
In dentistry, zirconia restorations are the most frequently used indirect restorative material. In contrast to glass ceramics, this material can be bonded to the tooth structure using a conventional cement (e.g., resin-modified glass ionomer) if adequate retention and resistance forms are present. The material can be bonded to the tooth structure if these elements are absent or insufficient. While glass-ceramics must be bonded to the tooth structure.1 Bonding of zirconia restorations expands their clinical use, providing high-strength restorative material in minimally retentive abutments. The adoption of bonding protocols allows for more conservative and defect-oriented tooth preparations. Partial-coverage zirconia restorations have been shown to withstand in vitro thermomechanical loading when bonded to the tooth substrate.2
Bonding to zirconia has been studied extensively in the last decade. Predictable and durable outcomes are achieved when adhesive bonding protocols are followed meticulously. It’s important to highlight the technique sensitivity of the adhesive bonding procedure.3 A survey conducted in 2021 showed that only 63% of dentists followed appropriate evidence-based zirconia bonding protocols.4 Multiple simplified adhesive systems were introduced, not necessarily resulting in favourable outcomes. The intaglio surface of the zirconia requires both mechanical and chemical treatment prior to bonding to the tooth structure, also known as the APC concept. A simplified approach to the bonding of zirconia involves three steps: air-borne particle abrasion, primer application, and resin cement.5
SURFACE TREATMENT AND DECONTAMINATION OF ZIRCONIA RESTORATIONS
Saliva and blood contamination of the intaglio surface has been found to significantly decrease the bond strength of zirconia substrates. Something we initially failed to understand, which resulted in a high number of zirconia debonding during the first decade of its use. Different decontaminants have been introduced to the market. A study compared different etchants and zirconia cleaners’ ability to decontaminate the zirconia surface. Compared to other decontamination solutions, air-particle abrasion was the most efficient in mechanically removing salivary and blood contaminants and restoring the zirconia bond strength.6 Therefore, the air-particle abrasion should be performed following the restoration try-in.
Surface treatment of ceramics is critical to achieving a strong and durable bond. Glass-based ceramics such as lithium disilicate are etched with hydrofluoric acid of varying concentrations to create a porous surface. Glass-free, high-strength zirconia requires both mechanical and chemical treatment to optimize its surface for bonding and cannot be etched using conventional hydrofluoric acid etching.
Any mechanical air-particle abrasion of the intaglio surface should be carried out with extreme caution to avoid surface flaws. The mechanical air-particle abrasion with 50μm Al2O3 particles and 2.5 bar pressure for 10 seconds at a 10 mm standoff distance was observed to preserve zirconia strength. These air-particle abrasion conditions produced only a slight monoclinic phase transformation. Excessive air-particle abrasion or using large size particles will degrade the strength of the restoration as the damage will surpass the compressive stress field.7,8 The clinician should perform the air-particle abrasion process due to the importance of this step. Additionally, it was observed that priming a recently air-abraded surface generates a positive charge, enabling effective priming capability and leading to enhanced bond strength, in contrast to air-particle abrasion a few days before delivery, where surface energy dissipates and results in lower bond strength. Then followed by a chemical salination with a ceramic primer containing 10-methacryloyloxydecyl dihydrogen phosphate (MDP) monomer. The phosphoric group in the monomer promotes adhesion to the metal oxides in the air-abraded zirconia surface, and the vinyl group facilitates polymerization with unsaturated carbon bonds in the resin matrix. The ceramic primer should be scrubbed into the surface for 2-3 minutes, followed by a gentle stream of air to remove any excess solvents.9
CEMENT SELECTION
Zirconia, like any other ceramic material, cannot undergo plastic deformation; therefore, cement selection plays an important role in the longevity of the restoration. Dual-cure or self-cure adhesive or self-adhesive resin cement should be utilized when bonding zirconia restorations. The abutment tooth should be treated following the manufacturer’s instructions.10 While self-adhesive resin cements don’t require any tooth preparation, a tooth primer and a low-ph adhesive should be used when resin cement is selected. Simplified self-adhesive resin cement should be avoided when the abutment lacks mechanical retention. Some manufacturers have developed 10-MDP-containing self-adhesive cement, simplifying the bonding procedure. The effectiveness of these cements has not been heavily studied.11
LIGHT POLYMERIZATION THROUGH ZIRCONIA
Multiple factors influence resin cement polymerization under any ceramic. ceramic thickness, shade, and translucency. It can also be influenced by the polymerization type, resin cement composition, curing light’s output, curing duration, and distance.12,13
The thickness and shade of the zirconia crown play an important role in light transmission and the polymerization initiation of the resin cement.14 The International Organization for Standardization (ISO) recommends irradiance for polymerization lights of 300 mW/cm2, and the standard depth-of-polymerization requirement is 1.5 mm.15 Manufacturers’ instructions for resin-based cement may not necessarily account for the thickness and shade of the restorative material. Adequate resin cement polymerization is critical to the bond strength between the restorative material and tooth structure. Regardless of the curing unit type, and at irradiance values between 800-1200 mW/cm2, doubling the curing time (around 40 seconds) through each surface and approximating the light cure unit tip to the crown should be followed as distance impacts the amount of delivered energy. Please be aware that while increased light curing produces greater energy, increased energy also results in increased heat.16 To maintain a lower temperature while your dental assistant applies light curing to the restoration, it is advisable to direct a stream of air from the air syringe to the tip of the curing light.17
Bottom Line
Following a try-in and fit check, the adhesive bonding procedure is conducted as follows:
- The intaglio surface is air-abraded with 50μm Al2O3 particles at 2.5 bar pressure for 10 seconds at a 10 mm standoff distance.
- A ceramic primer containing 10-MDP is scrubbed into the surface with agitation for 2-3 minutes, followed by a gentle stream of air to remove any remaining solvents.
- The abutment tooth is treated according to the resin cement manufacturer’s instructions. Focus on etching the exposed enamel with phosphoric acid.
- The restoration is bonded using a dual-cure or self-cure resin cement with sufficient light polymerization.
ZIRCONIA RESIN-BONDED FIXED DENTAL PROSTHESIS
The adoption and success of zirconia bonding expanded the clinical application of zirconia. Conservative teeth replacement options while using high-strength zirconia single-wing resin-bonded bridges are possible. Congenitally missing anterior teeth require esthetic and conservative early interventions. Utilizing bonded restorations with minimally invasive and simple cantilever retainer preparations. Kern et al. published a clinical study on the longevity of resin-bonded zirconia fixed partial dentures with facial veneering porcelain. The reported success rate ranged between 76-98% based on the cause of the missing teeth with above 90% survival rate of ten years follow up.18 This treatment option provides a valid and successful outcome with minimum intervention. The International Academy for Adhesive Dentistry (IAAD) published working instructions on the bonding of zirconia resin-bonded fixed dental prostheses with emphasis on the protection of the layering porcelain during the intaglio surface treatment.19
CLINICAL CASE
An 18-year-old patient presented to our clinic with two congenitally missing laterals (Fig. 1). Too young to receive implants, an ideal space for both implants was created by the orthodontist (Fig. 2). To conserve tooth structure and provide a long-term interim prosthesis, a 3Y-zircona resin-bonded bridge was selected. For cantilevering, teeth 8 and 9 were chosen due to their greater surface area and less complex anatomy in comparison to teeth 6 and 11. The lingual preparation involves a 0.3-0.5mm reduction, staying in enamel, with a light chamfered margin and 2 mm away from the incisal edge. A pinhole is placed in the middle of the preparation for resistance and placement. The proximal side of the tooth preparation adjacent to the edentulous area is additionally reduced pushing the margin towards the facial to allow for more thickness of the zirconia at the connector (Fig. 3). The connector dimension should be 3×2.5 mm (Fig. 4). The bonding protocol should be followed as described, meticulously! The final outcome is a 3Y-zirconia resin-bonded fixed dental prosthesis with facial porcelain layering to add characterization (Fig. 5).
 Fig. 1
Fig. 1

Fig. 2

Fig. 3

Fig. 4
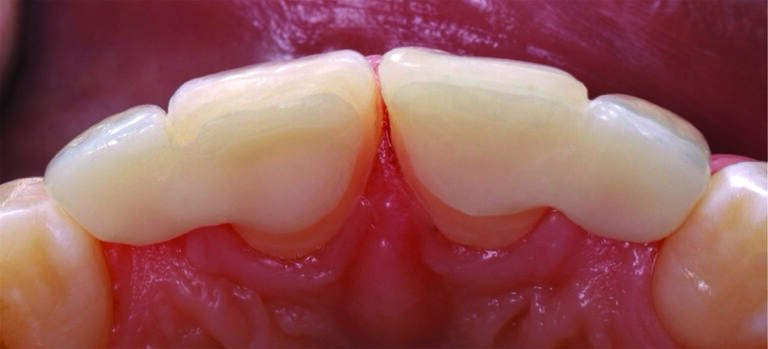
Fig. 5

Oral Health welcomes this original article.
References
- Heboyan A, Vardanyan A, Karobari MI, et al. Dental Luting Cements: An Updated Comprehensive Review. Molecules. 2023;28(4). doi:10.3390/molecules28041619
- Gupta S, Abdulmajeed A, Donovan T, Boushell L, Bencharit S, Sulaiman TA. Monolithic Zirconia Partial Coverage Restorations: An In Vitro Mastication Simulation Study. Journal of Prosthodontics. 2021;30(1). doi:10.1111/jopr.13287
- Inokoshi M, De Munck J, Minakuchi S, Van Meerbeek B. Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res. 2014;93(4). doi:10.1177/0022034514524228
- Ostermann F, Meyer G, Kern M. Survey of clinically used adhesive ceramic bonding methods – follow up after 12 years. Dental Materials. 2021;37(4). doi:10.1016/j.dental.2020.11.018
- Blatz MB, Alvarez M, Sawyer K, Brindis M. How to Bond Zirconia: The APC Concept. Compend Contin Educ Dent. 2016;37(9).
- Sulaiman TA, Altak A, Abdulmajeed A, Rodgers B, Lawson N. Cleaning Zirconia Surface Prior To Bonding: A Comparative Study of Different Methods and Solutions. Journal of Prosthodontics. 2022;31(3). doi:10.1111/jopr.13389
- Zhang Y, Lawn BR, Rekow ED, Thompson VP. Effect of sandblasting on the long-term performance of dental ceramics. J Biomed Mater Res B Appl Biomater. 2004;71(2). doi:10.1002/jbm.b.30097
- Chintapalli RK, Marro FG, Jimenez-Pique E, Anglada M. Phase transformation and subsurface damage in 3Y-TZP after sandblasting. Dental Materials. 2013;29(5). doi:10.1016/j.dental.2013.03.005
- De Souza G, Hennig D, Aggarwal A, Tam LE. The use of MDP-based materials for bonding to zirconia. Journal of Prosthetic Dentistry. 2014;112(4). doi:10.1016/j.prosdent.2014.01.016
- Karimipour-Saryazdi M, Sadid-Zadeh R, Givan D, Burgess JO, Ramp LC, Liu PR. Influence of surface treatment of yttrium-stabilized tetragonal zirconium oxides and cement type on crown retention after artificial aging. Journal of Prosthetic Dentistry. 2014;111(5). doi:10.1016/j.prosdent.2013.09.034
- Yazigi C, Alawi S, Wille S, Lehmann F, Kern M. Durability of Resin Bonding to Dental 3Y-TZP Zirconia Using Different Adhesive Systems. Materials. 2024;17(2). doi:10.3390/ma17020424
- Myers ML, Caughman WF, Rueggeberg FA. Effect of Restoration Composition, Shade, and Thickness on the Cure of a Photoactivated Resin Cement. Journal of Prosthodontics. 1994;3(3). doi:10.1111/j.1532-849X.1994.tb00146.x
- Chaiyabutr Y, Kois JC, LeBeau D, Nunokawa G. Effect of abutment tooth color, cement color, and ceramic thickness on the resulting optical color of a CAD/CAM glass-ceramic lithium disilicate-reinforced crown. Journal of Prosthetic Dentistry. 2011;105(2). doi:10.1016/S0022-3913(11)60004-8
- Pazin MC, Moraes RR, Gonçalves LS, Borges GA, Sinhoreti MAC, Correr-Sobrinho L. Effects of ceramic thickness and curing unit on light transmission through leucite-reinforced material and polymerization of dual-cured luting agent. J Oral Sci. 2008;50(2). doi:10.2334/josnusd.50.131
- International Organization for Standardization ISO/TS 10650. Dental equipment—powered polymerization activators. International Organization for Standardization: Geneva, Switzerland; 1999.
- Sulaiman TA, Abdulmajeed AA, Donovan TE, et al. Optical properties and light irradiance of monolithic zirconia at variable thicknesses. Dental Materials. 2015;31(10). doi:10.1016/j.dental.2015.06.016
- Mouhat M, Mercer J, Stangvaltaite L, Örtengren U. Light-curing units used in dentistry: factors associated with heat development—potential risk for patients. Clin Oral Investig. 2017;21(5). doi:10.1007/s00784-016-1962-5
- Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017;65. doi:10.1016/j.jdent.2017.07.003
- Ozcan M. Air abrasion of zirconia resin-bonded fixed dental prostheses prior to adhesive cementation: why and how? J Adhes Dent. 2013;15(4). doi:10.3290/j.jad.a30476
About the Authors:

Dr. Taiseer Sulaiman is a tenured associate professor at the Adams School of Dentistry, University of North Carolina, Chapel Hill. He is a wet-handed clinician who is passionate about bridging the gap between material selection and clinical application. He has published over 80 peer-reviewed articles, book chapters, and abstracts. He has presented on many national and international stages and is a member of numerous dental academies.

Dr. Tariq Alsahafi is a PhD candidate in the oral and craniofacial biomedicine program at Adams School of Dentistry and the lab manager of Sulaiman’s Biomaterials Laboratory.









