More Magazine–June 1, 2010
by Katharine Davis Fishman
Late last fall I started walking like a penguin. The array of
specialists I waddled in to see–the anesthesiologist, the physiatrist (a
doctor who supervises physical therapy and rehabilitation), the
rheumatologist, the sports-med doctor and finally the back surgeon–were
baffled by my gait and the increasingly intense throbbing in my left
buttock.
At 11 o’clock the night of the back- doctor visit, I tripped on a
rug. As I slid down the wall, my upper thigh shot out to a 45-degree
angle, and I felt an excruciating pain. “Joe, call 911!” I shouted to my
husband.
My femur, or thigh bone, had fractured. Doctors implanted a titanium
rod and two screws, and I spent three weeks,including rehab,at the
nearest regional trauma center.
Two months after the accident, when I showed up (still using a
walker) for follow-up care at Hospital for Special Surgery in New York
City, I learned that the fracture had probably been caused by
bisphosphonates. Those were the what-a-nuisance drugs that had me
getting up early, swigging down a little pill with a big mug of water
and–forbidden to eat for the next 30 to 60 minutes–enviously watching my
husband enjoy his muffin, all in the interest of avoiding . . . hip
fractures! After an osteoporosis diagnosis, I’d swallowed Fosamax for
nearly 10 years, stopped for a year after I developed an ulcer, then
spent three years on Boniva, the Sally Field drug. All this pill taking
helped; I moved from osteoporosis to osteopenia, a milder condition. And
yet a silly at-home accident had just broken my femur.
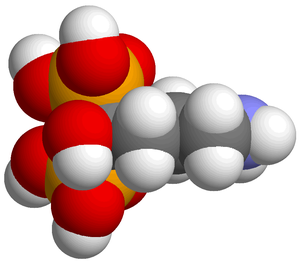
Image via Wikipedia
Around 2004, Joseph
Lane, MD, an orthopedist who’s chief of the Metabolic
Bone Disease Service at Hospital for Special Surgery, began to
notice similar strange events among some patients who’d been taking
bisphosphonates for about six years. Two women stand out particularly in
Lane’s memory. “One had been complaining of thigh pain for three
months,” he remembers. “She’d had two epidural injections for back pain,
and while she was in a swimming pool she broke her femur, simply by
turning around. Number two is a woman who was getting on a plane to go
visit her grandchildren. Similar story: She had earlier complained of
sciatica, but her doctors didn’t take an X-ray. Instead, they gave her
an MRI and an epidural injection. Then, the day of her flight, she
climbed the stairs during boarding and broke her femur going up.”
In 2005, Lane read an article in the Journal of Clinical
Endocrinology and Metabolism that jibed with what he’d been seeing.
A team at the University of Texas in Dallas and at Henry Ford Hospital
in Detroit had biopsied nine patients with osteoporosis or osteopenia,
most of whom had been taking alendronate–Fosamax’s generic name–for
three to eight years and had “spontaneous nonspinal fractures” in odd
places that took an unusually long time to heal. Bone biopsies showed
“minimal, or no, identifiable osteoblasts” (the buildup cells) and low
breakdown activity–a syndrome that became known in lay language as
frozen bone.
This was a small study with no control group, and some patients were
taking drugs besides alendronate. But the authors called for more
research “to determine how long bisphosphonates can safely be given.”
Lane and four colleagues reviewed the records of all patients admitted
to its trauma center from 2002 to 2007 with femur-shaft fractures that
were “low energy,” meaning they had been incurred while the person was
simply standing around (or splashing in a swimming pool).
The 70 trauma center patients whose cases they reviewed had all
suffered from what’s technically known as an atypical subtrochanteric
femur -fracture–and more than a third had been taking Fosamax, the
bisphosphonate that’s been available the longest. Three quarters of
these Fosamax patients shared a particular radiographic pattern: a
simple horizontal or diagonal fracture with a sort of beaky overhang of
bone. Their X-rays looked exactly like the one I was presented with two
years later. The pattern was 98 percent specific to Fosamax users, and
those who displayed it had been using the drug significantly longer than
those whose breaks did not look like that. A follow-up study matching a
smaller group of patients who had femur fractures with a control group
of subjects who had ordinary hip fractures showed roughly similar
results: Nearly a third of those with thigh fractures were on Fosamax,
as opposed to one ninth of the hip patients; two thirds of the thigh
patients on Fosamax showed the pattern, and they tended to have been on
Fosamax longer than those with hip fractures.
Meanwhile, more reports were coming out, one from Singapore and one
from Japan. Researchers hypothesized that bisphosphonates produce bone
that is brittle and fracture-prone and that the thigh pain comes from
little stress fractures that don’t heal but rather accumulate and build
up to one big kahuna of a break. The patients Lane sees are active women
seven to 10 years younger than those who break their hips (which
happens on average at age 82). “Every woman I’ve seen has been out there
shopping, working, running after her grandchildren, doing stuff,” he
says. “These are not couch potatoes. I have never seen this kind of
fracture in a nursing home patient.”
Two New York teams, one at Columbia and another (including Lane) at
Hospital for Special Surgery, recently presented small controlled
studies of postmenopausal women with osteoporosis at the 2010 annual
meeting of the American Academy of Orthopaedic Surgeons. The HSS team
biopsied osteoporotic bone while the Columbia group analyzed the
patients’ scans, and both studies buttress the theory that long-term
bisphosphonate use alters bone properties so as to increase the risk of
atypical femur fractures.
The bottom line: Experts agree that bisphosphonates prevent a lot of
fractures in elderly patients with severe osteoporosis, and more of
these people should be getting the drugs. If you are in your fifties and
have a mother in her eighties, most likely she is a better candidate
for bisphosphonate therapy than you are. Before taking these drugs,
consult with your doctor to be absolutely sure you have real
osteoporosis. If you do begin this course of therapy, get checked after
three to five years to see if you still need it.
Read the full article at more.com.










