Periodontal disease is at an epidemic level. “Periodontal diseases and dental caries are the most prevalent chronic diseases, affecting children, adolescents, adults and the elderly.”1 Over seventy percent of Canadians have some form of periodontal disease. The statistics are similar in the United States. Gingivitis is present at all ages.2 Fifty percent to 94% of patients are experiencing some form of gingivitis, depending on clinical definition of gingivitis and the sample studied.3 According to a recent article in the New York Times, “More than 75% of American adults have some form of gum disease, but according to a major survey, only 60% have any significant knowledge”. The oral-systemic link, which has shown implications in diabetes, cardiovascular disease and now possibly stroke, is hard evidence for the importance of oral care.
Periodontal disease occurs with an initial inflammatory response to bacterial infection. This activates the innate immune system. Amplification of this initial localized response results in the release of an array of cytokines and other mediators and propagation of inflammation through the gingival tissues. The failure to encapsulate this “inflammatory front” within gingival tissue results in expansion of the response adjacent to alveolar bone. The inflammatory process then drives the destruction of connective tissue and alveolar bone that is the cardinal sign of periodontal disease.4
Periodontal disease is very cyclic (Figure 1). Periodontal disease occurs when the bacteria infect the biofilm, causing an inflammatory response from the gingival sulcus area. Once it is infected, inflammation increases. If unchecked, this inflammation will cause destruction to gingival tissues and surrounding bone structures, hence causing a periodontal pocket.5
Figure 1
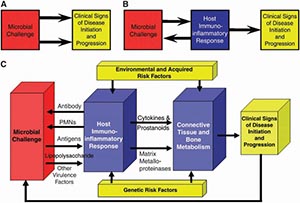
Periodontal Pathogenesis5
By not addressing the inflammatory response, it will continue to destroy tissue and bone. Normally, inflammatory responses to tissue will assist in healing the injured tissue. Periodontal disease represents a state of dysfunctional healing. The inflammatory response is not effective in resolving the lesion but actually perpetuating it.
Interestingly, we know that all inflammation is not always bad. It is a healthy bodily response. When we injure our knee or our back, we know that ice is necessary to reduce the swelling that occurs. If we don’t target the inflammation, future issues may arise. Using a similar thought process, treating the inflammation should be the primary target for periodontal disease.
So, what are we going to do about this? We need to target plaque and treat inflammation. Dental hygienists are truly the periodontal oral healthcare champions of our practice. They are on the front line of disseminating oral self-care instructions to our patients on a daily basis. Along with explaining the ravages of periodontal disease to our patients, they give fastidious oral hygiene instruction including brushing, flossing and rinsing. Rinsing should be an integral part of basic oral hygiene instructions.
Why rinsing? Rinsing is simple, fast and easy. Rinsing allows for a broad delivery system and can penetrate interdentally. Additionally, rinsing will deliver therapeutic agents, such as antiseptics, fluoride and anti-inflammatory agents) in a short period. The ideal rinsing product should have a combination effect of reducing bacterial load while delivering a therapeutic benefit to the tissue. The reduction of bacterial load should not be from the act of rinsing but the therapeutics in the rinsing liquid.
Several rinses are currently available.6 Essential oils disrupt cell wall viability to achieve antibacterial effects. Since the majority of these rinses contain alcohol, data is equivocal if effect is due to the actual essential oils or high alcohol content. An example in this category is Listerine, which contains eucalyptol, menthol, thymol, and methyl salicylate. Potential side effects include: tissue dryness and trauma from alcohol concentration. Some cell toxicity may also occur due to alcohol – a concern for surgical cases.
Delmopinol hydrochloride 0.2% is found in GUM PerioShield. It does not kill bacteria, but interferes with the synthesis of glucan. It reduces biofilm formation and interferes with bacterial adherence. Side effects include a significant taste alteration and staining (though less than chlorhexadine).
Chlorine dioxide, which is found in CloSYS, TheraBreath, Oxyfresh, and ProFresh (sodium chlorite), has an anti-bacterial effect that is combined with increased reduction of volatile sulfur compounds. The primary benefit of these products is fresh breath.
As far as the bactericidal rinses, chlorhexadine and cetylpyridinium chloride (i.e. Cepacol) utilize a cationic charge to bind anionic bacterial cell wall to achieve bactericidal effect. Both products have significant side effects but chlorhexadine is significantly worse. Chlorhexadine contains alcohol and will cause significant staining. Other side effects include altered taste, oral mucosal erosion, parotid gland swelling due to stenosis of the parotid and enhanced supergingival calculus formation.7 Chlorhexadine has overdose issues with children. Ingestion of 1-2 ounces of CHX by small child may lead to gastric distress including nausea or signs of alcohol intoxication. Chlorhexadine is also available alcohol free, though the staining and other issues remain.
There is a natural alternative. Utilizing plant botanicals to target inflammation and plaque, PeriActiveTM mouth rinse is a great alternative in this rinse category. Developed by Izun Pharmaceuticals Corporation Oral Care Division, there is a rinse utilizing natural bio-active compounds that exhibited powerful anti-inflammatory and wound-healing properties. PeriActiveTM contains three botanicals that work synergistically to reduce inflammation: Echinacea purpurea, Centella asiatica and Sambucus nigra. Echinacea purpurea and Centella asiatica reduce irritation and gingivitis. Sambucus nigra, in addition to reducing inflammation and gingivitis, is a gingival repair stimulator. These three products together promote healing (Table 1).
Table 1
PeriActiveTM is antibacterial, promotes tissue healing and has no alcohol. It is safe for daily use and causes no staining or drying of oral tissues. The bonus is the natural botanicals in the formulation. PeriActiveTM will block inflammation in several sites and induces fibroblasts to migrate, deposit matrix proteins, and secrete factors associated with healing. PeriActiveTM harnesses the polymolecular nature of plant extracts to block inflammation at multiple sites, which is a beneficial approach to controlling inflammatory damage. PeriActiveTM may also be utilized with the toothbrush, in lieu of toothpaste. Patients claim there is no “morning breath” if this product is used at night.
PeriActiveTM has been shown to actively reduce bacteria after two minutes (Figure 2). This is important in reigning in the active pathogens, such as P. gingivalis and A. viscosus, which are factors in periodontitis. Additionally, there has been evidence of decrease percentage in bleeding sites after using PeriActiveTM 12 (Figure 3). Finally, PeriActiveTM has shown to have similar antibacterial effect compared to Chlorhexadine, when utilized post implant surgery (Figure 4). Healing of the surgical site, two weeks post-operative, demonstrates healthy tissue without the use of alcohol or staining13,14 (Figures 5 & 6).
Figure 2

Strong anti-bacterial effect. PeriActiveTM reduction in bacteria.
Figure 3
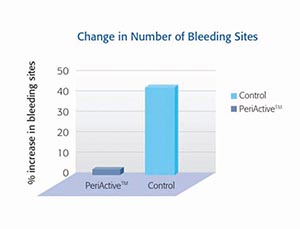
Change in Number of Bleeding Sites utilizing PeriActiveTM 11,12
Figure 4
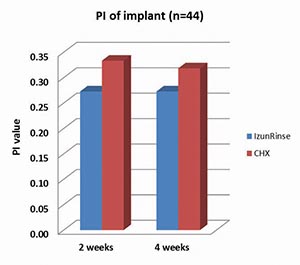
PeriActiveTM has similar antibacterial effect to chlorhexadine, post implant surgery13,14
Figure 5

Immediately post surgery.
Figure 6

PeriActiveTM rinse two weeks post surgical procedure used in conjunction with PerioPatchTM
We all struggle with compliance for our patient’s oral health maintenance. We aren’t able to be with our patients 24/7. We need to assist them with a solution to their inflammation and enlist them in stopping the cycle of their own periodontal disease. Along with brushing and flossing, using an anti-inflammatory rinse, these oral care regimens will assist our patients in keeping their teeth for a lifetime. For practitioners and patients who prefer a more natural approach to healthcare, without the staining and alcohol, PeriActiveTM is an excellent, bioactive choice. It prevents plaque, is antibacterial, reduces bleeding and inflammation, soothes the tissues with botanicals post operatively, while enhancing tissue repair.
References:
- Archived, Chronic Diseases in Canada
http://www.phac-aspc.gc.ca/publicat/hpcdp-pspmc/30-4/preface-eng.php Accessed December 6, 2016 - Coventry J, et al. BMJ. 2000;321:36–39; 2.Richards D. Evid Based Dent. 13;14: Eke PI, Dye BA, Wei L,et al. J Periodontol. 2015;86:611–622
- Mariotti A, Hefti AF. BMC Oral Health. 2015;15(Suppl 1):S6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4580771/ Accessed October 12, 2016
- Journal of Periodontology August 2008, Vol. 79, No. 8s, Pages 1569-1576, DOI 10.1902/jop.2008.080233 (doi:10.1902/jop.2008.080233) Inflammation and Bone Loss in Periodontal Disease David L. Cochran*
- Kornman, K. Mapping the Pathogenesis of Periodontitis: A New Look. J Periodontology, August 2008 Vol. 79, No. 8s, Pages 1560-1568
- Goldstep, F. Oral Rinses for Periodontal Health. Oral Health Journal. December 1, 2014
- Side effects of chlorhexidine mouth washes., Flötra L, et al. Scand J Dent Res. 1971;79(2):119-25 Accessed October 7, 2016
- Shetty BS, Udupa SL, Udupa AL, Somayaji SN. Effect of centella asiatica L (Umbelliferae) on normal and dexamethasone-supressed would healing in wistar albino rats. Int J Low Extrem Wounds. 2006;5(3):137-143
- Harokopakis E, Albzreh MH, Haase EM, et al. Inhibition of proinflammatory activities of major periodontal pathogens by aqueous extracts from elder flower (Sambucus nigra). J Periodontol. 2006;77(2):271-279
- Woelkart K, Marth E, Suter A, et al. Bioavailability and pharmacokinetics of Echinacea purpurea preparations and their interaction with the immune system. Int J Clin Pharmacol Ther. 2006; 44(9):401-408.
- Samuels N, Grbic J, Saffer A, et al. Effect of an herbal mouth rinse in preventing periodontal inflammation in an experimental gingivitis model: A pilot study. Compendium of Continuing Education in Dentistry. Aegis Communications. March 2012, Vol 33, Issue 3.
- Levine, WZ, Samuels, N, Williams, R. Effect of a Botanical Mouth Rinse on Dental Plaque Formation: A Randomized, Double-blinded, Placebo-controlled Trial Journal of Oral Hygiene and Health August 10, 2014
- Rosen PS, Levine WZ. A Pilot Study Comparing An Alcohol Free Botanical Rinse to Chlorhexidine Rinse in Managing Post-Surgical Inflammation with Dental Implants. Submitted
- Rosen P. and Levine W. A pilot study comparing a botanical rinse to chlorhexidine rinse in managing postsurgical inflammation around dental implants.
- http://periobasics.com/immunology-of-periodontal-diseases.html Accessed March 2, 2017.
Sheri B. Doniger is a leading dental clinician, author, international educator, and consultant who currently practices dentistry in Lincolnwood, IL. Dr. Doniger is an avid researcher, frequently contributing to an array of dental publications on a variety of topics. She is a member of the IZUN Oral Healthcare Scientific Advisory Team. Please free to contact Dr. Doniger at www.donigerdental.com. Clinical photos courtesy of Dr. William Z. Levine.
RELATED ARTICLE: Oral Rinses For Periodontal Health: Simplified












