
If you are thinking, “this article is not applicable to me”, then please consider the list of questions below:
- I am aging and when my treatment becomes too complex for my current healthcare provider, is there someone willing to treat me and will someone facilitate the transfer of my care?
- Am I willing to treat persons with disabilities?
- Do I know the readiness of my patient to be transferred and how to facilitate the transfer of care for my patients? i.e., Provide the right information and enough information for the next provider.
- Whether it is a patient who moved into my neighbourhood, or the patient is seeking my expertise, what do I need to know to best provide care for my new patient?
The relevance of this article extends beyond care for persons of disabilities because patients who were once healthy in your dental practice will age and may develop disabilities (temporary or permanent). Access to dental care is a basic human right for all patients whether they present in good general health or with disabilities.
The current reality of how persons with disabilities struggle to access care is apparent from a recent letter a parent wrote on August 18, 2023, to the Minister of Health. Below is an excerpt from the letter.
“I have a teenager with special needs. My daughter is deaf and severely developmentally delayed. This letter will give an outline of the lack of dental services for people with special needs.
My family used to live in a town in Ontario. Since my daughter was a baby, we were going to Sick Kids Hospital for years. We were introduced to their dental program there. My daughter went a few times when she was little (3-5 years old) and after that, it was impossible to find a dentist in our area to even look at her due to her issues.”
Establishing and maintaining a sustainable dental home is perhaps one of the more challenging issues across the life span for people with disabilities. It is the families of persons with disabilities who advocate for the need for care and are involved in decision-making. Tensions arise when a patient with disabilities is ready to transition, but there is no provider available and/or no process in place. Willingness to treat persons with disabilities needs to improve and processes need to be present within the healthcare system.
Major barriers to transitioning for patients with disability include:
Financial – Lack of adequate insurance, reliance on pro bono care, need for prior approval, remuneration not commensurate with increased knowledge and time, and general lack of funding for required to provide good care for case complexity.
Expertise – Low availability and education of general dentists and specialists willing to treat these patients, lack of adequate training in undergraduate and post graduate curricula, lack of a specialty to refer complex cases to and increasing life span of people with disabilities. Dentists who may have treated a person for many years but are suddenly confronted with an aging disabled person may lack the appropriate training to provide ongoing care.
Organizational – Patient’s lack of readiness, and staff time for transition planning, breaking the bond with pediatric care providers, limited knowledge about community resources that support young adults with disability, inadequate staff training, long waiting times, lack of environmental facilitators like transportation or, inadequate interprofessional communication, insufficient data or research in this arena, and inability of patients to self-advocate at dental visits.
Facilities – Structural barriers like inadequate room sizes or access to wheelchairs, lack of safe environments and equipment, lack of appropriate facilities for general anesthesia and sedation, and general insufficient training of staff.1
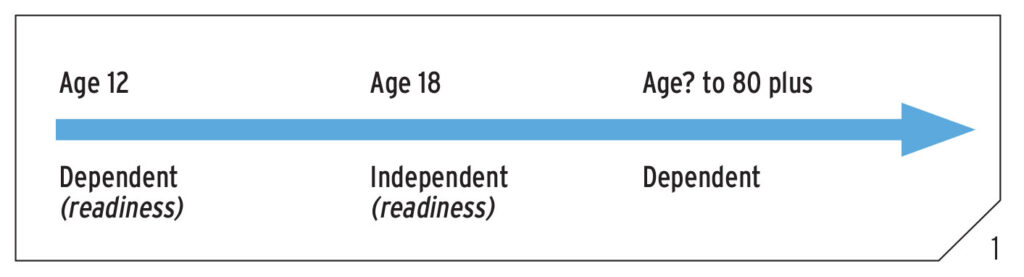
As can be seen in Figure 1, an important part of transitioning a patient from one office to another is assessment of readiness and preparing a person to move to the next stage. Information is key and it is the responsibility of the care provider to forward as much information as possible to the next treating provider. This should not be left to the patient to carry for themselves.2
Fig. 1
What tools are available to help providers gather and forward this information?
Below is a summary of the tools available from this link.3 Canadian Dental Association (cda-adc.ca; search for Case Complexity Tool).
A safe referral pathway is essential for the patient and providers involved. In conjunction with the Canadian Dental Association (CDA), a parent, and a GP provider, we {members of the Canadian Society for Disability and Oral Health (CSDH)} first assessed medical transitioning documents and then created a series of adapted forms that were piloted, revised, and are now available on the CDA website to help offices in the various stages of transitioning.
Step 1: Transition Readiness Assessment
This step is an assessment of the patient’s willingness and ability to take care of their oral health as well as preparing for more independent living. In the case of the geriatric patient, their willingness and preparedness for assisted living is assessed. Examples of questions to ask are: Are they able to make oral healthcare decisions? What is their awareness of their oral health needs? Can they express these needs? How well do they tolerate the dental environment? The assessment also has patients and their families identify difficult issues that might arise during the transition and consider actions that can be taken to alleviate these problems.
Step 2: Dental Summary and Care Plan
In this step, the current dental home care provider (often a pediatric specialist) completes a dental summary and care plan. The specialist will outline the specifics of what works and what does not work for the individual. Specific behavioral interventions can be highlighted. This information includes: What treatment has been accomplished successfully? How was this treatment provided? Sometimes the new practitioner may be unaware of specific techniques so in certain areas of the form, it will have embedded video material to help demonstrate some of the nuances of the methodologies used by the current provider. For example, how one can improve the motricity (ability to masticate) in a patient with Down Syndrome.
Step 3: Meet and Greet
Here, we provide a brief example of a letter that the new practitioner can send out to the family, welcoming them to the new practice and detailing the process by which they plan on incorporating them into the new office. Should an office be receiving a new patient that has not been seen in a previous office, the CDA also has a specific questionnaire that can help gather specific information not normally requested in new patient medical forms. Aspects, for example, relate to specific sensitivities and methodologies of self-regulation. Receiving safe care is the expectation that individuals with disabilities hold most dearly.
The dental summary care plan is an attempt to provide extra educational material to the new dental team. It also offers an opportunity to discuss financial and other perceived barriers relevant to each family.
Having made a transition, what can you (the practitioner) do to make it easier for the patient?
Any dental practice can accommodate some of the ideas below to help patients ground and calm their nervous systems. For many individuals with disabilities when they are fearful, they get locked into their sympathetic nervous systems i.e., flight, fight, freeze response. When the physiology is disrupted, then this state of threat results in the individual having the feeling of an unsafe environment. Use of simple breathing techniques and prosodic voice can re-engage the parasympathetic nervous system and provide a calming de-escalating energy. Again, gathering as much information as possible prior to a procedure will help mitigate some of these responses. When providing treatment, Figure 2 shows supportive devices like cushions, bean bags, vacupacs, and weighted blankets that go a long way to help a patient achieve allostasis (central nervous system integration). Portable radiographs can be used for patients in wheelchairs. Learning how to provide care in a wheelchair or using a transfer board to enable easy movement from wheelchair to dental chair are all basic methodologies that can be implemented in any dental practice.
Fig. 2A

Fig. 2B
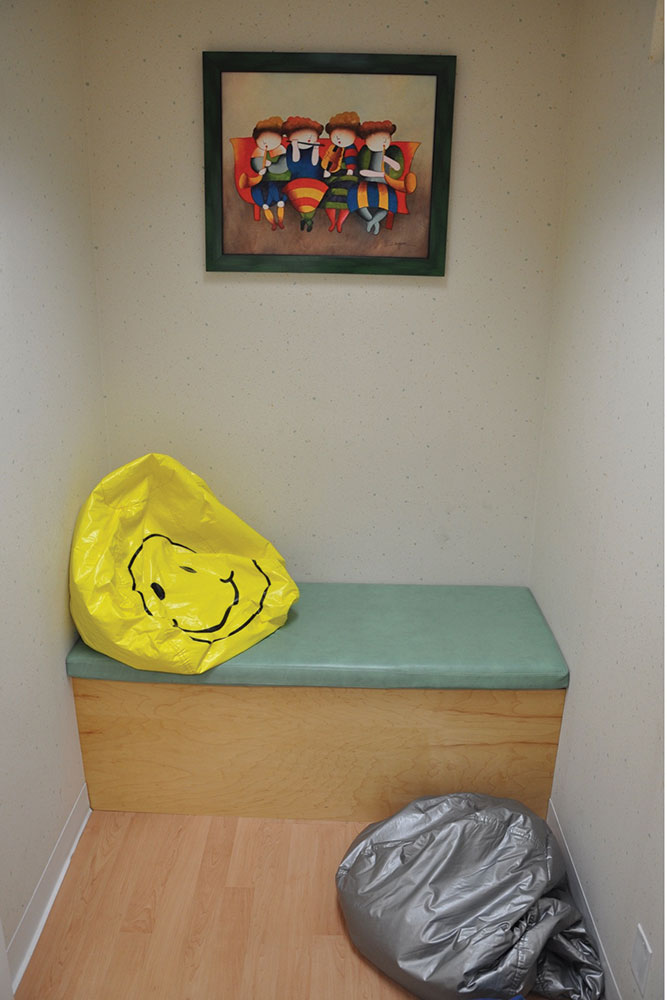
Fig. 2C

Fig. 2D

Fig. 2E

Conclusion
The development of trust and safety in a dental office setting for all persons is dependent on access to care from their dental home and consistency in their care upon transition to another provider. For individuals with disability, this is compounded because it can be difficult for them to grasp the situation, to get a clear picture, and to organize the order of the events that are happening. Situations such as this calls for cooperation of the whole team where the present team has information from the past and would “pay it forward” by sharing information with the future team. The concept of transitioning from one stage of life to the next stage of life is not new, but there has been inadequate attention to this process. Willingness to treat by the provider and acting on readiness for transition of the patient by the provider are crucial to achieve successful transitions. This is an urgent call to action for all members of the dental team to make it routine to facilitate the process for patients to maintain access to safe oral health care and a sustainable dental home.
The Canadian Society for Disability and Oral Health (CSDH) is a strong component society of the International Association for Disability and Oral Health (iADH). CSDH is the only national dental society in Canada specifically focused on oral health care for people with disabilities. Our mission is “Promoting highest quality oral health CARE for Canadians with disabilities, through Collaboration, Advocacy, Research and Education.”
Along with other important work, the CSDH is currently involved with advocacy focused on the Canadian Dental Plan and how it addresses oral healthcare for those with special needs. Learn more at Canadian Society for Disability and Oral Health (csdh.ca)
Oral Health welcomes this original article.
References
- Gréaux, M., Moro, M. F., Kamenov, K., Russell, A. M., Barrett, D., and Cieza, A. Health equity for persons with disabilities: a global scoping review on barriers and interventions in healthcare services. International Journal for Equity in Health. 2023; 22(1), 1–236. https://doi.org/10.1186/s12939-023-02035-w
- White P.H. and Cooley W.C. Transitions Clinical Report Authoring Group; American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians. Supporting the Health Care Transition from Adolescence to Adulthood in the Medical Home. Pediatrics. 2018;142(5):e20182587. Pediatrics. 2019;143(2):e20183610. doi:10.1542/peds.2018-3610
- Canadian Dental Association. The CDA Dental Patient with Special Health Care Needs Transition Process (draft). Published online August 23, 2021. cda-adc.ca; search for Case Complexity Tool.
About the Author:

Dr. Clive Friedman is a Pediatric Dentist with a long association with organizations working with persons with special needs.

Dr. Cecilia Dong is an Assistant Professor at Western University’s Schulich School of Medicine and Dentistry and is cross-appointed to the Department of Pathology and Laboratory Medicine.









