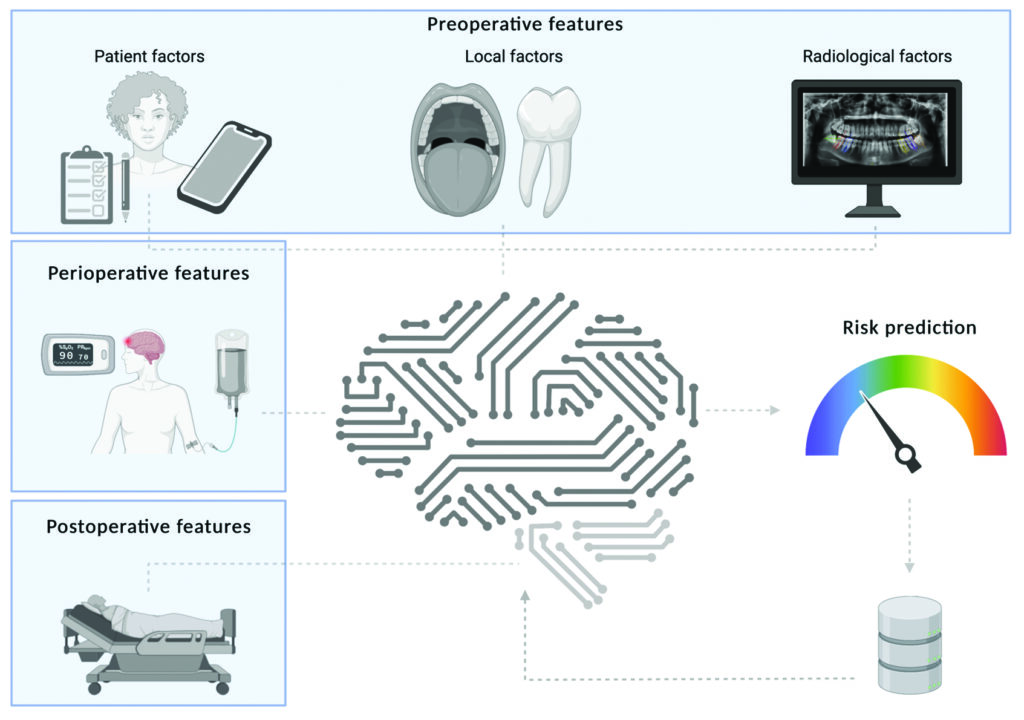
In the pre-surgery phase, our research group conducted a yet unpublished study using the same database by Vranckx et al.22 We were able to predict with 81% accuracy which patients would have severe pain after surgery. We used a “random forest” (a collection of decision-making trees) and the “Boruta algorithm” (a method to select the most important factors) to make these predictions. Also, unexpected significant predictive features were revealed using this method providing new insights in pain prediction. In a similar manner, Hur et al. calculated the risk factors for developing distal caries on the second molar associated with third molar impaction. A random forest model outperformed the other ML methods and showed the importance of the examined risk factors in developing these caries such as age, gender, location of contact point and Pell and Gregory classification.23
In the future, these models could be integrated into the electronic health record aiding the treating physician in consenting and informing the patient in advance and selecting the best management strategy.
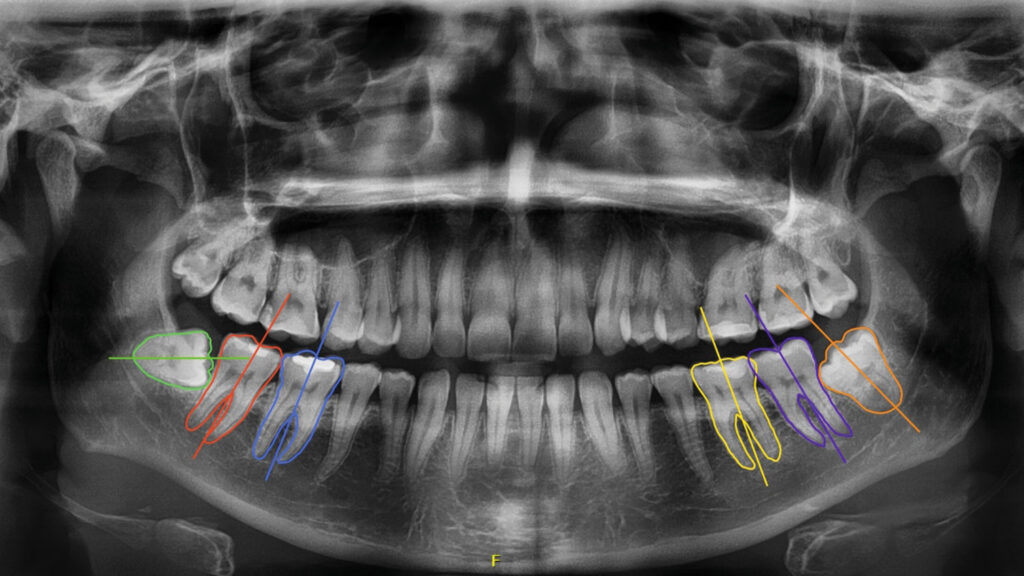
In our dental practices, we rely heavily on oral imaging, a field that will see many machine-learning developments in the next years. In Figures 2-5, we show some examples of radiological developments related to wisdom tooth surgery. In a first step, researchers succeeded in using a convolutional neural network (CNN) to automatically detect and segment the mandibular canal and the third molar on panoramic images.24,25 An important step in the further development of risk prediction models. A convolutional neural network is a type of computer program designed to process and recognize patterns, like images or sounds. It works similarly to how our brain recognizes things, by breaking down complex information into simpler parts and then combining them to understand the bigger picture. This makes CNNs particularly good at tasks like image recognition and analysis. Vranckx et al. used automatic segmentation and subsequent angulation measurements of mandibular molars to predict whether the third molar has a chance for functional eruption. Using a linear regression model, they found that an angle of more than 27° between the longitudinal axes of the third and second molar could accurately predict whether the wisdom tooth would erupt. Moreover, they showed that with increased angulation, the probability of a close relationship between the third molar and IAN increased significantly.26,27 Lee et al. trained a similar model to predict extraction difficulty and likelihood of IAN injury on panoramic radiographs with accuracies over 80%.28 Others used a similar approach to predict the Pederson difficulty score for extraction of third molars.29 Their CNN was able to accurately predict the ramus relationship, depth of impaction and angulation, and thus predict the final difficulty index.
Fig. 2
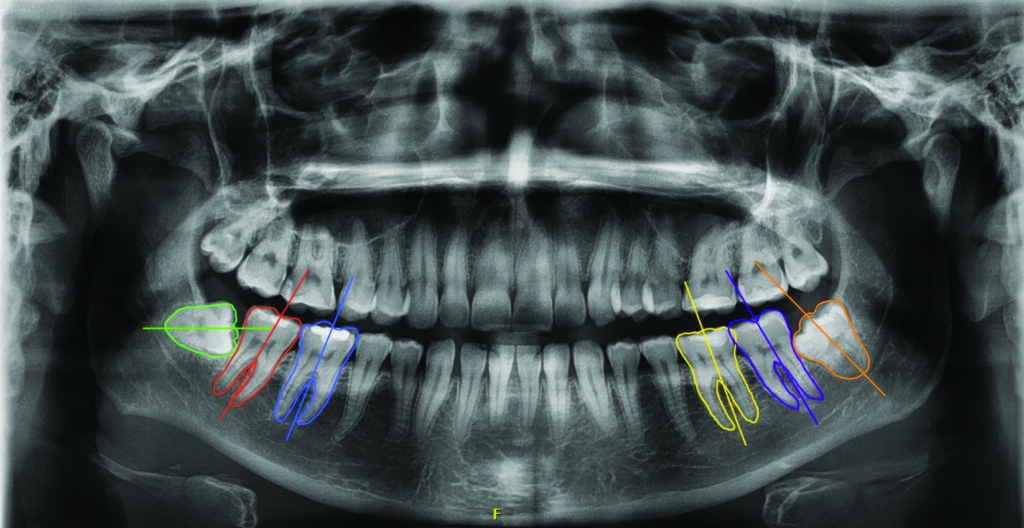
Fig. 3
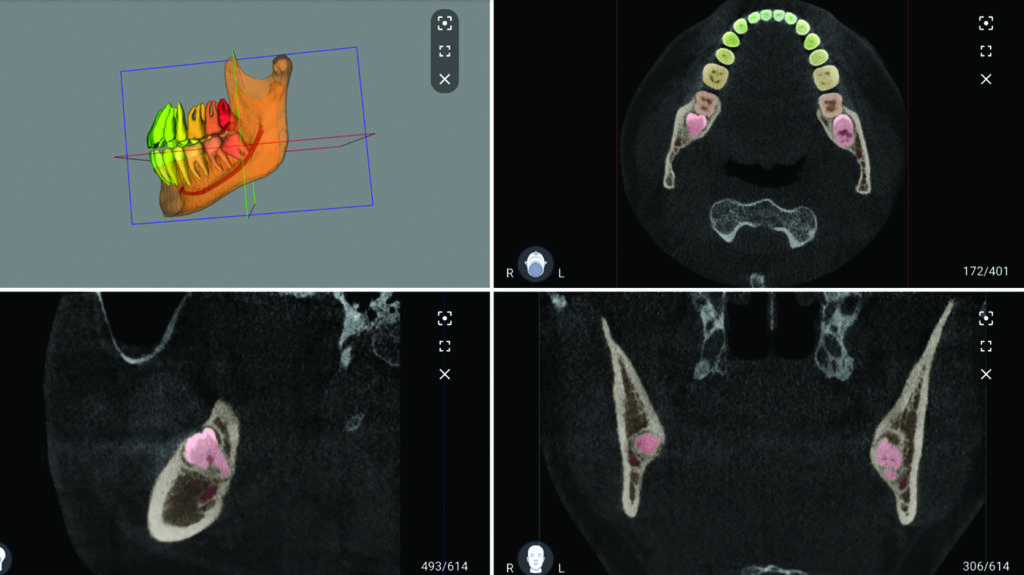
Fig. 4
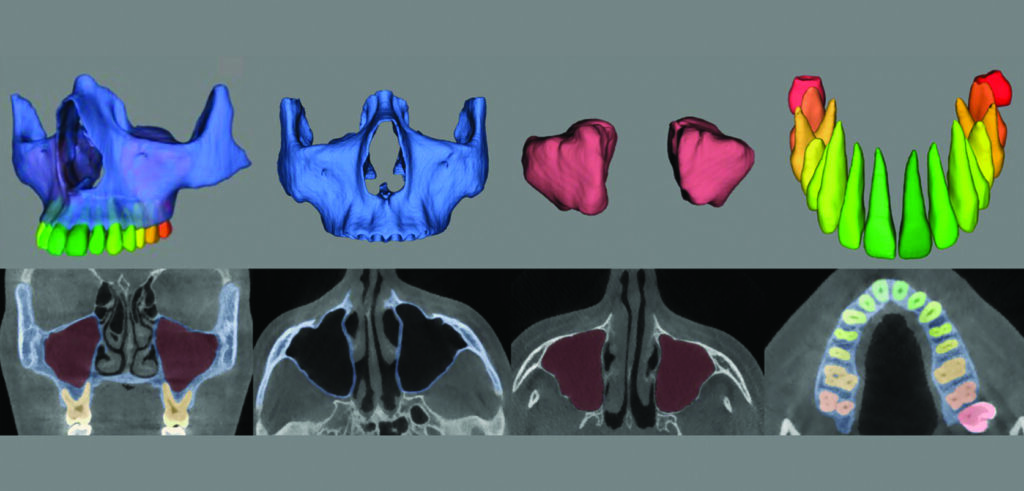
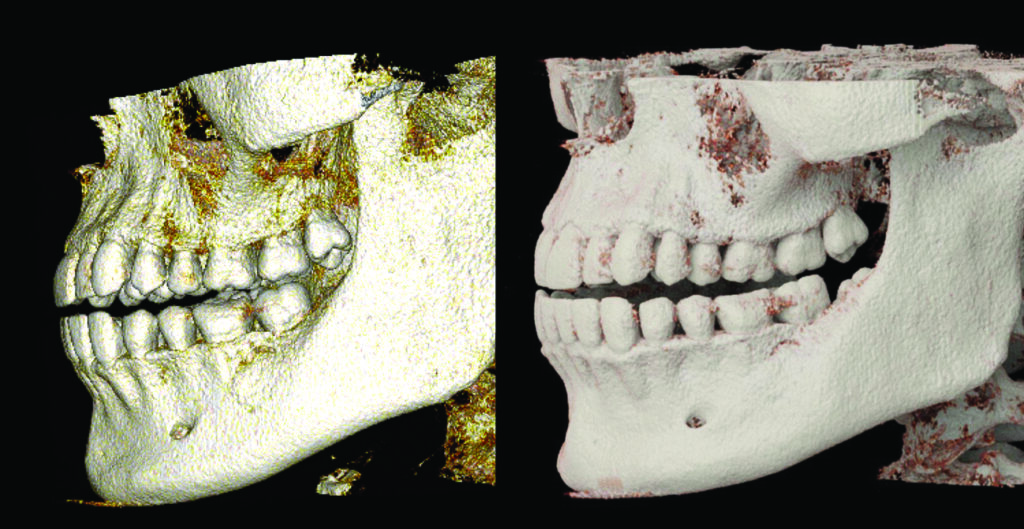
Fig. 5
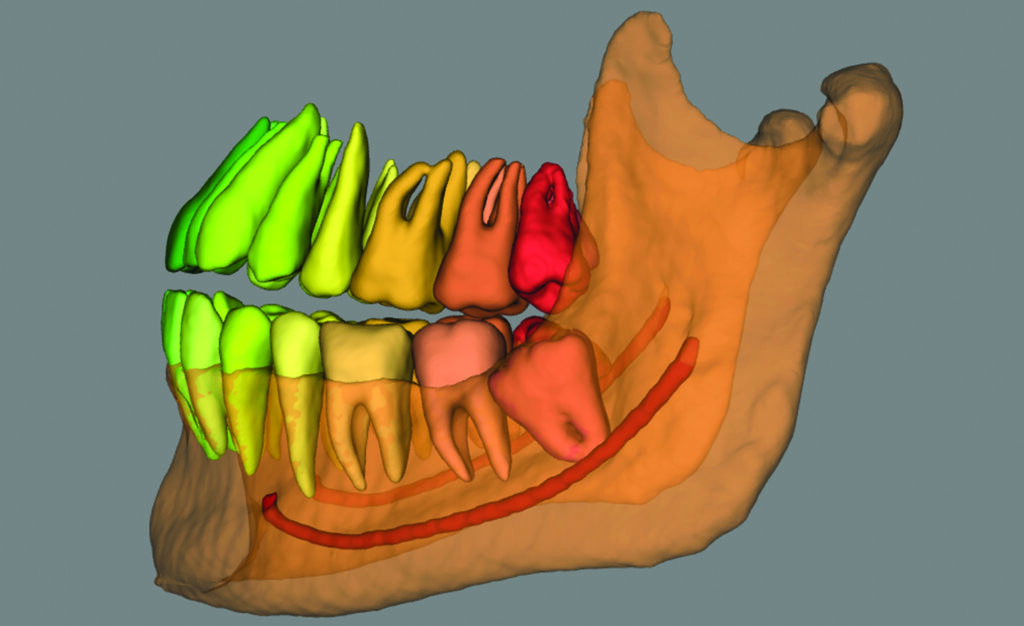
Subsequent developments by Choi et al., led to the use of CBCT and panoramic radiographs to train a learning algorithm to predict on a panoramic whether the IAN is located buccally or lingually from the mandibular canal and whether there was true contact between the two structures. This is important as a lingual position and close contact bear a greater risk for nerve damage when removing that third molar. Here, the algorithm was superior to the experienced radiologists with an accuracy to detect true contact of 72%. The question remains whether such accuracy is sufficient to estimate a potentially dangerous but infrequent risk.
These models could also be used to enhance preoperative visualization of important structures. Nogueira-Reis et al. created reliable virtual patient models from CBCT images using automatic segmentation in an average time of 1.7 minutes.30 Moreover, the platform allowed to select distinct anatomical structures such as the airway, teeth, maxillary sinuses enabling fast and accurate virtual surgical planning in the near future. However, it will remain difficult to demonstrate that these sophisticated visualization tools reduce the risk of complications in wisdom tooth surgery. Randomized studies in which the surgeon is offered only one type of imaging technique preoperatively to assess risk is often considered unethical. Moreover, large groups are needed to demonstrate a statistically significant difference on outcomes using different imaging modalities as the incidence of nerve injury is low. Finally, it is also difficult to demonstrate a behavioral change in surgeons the moment they are shown the preoperative imaging study. In other fields, however, it was recently demonstrated that true-to-life 3D cinematic rendered models are superior for detecting maxillofacial fractures compared to 2D CT images or volume rendered models (Fig. 6).31 A similar approach could be adopted to study the use of enhanced 3D models in preoperative surgical planning of wisdom tooth removal.
Fig. 6
Future Perspectives and Clinical Implementation
There is a clear exponential growth of AI applications in dentistry and medicine. It is evident that these applications will soon disrupt the way we work. However, there are some obstacles that need to be overcome before we can fully integrate these tools into our daily practice (Fig. 7).32
Fig. 7
First of all, we should ensure that these risk prediction tools are robust. Many of the already available tools are not validated on large populations and thus certain groups may be over- or underrepresented causing bias in the algorithm. This may lead to conclusions made by the algorithm that are not applicable to the desired population. To properly evaluate this, we require transparent AI systems that are ethically vetted. These systems emerge on big data and can become even more accurate with feedback from new dynamic real-world data in which the algorithm keeps improving by its daily application. For this, continuous feedback and monitoring systems need to be in place.
This leads us to our second obstacle, which is security and privacy. Data protection and privacy issues are at the forefront of all IT applications in healthcare nowadays. If these systems are used in practice and especially if a dynamic feedback model is used, patients and healthcare providers should be aware and consent on how this data is used and stored to improve a mostly commercial product. Furthermore, a robust security system is necessary to avoid data leaks in these mostly cloud-based products.
A third area of focus in implementing artificial intelligence in dental practices concerns how clinicians use these tools and their implications for liability. It is essential to understand that risk prediction models serve as a supportive tool, and like any other tool, they must be used correctly. These AI systems should assist clinicians in making decisions rather than automatically generating responses.
This highlights the importance of clinicians maintaining responsibility for the outcomes of decisions informed by AI systems. To ensure proper use and understanding of AI technologies, healthcare providers interacting with such systems should have at least a basic knowledge of their functions and underlying principles.
To facilitate this understanding, it is crucial to integrate AI technologies into dental and medical education programs. This will provide healthcare professionals with the necessary foundation to effectively utilize AI tools while ensuring they remain accountable for their decisions. Additionally, addressing ethical and legal concerns related to AI implementation will promote transparency and help safeguard patient interests.
Finally, after these robustness, security and liability issues are addressed a very practical problem becomes clear. Many of the risk assessment applications available today in third molar management are trained to solve very specific tasks requiring very specific input in a research setting. The transition to a clinical application poses a challenge as clinical reality is a bit messier. Clinicians have multiple questions: should I remove the third molar and if so, how big is the chance of nerve injury or a postoperative infection? This requires a combination of multiple AI models. Furthermore, these should be integrated in electronic patient record systems in a user-friendly way to make sure they are easily accessible.
Conclusion
The complication rates in third molar surgery promote the development and use of risk prediction systems to allow for adequate case selection, safe surgical planning, and individualized postoperative care. AI systems are rapidly propelling these prediction systems forward in very promising way. Due to technical improvements, declining radiation doses and a high diagnostic yield, CBCT imaging plays a crucial role in this process. Accurate risk prediction tools are already available in a research setting. The wide-spread adoption of these tools in clinical practice is on the horizon but needs to overcome robustness, security, liability and practical issues. 
Disclosure: Reprinted with permission from Dental Update. (Dent Update 2024; 51: 28–33)
Conflict of interest – copyright statement: The authors declare no conflict of interest. All figures and tables were created by the authors and we confirm we obtain the proper rights to publish the presented materials.
References
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ. 1998 Apr 11;316(7138):1154–7.
- Bouloux GF, Steed MB, Perciaccante VJ. Complications of Third Molar Surgery. Oral and Maxillofacial Surgery Clinics of North America. 2007 Feb;19(1):117–28.
- Gerry S, Bonnici T, Birks J, Kirtley S, Virdee PS, Watkinson PJ, et al. Early warning scores for detecting deterioration in adult hospital patients: systematic review and critical appraisal of methodology. BMJ. 2020 May 20;369:m1501.
- Vranckx M. Third molar management: eruption, removal and associated risks. [Leuven]: KU Leuven; 2020.
- Mercier P, Precious D. Risks and benefits of removal of impacted third molars. A critical review of the literature. Int J Oral Maxillofac Surg. 1992 Feb;21(1):17–27.
- Bruce RA, Frederickson GC, Small GS. Age of patients and morbidity associated with mandibular third molar surgery. J Am Dent Assoc. 1980 Aug;101(2):240–5.
- Phillips C, White RP, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg. 2003 Dec;61(12):1436–48.
- Renton T, Smeeton N, McGurk M. Factors predictive of difficulty of mandibular third molar surgery. Br Dent J. 2001 Jun 9;190(11):607–10.
- Gbotolorun OM, Arotiba GT, Ladeinde AL. Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction. J Oral Maxillofac Surg. 2007 Oct;65(10):1977–83.
- Pell G, Gregory G. Impacted mandibular third molars: classifications and modified technique for removal. Dent Digest. 1933;2:23–54.
- Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990 Feb;28(1):20–5.
- Vranckx M, Fieuws S, Jacobs R, Politis C. Prophylactic vs. symptomatic third molar removal: effects on patient postoperative morbidity. Journal of Evidence Based Dental Practice. 2021 Sep 1;21(3):101582.
- Van der Cruyssen F, Peeters F, Gill T, De Laat A, Jacobs R, Politis C, et al. Signs and symptoms, quality of life and psychosocial data in 1331 post-traumatic trigeminal neuropathy patients seen in two tertiary referral centres in two countries. Journal of Oral Rehabilitation. 2020;47(10):1212–21.
- Robbins J, Smalley KR, Ray P, Ali K. Does the addition of cone-beam CT to panoral imaging reduce inferior dental nerve injuries resulting from third molar surgery? A systematic review. BMC Oral Health. 2022 Nov 3;22(1):466.
- Korkmaz YT, Kayıpmaz S, Senel FC, Atasoy KT, Gumrukcu Z. Does additional cone beam computed tomography decrease the risk of inferior alveolar nerve injury in high-risk cases undergoing third molar surgery?Does CBCT decrease the risk of IAN injury? International Journal of Oral and Maxillofacial Surgery. 2017 May;46(5):628–35.
- Ghaeminia H, Burger M, Galjart M, Maertens J, van der Sleen J, Vissink A, et al. Richtlijn derde molaar. NVMKA. 2018.
- Royal College of Surgeons Faculty of Dental Surgery. Parameters of care for patients undergoing mandibular third molar surgery [Internet]. 2020. Available from: https://www.rcseng.ac.uk/-/media/files/rcs/fds/guidelines/3rd-molar-guidelines–april-2021.pdf
- Feragalli B, Rampado O, Abate C, Macrì M, Festa F, Stromei F, et al. Cone beam computed tomography for dental and maxillofacial imaging: technique improvement and low-dose protocols. Radiol med. 2017 Aug;122(8):581–8.
- Jacobs R. Dental cone beam ct and its justified use in oral health care. Journal of the Belgian Society of Radiology. 2011 May 4;94(5):254.
- Jaju PP, Jaju SP. Cone-beam computed tomography: Time to move from ALARA to ALADA. Imaging Sci Dent. 2015;45(4):263.
- Erickson BJ. Basic Artificial Intelligence Techniques. Radiologic Clinics of North America. 2021 Nov;59(6):933–40.
- Vranckx M, Fieuws S, Jacobs R, Politis C. Prophylactic vs. symptomatic third molar removal: effects on patient postoperative morbidity. Journal of Evidence Based Dental Practice. 2021 Sep;21(3):101582.
- Hur SH, Lee EY, Kim MK, Kim S, Kang JY, Lim JS. Machine learning to predict distal caries in mandibular second molars associated with impacted third molars. Sci Rep. 2021 Dec;11(1):15447.
- Liu MQ, Xu ZN, Mao WY, Li Y, Zhang XH, Bai HL, et al. Deep learning-based evaluation of the relationship between mandibular third molar and mandibular canal on CBCT. Clin Oral Invest. 2022 Jan;26(1):981–91.
- Ariji Y, Mori M, Fukuda M, Katsumata A, Ariji E. Automatic visualization of the mandibular canal in relation to an impacted mandibular third molar on panoramic radiographs using deep learning segmentation and transfer learning techniques. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2022 Jun;S2212440322010112.
- Vranckx M, Ockerman A, Coucke W, Claerhout E, Grommen B, Miclotte A, et al. Radiographic prediction of mandibular third molar eruption and mandibular canal involvement based on angulation. Orthod Craniofac Res. 2019 May;22(2):118–23.
- Vranckx M, Van Gerven A, Willems H, Vandemeulebroucke A, Ferreira Leite A, Politis C, et al. Artificial Intelligence (AI)-Driven Molar Angulation Measurements to Predict Third Molar Eruption on Panoramic Radiographs. Int J Environ Res Public Health. 2020 May 25;17(10):E3716.
- Lee J, Park J, Moon SY, Lee K. Automated Prediction of Extraction Difficulty and Inferior Alveolar Nerve Injury for Mandibular Third Molar Using a Deep Neural Network. Applied Sciences. 2022 Jan 4;12(1):475.
- Yoo JH, Yeom HG, Shin W, Yun JP, Lee JH, Jeong SH, et al. Deep learning based prediction of extraction difficulty for mandibular third molars. Sci Rep. 2021 Dec;11(1):1954.
- Nogueira-Reis F, Morgan N, Nomidis S, Van Gerven A, Oliveira-Santos N, Jacobs R, et al. Three-dimensional maxillary virtual patient creation by convolutional neural network-based segmentation on cone-beam computed tomography images. Clin Oral Invest [Internet]. 2022 Sep 17 [cited 2022 Nov 14]; Available from: https://link.springer.com/10.1007/s00784-022-04708-2
- Hu R, Zhang X y., Liu J, Wu J h., Wang R p., Zeng X c. Clinical application of cinematic rendering in maxillofacial fractures. International Journal of Oral and Maxillofacial Surgery. 2022 Dec;51(12):1562–9.
- Recht MP, Dewey M, Dreyer K, Langlotz C, Niessen W, Prainsack B, et al. Integrating artificial intelligence into the clinical practice of radiology: challenges and recommendations. Eur Radiol. 2020 Jun;30(6):3576–84.
About the Authors

Dr. Fréderic Van der Cruyssen Department of Oral & Maxillofacial Surgery, University Hospitals Leuven, Leuven, Belgium. Department of Imaging and Pathology, OMFS-IMPATH Research Group, Faculty of Medicine, University Leuven, Leuven, Belgium.

Dr. Pieter-Jan Verhelst Department of Oral & Maxillofacial Surgery, University Hospitals Leuven, Leuven, Belgium. Department of Imaging and Pathology, OMFS-IMPATH Research Group, Faculty of Medicine, University Leuven, Leuven, Belgium.

Dr. Reinhilde Jacobs Department of Imaging and Pathology, OMFS-IMPATH Research Group, Faculty of Medicine, University Leuven, Leuven, Belgium. Department of Oral Health Sciences, KU Leuven and Department of Dentistry, University Hospitals Leuven, Leuven, Belgium. Department of Dental Medicine, Karolinska Institutet, Stockholm, Sweden.