The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions has recommended adopting the term “periodontal phenotype” instead of “gingival biotype” by the dental community.1 This term is based on both gingival phenotype (gingival thickness [GT] and keratinized tissue width [KTW]) and bone morphotype (thickness of the facial and/or buccal bone plate).2 Environmental factors and clinical interventions such as overhanging restorations, orthodontics, or gingival grafting procedures can modify the periodontal phenotype.1
It is estimated that 75% of the population has some degree of malocclusion.3 With the advent of clear aligners making orthodontic therapy more accessible, more and more people are receiving orthodontic treatments. However, we cannot ignore that tooth movement, and the periodontium have a dynamic and co-dependent relationship.4 It has been reported that about 20- 35% of patients may develop facial gingival recession (GR) 2 to 5 years after orthodontic treatment.5 According to an American Academy of Periodontology (AAP) consensus report, a higher incidence of bony dehiscence and GR could be observed in teeth surrounded by thin periodontal phenotypes or if orthodontic forces were applied to move dentition outside of the alveolar process, such as arch expansion.6 Therefore, it is essential to carefully assess dentoalveolar bone and soft tissue conditions before tooth movement.7 Patients with higher risks of periodontal breakdown from orthodontic tooth movement may warrant phenotype modification therapy involving either soft or hard and soft tissue augmentation.7
The AAP recommends performing gingival augmentation around teeth with less than 2mm of KTW or when significant labial movement is expected. Augmentation should also be done before any labial tooth movement in the presence of a thin periodontal phenotype.6 However, soft tissue augmentation alone will not cover bony dehiscence nor change the thickness of the buccal bone plate. Consequently, grafted sites may still experience GR after the end of orthodontic treatment. It has been reported that hard tissue augmentation provides clinical benefits such as preventing GR8, increasing KTW9, enhancing facial bone thickness10, expanding the scope of safe tooth movement4 and decreasing relapse of orthodontic treatment.11
When should we perform a soft tissue augmentation?
- With <2mm KTW
- If the tooth is expected to have significant labial tooth movement
- Thin periodontal phenotype with labial tooth movement
Case presentation
A 63-year-old female patient with no contributing medical history and an allergy to penicillin was referred by her orthodontist for periodontal evaluation before starting her orthodontic treatment. Upon examination, the patient displayed sufficient gingival thickness and KTW. However, she presented a fragile buccal bone plate on the facial side of her lower anterior teeth, with her roots showing transparency through her buccal mucosa. (Fig. 1A) The patient had only minor crowding. However, labial tooth movement was planned to align her teeth. Because of her orthodontic activities, we were concerned that her teeth would be moved outside the bony housing, creating GR and bony dehiscence.
Fig. 1A

We have decided to perform a hard tissue augmentation on her lower anterior sextant using a ribose cross-linked collagen scaffold (Dentsply, Charlotte, NC). This scaffold is 2mm thick and can ossify and maintain its integrity for up to 6 months. Upon full-thickness flap reflection, we observed a very thin layer of bone over the root prominences. (Fig. 1B) The ribose cross-linked collagen scaffold was stabilized over the buccal root surfaces using periosteal compression sutures, and tension-free closure of the flap was achieved.
Fig. 1B

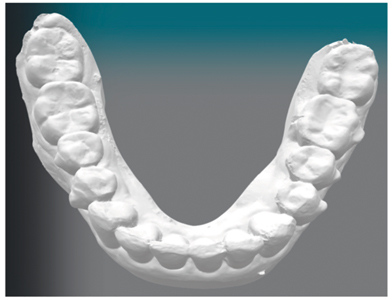
The patient was seen after 2-weeks and 4-months post-operatively (Figs 1C & 1D) and followed until the end of her orthodontic treatment. When comparing her pre-operative and 4-month post-operative pictures, we can appreciate an overall thicker periodontal phenotype, the roots can no longer be seen through the buccal mucosa, and a significant increase in KTW. (Fig. 2) Her orthodontic treatment was completed after 14 months, and a digital intra-oral scan was obtained, demonstrating a thicker volume on the buccal of her lower anterior teeth. (Fig. 3)
Fig. 1C

Fig. 1D

Fig. 2A
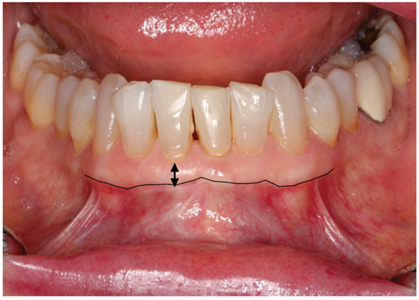
Fig. 2B

Fig. 3A

Fig. 3B
Conclusion
Periodontal phenotype plays a crucial role in the stability and maintenance of periodontal health for patients receiving orthodontic therapy. Thus, it is essential to carefully assess dentoalveolar bone and soft tissue conditions before tooth movement. Patients with a higher risk of periodontal breakdown from orthodontic treatment may benefit from phenotype modification therapies. Soft tissue augmentation alone may not prevent bony dehiscence and fenestration. Based on currently available evidence in the scientific literature, hard tissue augmentation appears to be a promising alternative which provides clinical benefits such as preventing GR, increasing KTW, enhancing facial bone thickness, and expanding the scope of safe tooth movement.
Oral Health welcomes this original article.
References
- Jepsen S, Caton JG, Albandar JM, et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol. 2018;89(Suppl 1):S237-S248.
- Kim DM, Bassir SH, Nguyen TT. Effect of gingival phenotype on the maintenance of periodontal health: an American Academy of Periodontology best evidence review. J Periodontol. 2020;00:1-28.
- Proffit WR, Fields HW, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult ORthodon Orthognath Surg. 1998;13(2):97-106.
- Wang CW, Yu SH, Mandelaris GA, Wang HL. Is periodontal phenotype modification therapy beneficial for patients receiving orthodontic treatment? An American Academy of Periodontology best evidence review. J Periodontol. 2020;91:299-310.
- Renkema AM, Fudalej PS, Renkema A. Kiekens R, Katsaros C. Development of labial gingival recessions in orthodontically treated patients. Am J Orthod Dentofacial Orthop. 2013;143:206-212.
- Kim DM, Neiva R. Periodontal soft tissue non-root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(Suppl 2):S56-S72.
- Johal A, Katsaros C, Kiliaridis S, et al. State of the science on controversial topics: orthodontic therapy and gingival recession (a report of the Angle Society of Europe 2013 meeting). Prog Orthod. 2013;14:16.
- Bahammam MA. Effectiveness of bovine-derived xenograft versus bioactive glass with periodontally accelerated osteogenic orthodontics in adults: a randomized, controlled clinical trial. BMC Oral Health. 2016;16:126-135.
- Wilcko MT, Ferguson DJ, Makki L, Wilcko WM. Keratinized gingiva height increases after alveolar corticotomy and augmentation bone grafting. J Periodontol. 2015;86:1107-1115.
- Brugnami F, Caiazzo A, Mehra P. Can corticotomy (with or without bone grafting) expand the limits of safe orthodontic therapy? J Oral Biol Craniofac Res. 2018;8:1-6.
- Makki L, Ferguson DJ, Wilcko MT, et al. Mandibular irregularity index stability following alveolar corticotomy and grafting: a 10-year preliminary study. Angle Orthod. 2015;85:743-749.
About the Author

Dr. Thomas Nguyen is the Associate Director of the Division of Periodontics at the McGill Faculty of Dental Medicine and Oral Health Sciences, Montreal, QC, Canada. He is a Fellow of the Royal College of Dentists of Canada and a Diplomate of the American Board of Periodontology. Dr. Nguyen is based in Montreal and maintains a practice limited to periodontology and implant dentistry.