
Epinephrine is the second-most frequently administered medication by dentists as it is present in almost all local anesthetic cartridges. Epinephrine is an endogenous hormone released from the adrenal medulla. Its main function is to support the body in times of physiologic stress by increasing cardiac output and glucose delivery to tissues.1 Within dentistry, epinephrine serves as a beneficial adjunct to local anesthesia due to its potent vasoconstrictive properties. This provide hemostasis, prolonged duration of action, better depth of numbness, as well as decreased local anesthesia toxicity due to delayed systemic absorption.2 Although beneficial, these same properties require caution with certain patient populations that are susceptible to extreme changes in cardiac and vascular function.
Pharmacodynamics
To best appreciate the risks with epinephrine use, the physiologic mechanism of this medication must be understood. Epinephrine is a non-specific α and β agonist for the sympathetic nervous system, meaning that it directly activates α1, α2, β1, and β2 adrenergic receptors.
Alpha-1 adrenergic receptor activation causes peripheral vasoconstriction that increases blood pressure. This action also redirects blood flow from the periphery into central compartments (such as the heart), making it a lifesaving medication in cases of cardiac arrest.1 It also reduces hypotension and the incidence of shock during anaphylaxis.3
The activation of α2 receptors inhibits insulin release from the pancreas and stimulates glucagon secretion. This increases glucose concentration in the blood for improved “fight or flight” responses by the body’s muscles.
The β1 action of epinephrine results in increased chronotropy (heart rate) and inotropy (contractility) of the heart. Some dental patients incorrectly believe these effects to be an “allergy” to epinephrine when they detect a faster, bounding heart rate.
Epinephrine binds to β2 receptors resulting in bronchodilation of the airways and peripheral vasodilation of the arterioles. This bronchodilation can be lifesaving in cases of anaphylaxis and severe asthma to allow improved air entry into the lungs.3
Understanding the risks
Different levels of physical activity result in varying degrees of endogenous epinephrine secretion. Patients with cardiovascular comorbidities may become symptomatic (e.g., chest pain, shortness of breath) with light physical activity or even at rest. Therefore, the amount of exogenous epinephrine we administer to patients must not exceed what they can physiologically tolerate.
Dr. Charles Richard Bennett published the most frequently referenced suggestion for those with cardiovascular comorbidities stating that they should only receive doses of up to 0.04 mg of epinephrine.4 Unfortunately, there lacks scientific evidence supporting this dose, but it can provide clinicians with a theoretical approach to minimizing patient risk. If larger amounts are required, blood pressure and heart rate should be monitored post injection, and doses should be spread throughout the appointment. The use of local anesthetics without epinephrine is also a valuable tool. Generally, the use of epinephrine impregnated retraction cords in susceptible patients is contraindicated as the absorbed dose can exceed the accepted per appointment maximum adult dose of 0.2 mg.5
It is important to note that pain and anxiety caused by lack of adequate anesthesia during dental treatment can result in release of endogenous catecholamines that exceeds the recommended limits of epinephrine administration provided in some dental guidelines. The American Dental Association references the use of a maximum of 0.04 mg per appointment.6 Therefore, complete avoidance of epinephrine is not recommended.
Epinephrine use is cautioned in the following scenarios:
a) Hypertension
Hypertension is a systemic disorder typically caused by decreased compliance of arterial vasculature and thickening of the vessel walls.7 Patients with poorly controlled hypertension can experience labile blood pressures and extreme responses to vasopressors.7 Therefore, epinephrine should be limited to 0.04 mg per appointment.
b) Coronary artery disease
Angina is a chest pain that occurs due to imbalance in myocardial oxygen supply and demand. In most cases, atherosclerotic plaque formation inside the lumen of the coronary arteries results in decreased oxygen supply to the myocardium.8 Therefore, increases in cardiac work are poorly tolerated. Tachycardia and hypertension caused by epinephrine can be life threatening in these patients and should be used judiciously.9
c) Hyperthyroidism
Hyperthyroidism is a disorder of elevated serum levels of thyroid hormones T3 and T4. These hormones affect almost all organ systems in the body and increase expression of the β1 receptors of the heart.10 This causes increased cardiac contractility, tachycardia, and hypertension. Uncontrolled hyperthyroidism can rapidly become life threatening and the combination with epinephrine may result in fatal dysrhythmias, hypertension, and adverse cardiac events.11 Epinephrine use should be limited in patients who are not currently euthyroid.
d) β-blockers
β-blockers, even if selective for β1 receptors, cause a certain degree inhibition of the β2 receptor. This will decrease peripheral vasodilation of skeletal muscle resulting in unopposed α1 vasoconstriction in patients receiving epinephrine. This may lead to significant increases in blood pressure, especially with inadvertent intravascular injections.12
e) Cocaine and methamphetamines
Cocaine and methamphetamine are stimulant substances, and similarly to epinephrine, have potent vasoconstrictive properties. In fact, their mechanism of action involves decreasing the reuptake of available epinephrine and norepinephrine in the body.13 The additive effects of stimulants and epinephrine can result in severe hypertension that can result in end organ damage. The main concern is that of a hemorrhagic stroke, myocardial infarction, and cardiac arrest.13 Patients should not receive any dose of epinephrine within at least 24 hours of cocaine or methamphetamine use to allow adequate time for drug clearance.14
f) Sulfite sensitivity
Allergies to epinephrine are exceedingly rare, with very few case reports available.15 True allergies to local anesthetics containing epinephrine are most often due to the metabisulfite preservative. The incidence of contact allergy to sulfites ranges from 1-7% depending on the population studied and is significantly higher in asthmatic populations.16 Therefore, patients with these allergies should receive plain local anesthetic.
g) Pheochromocytoma
A pheochromocytoma is a catecholamine secreting tumour of the adrenal gland. These are often associated with sympathetic nervous system surges due to the presence of excess of endogenous epinephrine and norepinephrine. Epinephrine-containing local anesthetics are contraindicated as this interaction may lead to life-threatening dysrhythmias, tachycardia, and hypertension.17
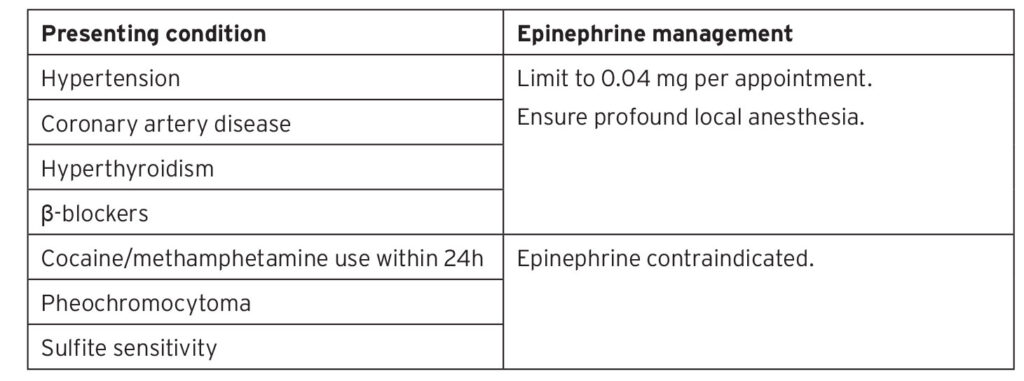
Table 1: Summary of Recommendations for Epinephrine Management in Dentistry
Conclusion
Epinephrine is a beneficial adjunct in local anesthesia for prolonging the duration of action, increasing the profoundness of numbness, and decreasing risk of local systemic anesthesia toxicity. Aspiration should be carried out when injecting local anesthesia to avoid inadvertent intravascular injections. Certain patients, however, should have increased monitoring, decreased dosing, or avoidance of its use.
Oral Health welcomes this original article.
References
- Soar, J., & Berg, K. M. (2021). Early Epinephrine Administration for Cardiac Arrest. JAMA network open, 4(8), e2120725. https://doi.org/10.1001/jamanetworkopen.2021.20725
- Achar, S., & Kundu, S. (2002). Principles of office anesthesia: part I. Infiltrative anesthesia. American family physician, 66(1), 91–94.
- Lieberman, P., Nicklas, R. A., Randolph, C., Oppenheimer, J., Bernstein, D., Bernstein, J., Ellis, A., Golden, D. B., Greenberger, P., Kemp, S., Khan, D., Ledford, D., Lieberman, J., Metcalfe, D., Nowak-Wegrzyn, A., Sicherer, S., Wallace, D., Blessing-Moore, J., Lang, D., Portnoy, J. M., … Tilles, S. A. (2015). Anaphylaxis–a practice parameter update 2015. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology, 115(5), 341–384. https://doi.org/10.1016/j.anai.2015.07.019
- Bennett C. R. (1984). Monheim’s Local Anesthesia and Pain Control in Dental Practice (7th ed.). St Louis/Mosby.
- Polat, N. T., Ozdemir, A. K., & Turgut, M. (2007). Effects of gingival retraction materials on gingival blood flow. The International journal of prosthodontics, 20(1), 57–62.
- American Dental Association. (2022, Nov 1). Hypertension (High Blood Pressure). https://www.ada.org/en/resources/research/science-and-research-institute/oral-health-topics/hypertension
- Yancey R. (2018). Anesthetic Management of the Hypertensive Patient: Part I. Anesthesia progress, 65(2), 131–138. https://doi.org/10.2344/anpr-65-02-12
- Brown, H. and Cook, T. (2014), Ischaemic heart disease unmasked by adrenaline injection during dental surgery. Anaesthesia Cases, 2: 57-59. https://doi.org/10.21466/ac.IHDUBAI.2014
- Ambrose, J. A., & Singh, M. (2015). Pathophysiology of coronary artery disease leading to acute coronary syndromes. F1000prime reports, 7, 08. https://doi.org/10.12703/P7-08
- Singh, I., & Hershman, J. M. (2016). Pathogenesis of Hyperthyroidism. Comprehensive Physiology, 7(1), 67–79. https://doi.org/10.1002/cphy.c160001
- Lee, K. J., Park, W., Pang, N. S., Cho, J. H., Kim, K. D., Jung, B. Y., & Kwak, E. J. (2016). Management of hyperthyroid patients in dental emergencies: a case report. Journal of dental anesthesia and pain medicine, 16(2), 147–150. https://doi.org/10.17245/jdapm.2016.16.2.147
- Hersh, E. V., & Giannakopoulos, H. (2010). Beta-adrenergic blocking agents and dental vasoconstrictors. Dental clinics of North America, 54(4), 687–696. https://doi.org/10.1016/j.cden.2010.06.009
- Hill, G. E., Ogunnaike, B. O., & Johnson, E. R. (2006). General anaesthesia for the cocaine abusing patient. Is it safe?. British journal of anaesthesia, 97(5), 654–657. https://doi.org/10.1093/bja/ael221
- Jufer, R. A., Wstadik, A., Walsh, S. L., Levine, B. S., & Cone, E. J. (2000). Elimination of cocaine and metabolites in plasma, saliva, and urine following repeated oral administration to human volunteers. Journal of analytical toxicology, 24(7), 467–477. https://doi.org/10.1093/jat/24.7.467
- Kohase, H., & Umino, M. (2004). Allergic reaction to epinephrine preparation in 2% lidocaine: two case reports. Anesthesia progress, 51(4), 134–137.
- Ralph, N., Verma, S., Merry, S., Lally, A., Kirby, B., & Collins, P. (2015). What is the relevance of contact allergy to sodium metabisulfite and which concentration of the allergen should we use?. Dermatitis : contact, atopic, occupational, drug, 26(4), 162–165. https://doi.org/10.1097/DER.0000000000000120
- Ramachandran, R., & Rewari, V. (2017). Current perioperative management of pheochromocytomas. Indian journal of urology : IJU : journal of the Urological Society of India, 33(1), 19–25. https://doi.org/10.4103/0970-1591.194781
About the Author:

Dr. Lucia Santos is a current third-year dental anesthesiology resident at the University of Toronto, where she had previously completed her Doctor of Dental Surgery degree. She can be reached at lucia.santos@mail.utoronto.ca.









