Introduction
Non-sterile clinical gloves are a key component of Standard Precautions. It was envisaged that their use, when there was a risk of direct contact with blood, body fluids, non-intact skin or mucous membranes, would prevent potential pathogens in those locations from being transmitted to other patients and, therefore, assist in reducing healthcare associated infections. As is often the case with seemingly logical actions, the wearing of gloves has had unintended consequences as illustrated by the following titles of recent articles in professional and lay publications.
“Contaminated Gloves Increase Risks of Cross-Transmission of Pathogens.” American Society of Microbiology, June, 2016
“ Hygienic? No, Your Doctor’s Rubber Gloves Could Infect You With a Superbug.” Mail Online, August, 2012.
“Wearing Gloves: The Worst Enemy of Hand Hygiene?” Future Microbiology, June, 2011.
“Gloves Are No Guarantee Your Doctor’s Hands Are Clean.” The New York Times, November, 2011
“The Misuse and Overuse of Non-Sterile Gloves: Application of an Audit Tool to Define the Problem.” Journal of Infection Prevention, February, 2015.
Rather than prevent infections, it appears that glove wearing has a real potential for spreading disease. This article will attempt to describe why this has occurred and how it might be corrected. It will begin with discussing the role that hands play in the spread of disease.
Hands and Disease Transmission
Microbiology
It is now appreciated that the hands of health care workers (HCWs) are frequently colonized by transient micro-organisms such as; methicillin resistant S. aureus, vancomycin resistant Enterococcus, Candida species, and Clostridium difficle. 1 Approximately 30,000 to 40,000 skin epithelial cells containing viable pathogens are shed per hour from normal skin. Dirty hands and these shed cells have the potential to contaminate exposed skin, uniforms, chairside furniture, bibs, equipment and instruments in the patient’s immediate environment. When clean hands touch those objects they- in turn- are colonized by the pathogens creating a potential for cross-contamination. 1
This explains why contaminated hands and shed cells from the hands of HCWs act as efficient means of spreading pathogens across working and non-working surfaces, between patients, and between clean areas and contaminated locations on the same patient, and are a significant cause of health care associated infections (HCAIs). 2 Although these transient micro-organisms are readily removed from the skin surface by water and soap or are destroyed by alcohol hand rubs, the HIV/AIDS scare of the mid-1980s promoted the wearing of gloves by HCWs as an extra precaution against the spread of HCAIs. To understand why glove use is now associated with disease transmission, it is necessary to discuss failures in the five moments for hand hygiene, cross contamination, and the misuse of non-sterile clinical gloves.
Five Moments for Hand Hygiene
In 2007 Sax and colleagues developed the concept of “My Five Moments for Hand Hygiene. 3 It describes work situations commonly experienced by HCWs when hand hygiene is needed to effectively reduce the potential for microbial transmissions during the administration of treatment. The five moments are described in Table 1.
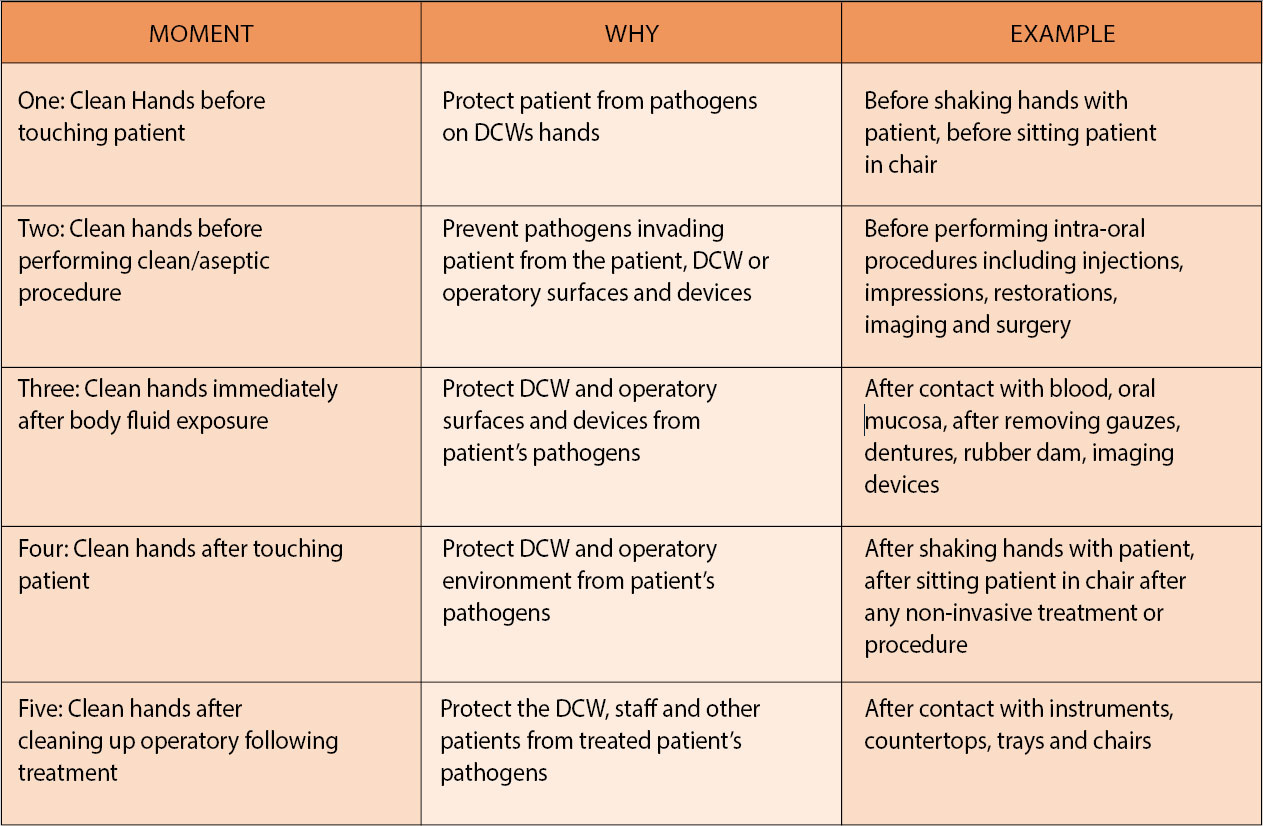
To provide a dental perspective, the Table is a modification of the Five Moments for Hand Hygiene (5MHH) published by the World Health Association. 4 The examples offered are for illustrative purposes and are not the only situations where the five moments should be enacted.
The five moments are standardized logical actions which can be applied to a wide range of health care activities. They are simple to teach, practice and monitor. They avoid the introduction of individual variations on when hands should be cleaned. 3 They have been endorsed by the World Health Organization (WHO) as their strict adherence in both developed and developing countries does result in significant decreases in HCAIs. 1 In fact, according to the WHO, the simple five moments for hand hygiene properly practiced are one of the most important and effective methods of infection control. 5 Therefore, it follows that failure to perform any of the five moments will result in contaminated hands which have the potential to spread disease.
Hands and Cross Contamination
Sax and colleagues reported a compliance rate for hand hygiene at less than 50% among hospital staff. 3
Dr. Jennie Wilson, a prominent UK infection control researcher, found that the adherence to proper hand hygiene among HCWs was around 40%. 6 A 1999 study of Canadian Dentists demonstrated that the percentage of dentists who did not wash their hands before patient contacts ranged from 13-60%. 7 More recently 19% of USA dentists admitted to never washing or disinfecting their hands between patients. 8
These findings support the conclusion by Larsen that the adherence by HCWs to proper hand hygiene is abysmal. 9 The potential for dirty hands to spread disease is real and has not be reduced by the equally abysmal failure of most hand hygiene compliance programs. 10 Unfortunately, glove wearing by HCWs has not compensated for the inadequacies in hand hygiene. To understand why, it is necessary to discuss the use and misuse of non-sterile clinical gloves. In the following text NSCGs and gloves will be used interchangeably to refer to non- sterile clinical gloves. Sterile gloves used in the operating room are not the subject of this article.
Non-sterile Gloves and Disease Transmission
Non-sterile Clinical Gloves –Their Use
In 1996 as part of Standard Precautions, non-sterile clinical gloves (NSCGs) were to be worn by HCWs when exposure to blood, body fluids, mucous membranes and non-intact skin was anticipated. 11,12 This is a highly specific purpose. These exposures create “portals of entry” and make vulnerable patients prone to cross-contamination from micro-organisms present on the hands of HCWs who might have previously treated a patient with an undiagnosed blood- borne infection. 13 The primary purpose for wearing NSCGs was and remains the protection of the patient. 13 The fact that gloves might also protect the HCW is a secondary consequence. 13 Equally important is the removal of the gloves immediately after the contact which justified their use. 13 This ensures that potential blood-borne infections from the treated patient are not transferred to other patients, equipment, or surfaces. 13 Thus, when used properly, NSCGs should assist in reducing the likelihood of cross-contamination and hence the number of HCAIs. 11,12 To-day, the specific purpose for wearing NSCGs appears to have been lost as their use has become routine throughout all aspects of healthcare delivery. 14 This common but inappropriate behaviour poses a real risk for cross-contamination. 15
Non-sterile Clinical Gloves –Their Misuse
Throughout the last twenty five years numerous clinical investigations have been undertaken on the glove wearing habits of HCWs. For example, in 1997 Thompson et al found that the rate for not changing gloves at the appropriate time was as high as 84%. 16 Girou in 2004 was able to recover pathogens from 86% of the NSCGs used by HCWs. 12 A controlled trial by Bearman and colleagues in 2007 demonstrated a definite increase in the number of HCAIs when NSCGs were used for all patient contacts compared to the number of such infections when the gloves were used solely for their intended purpose. 17 The investigation by Fuller in 2011 confirmed that gloves were not being changed between patient contacts and that compliance with routine hand hygiene was significantly reduced when NSCGs were used. 18 Moore et al in 2013 reaffirmed that during their use gloves do become contaminated with micro-organisms which, in turn, are transferred to other surfaces touched by the gloves and, when removed, to the wearer through the phenomenon of “back spray”. 19 In 2013 Wilson recorded a 33% failure rate to wash hands after gloves were removed, and that in 5% of cases a gloved hand touched 5 objects before performing the procedure justifying the glove usage. 20 Loveday in 2014 and Wilson in 2017 observed that among all HCWs up to 58% of glove wearing episodes were unnecessary and unjustified. 21,2 An interesting finding by Hughes in 2013 was that during the retrieval of NSCGs in an orthopedic ward, the dispensers containing them were contaminated by the skin commensals and pathogens on the hands of HCWs. 22 In turn, this creates the very real potential of fresh gloves being contaminated before they are used, and the realization that boxes of NSCGs are a source of spreading pathogens throughout the entire clinical environment. Such a situation has been identified in the dental office. 23
The significant findings from these and similar studies are:
- if gloves are not removed after contact with potentially infectious sources they assume the qualities of a contaminated “second skin” and that these dirty gloves are capable of causing cross-contamination in a similar manner as dirty hands; 24,25,26
- in many instances gloves are not changed at the appropriate time; 16
- the habitual use of gloves over a wide range of health care activities means that in many instances their use is inappropriate. 15
From this Wilson and others have agreed that NSCGs are being misused because they are:
- put on when not required;
- put on too early;
- removed too late;
- not changed at critical points in patient care. 2,15,18
Wilson and others have proposed that the overuse and misuse of gloves has desensitised HCWs to the triggers that would normally initiate hand hygiene as dictated by the five moments. 14,15,18,21 In her recent paper, Wilson lists the failures to recognize these triggers and by relating them to the 5MHH illustrates why the misuse of gloves creates a potential for HCAIs. 2 Table 2 describes this situation from a dental perspective.

Not donning fresh NSCGs immediately before exposure to a patient’s body fluids, mucous membranes or non-intact skin but continuing to wear ones which have been used for prior procedures is a failure to acknowledge the significance of Moment 2. In dentistry, an example of this would be wearing the same pair of gloves to handle non-sterile items prior to an intra-oral procedure as are worn while performing the procedure. Situations where this might occur are the wearing of NSCGs while placing bibs or protective glasses on patients, entering drawers, touching countertops, giving mouthwashes or medications and recording histories. Similarly, failure to remove gloves immediately after an exposure prone procedure is a violation of Moment 3. In dentistry, this would be the equivalent of the gloves that were worn for an intra-oral procedure being used to clean up after the procedure. HCWs who ignore the occasions when gloves should be removed, hand hygiene performed and, if necessary, fresh gloves worn, are creating lapses in infection control which in 50% of such instances produce a potential for cross-contamination and an increase in HCAIs. 2
The majority of investigations on NSCGs have involved medical and/or nursing personnel. However, it would be naïve to assume that dental staff are not similarly abusing gloves. Wearing the same pair of gloves while roaming from one operatory to another, not changing gloves between patients, wearing the same pair of gloves while performing separate intra-oral procedures on the same patient, removing gloves and donning fresh ones without hand hygiene, wearing gloves while greeting and seating patients and recording their histories, wearing gloves while in non-clinical environments, wearing gloves while performing an external TMJ examination or lymph node assessment, and somehow believing that wearing gloves justified less rigorous hand hygiene practices, are all examples of the misinformed and unjustified use of gloves. If gloves are being used inappropriately, it is reasonable to ask, “Why wear them?”
To understand why this almost universal pervasive misuse of gloves has occurred, it is necessary to explore the drivers for glove wearing by HCWs.
The Drivers of Glove Use
As part of Universal Precautions gloves were to be worn when contacting blood and other body fluids known to be infected with HIV, HBV and other blood borne pathogens. 27 Thus, before gloves were required to be worn the patient’s infectious status had to be determined. This all changed with Standard Precautions. They required that gloves were to be worn when performing exposure prone procedures such as contacting blood, body fluids, mucous membranes or non-intact skin regardless of the patient’s infectious status. 27 Standard Precautions negated the need to perform a risk assessment prior to such procedures. The unintended result of Standard Precautions was that HCWs treated all procedures as risky and so began wearing NSCGs for all patient contacts. Why such behaviour should occur was the catalyst for series of interviews with HCWs conducted by Loveday in 2014 and Wilson in 2017. 2,21 They found that the two principal reasons why HCWs wore gloves were based on emotion and socialization.
Emotion as a Driver
Common emotions justifying glove use were: self- protection against unspecified pathogens; prolonged use to ensure self-protection; easing mental stress from fears of contamination; disgust at touching patients, surfaces and items perceived as being unclean; saving time and reducing the need for hand hygiene; and by depersonalizing care there was the avoidance of demonstrating disgust at performing unpleasant tasks. 2,6,13,28 Surprisingly, HCWs either were not concerned with or unaware of the fact that gloves are not sterile coverings for hands but become contaminated and pass on infections in a manner similar to dirty hands.6 Common attitudes and beliefs regarding the wearing of NSCGs are identified in this response received by Wilson.
“Obviously, the idea is to protect yourself and the patient from infection so I suppose you could say that you should wear them all the time, which all of us do to be honest, you don’t know what patients have infections you don’t know that if you haven’t got information then you treat everybody the same so you’re protecting yourself and you’re protecting the public.” 2
Based on her interviews with HCWs, Wilson has concluded that, “The decision to wear NSCGs was strongly influenced by an emotional need for protection of self, driven by fear and disgust.” 2
Socialization as a Driver
The ready availability of NSCGs appears to give HCWs permission to routinely wear them without assessing – as mandated by infection control recommendations – if the risks associated with a specific procedure justify their use. 2 Many HCWs admitted to “automatically” wearing gloves despite their training and infection control policies recommending otherwise. 2 Peer behaviour did influence glove use but not without reservations. The following is an example of a HCW’s approach to NSCGs.
“I would use personal experience and knowledge. I wouldn’t be influenced by somebody saying you don’t need to wear gloves if I feel I need to wear gloves I would wear them.” 2
Not surprisingly, Wilson found that the most common influence on nurses’ decisions to wear gloves was their own judgement. This was so strongly held that, as demonstrated in the above quotation, it was not open to being challenged. 2 Other influences in descending order were infection control policies, the advice from lecturers/trainers and directions received from senior staff. 2
There is minimal information on to what degree the public`s perception of glove wearing influences the decisions of HCWs. The idea that glove wearing might give patients the impression that they are dirty or contagious does not appear to be an influencing factor. 2 However, patients do have their opinions on the use of NSCGs. A recent study found that 63% of patients had a negative opinion on glove use including observations that they were overused, not changed between patient tasks or patients, worn to avoid hand hygiene and used primarily for the benefit of the treating personnel who disliked being questioned on their use. 15 In addition, those patients were never asked if they had an allergy to the gloves’ ingredients. 15 Only 24% of patients had a positive approach to NSCGs which included the idea that HCWs knew when to wear them to avoid infections, and that hands were protected by them. 15 The same group of patients believed that the routine wearing of gloves was unifying as it prevented the identification of infected patients. 15 Patients are excused for having this idea, but HCWs ought to know that such an outcome was not the purpose of Universal or Standard Precautions.
Influences on Dental Staff
Many dental procedures are intra-oral and exposure prone, which according to Standard Precautions justifies glove wearing. However, it is reasonable to assume that like other HCWs, the primary reason for dental staff using NSCGs is self-protection. With this as the primary and seemingly dominating non-questionable influence, it is highly likely that gloves are routinely used by dental staff for procedures for which there is no justification apart from one of self- protection. If the answer to “Why Wear Them” is “To Protect Myself”, dental staff might wish to consider that practicing proper handwashing is the most effective method of protecting themselves and their patients.
Discussion
The references cited throughout this article represent a small sample of the numerous studies on the side effects of wearing NSCGs. The conclusion to be drawn from these investigations is that by their inappropriate use of gloves and less reliance on hand hygiene, HCWs are promoting health care associated infections and compromising the goals of Standard Precautions. Unfortunately, there is no reason to assume that the dental environment is immune to this infection control dilemma. It is suspected that the majority of dental staff misuse gloves and in doing so, no doubt unintentionally, violate the principles governing Standard Precautions. The correction of this situation will require that dental staff are emphatically informed that glove use is not a substitute for enacting the five moments for hand hygiene. They must appreciate that proper infection control necessitates assessing the risk of infection-principally to the patient-before donning gloves. This means that infection control recommendations must indicate clearly not only when and how gloves should be used but when and why they should not be used. Such actions should reduce self- protection and personal judgements as the principal drivers of glove use and permit glove use to be questioned by peers and patients. If this causes the habitual and inappropriate use of NSCGs to be broken and replaced by rational behaviour, it is possible that the intended purpose of Standard Precautions will be accomplished and that dental offices will not be the source of spreading health care associated infections. However, a simpler solution is at hand. The current misuse of gloves by dental staff has the potential to cause disease transmission. To avoid such an unintended consequence the profession should forget gloves and revert back to the simple, cheap, effective and environmentally friendly practice of hand washing albeit modernized to reflect the Five Moments for Hand Hygiene.
References
- P. Mathur, Hand hygiene: Back to the basics of infection control. Indian J Med Res 2011; 134(5): 611-620.
- J. Wilson et al, Applying human factors and ergonomics to the misuse of nonsterile clinical gloves in acute care. Am J Infect Control 2017; 45(7): 779-786.
- H. Sax et al, “My five moments for hand hygiene”: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hospital Infection 2007; 67: 9-21.
- World Health Association, Hand Hygiene: Why, How & When? 2009
- Guide to implementation of the WHO multimodal hand hygiene improvement strategy. Available at: http://www.who.int/patientsafety/en/
- J. Wilson, Hand hygiene: to glove or not to glove. Nursing Review 2015; 15 (5):1-10.
- G. M. McCarthy et al, Infection Control Practices Across Canada: Do Dentists Follow the Recommendations? J Can Dent Association 1999; 65: 506-511.
- R. Myers et al, Hand Hygiene Among General Practice Dentists: A Survey of Knowledge, Attitudes and Practices. JADA 2008; 139(7): 948-957.
- E. Larson et al, Compliance with handwashing and barrier precautions. J Hospital Infection 1995; 30: 88-106.
- M. Whitby et al, Why Healthcare Workers Don’t Wash Their Hands: A Behavioral Explanation. Infection Control Hospital Epidemiology 2006; 27(5): 484-492.
- M. Eveillard, Wearing gloves: the worst enemy of hand hygiene. Future Microbiology 2011; 6(8):835-837
- E. Girou et al, Misuse of gloves: the foundation for poor compliance with hand hygiene and potential for microbial transmission? J Hospital Infection 2004; 57: 162-169.
- J. Wilson et al, Does glove use increase the risk of infection? Nursing Times; 2014; 110 (39): 12-15.
- J. Wilson et al, The misuse and overuse of non-sterile gloves: application of an audit tool to define the problem. J Infect Prevention 2015; 16(1): 24-31.
- J. Wilson et al, Public perceptions of the use of gloves by healthcare workers and comparison with perceptions of student nurses. J Infect Prevention 2017; 18(3): 123-132.
- B. L. Thompson et al, Handwashing and glove use in a long- term care facility. Infect Control Hospital Epidemiology 1997; 18: 97-103.
- G. M.L. Bearman et al, A controlled trial of universal gloving versus contact precautions for preventing the transmission of multi-drug resistant organisms. Am J Infection Control 2007; 35(10): 650-655.
- C. Fuller et al, “The Dirty Hand in the Latex Glove”: A Study of Hand Hygiene Compliance When Gloves Are Worn. Infect Control Hospital Epidemiology 2011; 32(12): 1194-1199.
- G. Moore et al, The effect of glove material upon the transfer of methicillin- resistant Staphylococcus aureus to and from a gloved hand. Am J Infect Control 2013; 41: 19-23.
- J. Wilson et al, The misuse of clinical gloves: risk of cross-infection and factors influencing the decision of healthcare workers to wear gloves. Antimicrobial Resistance and Infection Control 2013; 2 (Suppl 1): 03.
- H. P. Loveday et al, Clinical glove use: healthcare workers actions and perceptions. J Hospital Infect 2014; 86:110-116.
- K. A. Hughes et al, Bacterial contamination of unused, disposable non-sterile gloves on a hospital orthopaedic ward. Australian Medical J 2013; 6(6): 331-338.
- J. B. Luckey et al, Bacterial count comparisons on examination gloves from freshly opened boxes and from examination gloves before treatment versus after dental dam isolation. J Endodontics 2006; 32: 646-648.
- A. Tenorio et al, Effectiveness of gloves in the prevention of hand carriage of vancomycin-resistant Enterococcus species by healthcare workers after patient care. Clinical Infect Diseases 2001; 32: 826-829.
- J. E. Patterson et al, Association of contaminated gloves with transmission of Acinetobacter calcoaceticus var. anitratus in an intensive care unit. Am J Med 1991; 91: 479-483.
- S. Lund et al, Reality of glove use and handwashing in a community hospital. Am J Infection Control 1994; 22: 352-357.
- Occupational Safety and Health Administration, Health Care Wide Hazards. Available at: https://www.osha.gov/SLTC/etools/hospital/hazards/univprec/univ.html
- T-H. Jang et al, Focus Group Study of Hand Hygiene Practice among Healthcare Workers in a Teaching Hospital in Toronto, Canada. Infection Control Hospital Epidemiology 2010; 31(2): 144-150.
Acknowledgement
The author wishes to acknowledge Dr. Jennie Wilson who kindly provided access to a number of the articles referenced in this paper.
About the Author
 John Hardie, BDS, MSc, PhD, FRCDC – Although retired from practice Dr. Hardie maintains a thirty plus years interest in the discipline of infection control as it relates to dentistry. He has published extensively on the subject and has lectured on it and related subjects throughout North America and in the UK, Europe, the Middle and Far East.
John Hardie, BDS, MSc, PhD, FRCDC – Although retired from practice Dr. Hardie maintains a thirty plus years interest in the discipline of infection control as it relates to dentistry. He has published extensively on the subject and has lectured on it and related subjects throughout North America and in the UK, Europe, the Middle and Far East.
RELATED ARTICLE: Surveillance: The Foundation of Effective Infection Prevention and Control












