
Dentists are constantly challenged in clinical practice to make decisions about whether to save or extract compromised teeth. Crown lengthening and orthodontic extrusion are techniques that have been used to provide restorations with improved longevity.1 Crown lengthening establishes a healthy relationship of the restoration to the periodontium by maintaining the biologic width. However, the procedure is considered less conservative as it sacrifices the supporting bone, alters crown by root ratio unfavorably and may lead to bone loss in adjacent teeth.2,3 The technique of forced orthodontic extrusion was first described in 1973 for the restoration of endodontically treated teeth with transverse root fractures to create a favorable relationship of the remaining root fragment with its associated periodontal tissues.4 It is considered a physiologically appropriate treatment as it reestablishes biological width, maintains gingival architecture and preserves all adjacent periodontal tissues.5 This procedure has also been referred to as ‘guided orthodontic regeneration’, ‘orthodontic extrusive remodelling’, ‘orthodontic extraction’ or ‘forced eruption’.6,7
Orthodontic Extrusion
More recently orthodontic extrusion is being utilized for implant site development to improve esthetic and functional outcomes with immediate implant placement. Tooth extraction is inevitably followed by hard and soft tissue loss which compromises the esthetic result especially in the anterior segment. Hard and soft tissue augmentation procedures before, during or after implant placement are not always predictable.7 Extrusion of teeth is preferred over hard and soft tissue augmentation for implant site preparation as it avoids creation of a new surgical site while stimulating viable mesenchymal stem cells to differentiate into osteoblasts, adipocytes and other periodontal ligament cells with regenerative potential.8 Moreover it can be used to modify soft tissue morphology with an increase in keratinized gingiva,9 which can improve the aesthetic result of the final prosthetic restoration.10 The amount of extrusion and force applied are dependent upon the tooth to be extruded and the amount of bone and soft tissue development required. Light forces have been recommended in periodontally compromised teeth. The rate of tooth movement must be slow to prevent ankylosis which would otherwise complicate extraction of the extruded tooth. A systematic review on the orthodontic extrusion found that the total treatment time and force applied were variable across selected literature. However it was concluded that to allow for simultaneous bone and soft tissue displacement, light and constant extrusive forces should not exceed 15g for anterior teeth and 50g for posterior teeth. However, depending upon root length and morphology and the density of the surrounding bone, the force required for extrusion may be up to 75g.11
In a clinical study, Amato et al reported on the biological behaviour of periodontal tissues and clinical outcomes during orthodontic extrusion. The results demonstrated that during tooth extrusion, new bone level formation to vertical tooth movement ratio is approximately 70% and that the amount of regenerated bone is not related to the original attachment levels. This finding suggests that that the attachment levels and amount of residual bone is not a limiting factor for success. The technique is invaluable when considering replacing hopeless teeth with a stable but reduced periodontium with dental implants.7
On the other hand, there appears to be greater variability with the amount of soft tissue regenerated and changes to the gingival margin, papilla, mucogingival junction (MGJ) and keratinized gingiva. In the study described above it was demonstrated that overall, the ratio of coronal growth of the gingival margin to vertical tooth movement was shown to be 65%. In cases where the gingival margin was at the bony crestal margin, the gingival migration was proportional to the orthodontic tooth movement. Some cases demonstrated gingival hyperplasia and others displayed negligible coronal movement of the gingiva proportional to the size of the preexisting periodontal pocket. In addition, some teeth adjacent to the extruded teeth demonstrated coronal gingival growth termed the ‘blanket effect’. Other soft tissue changes included coronal movement of the gingival papilla and a biotype conversion marked by an increased thickness of the gingiva on the buccal side. The MGJ showed variable responses based on its relation to the root, the supporting tissues and the presence of keratinized gingiva. For instance, if the MGJ was strongly attached to the root, the MGJ demonstrated coronal movement along with the gingival margin whereas if it was attached apical to the alveolar bone, only the gingival margin moved coronally resulting in an increased band of keratinized gingiva.7
Case #1
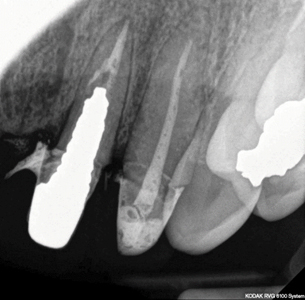
A 42 year old female presented with failed restorative treatment on teeth 21 and 22. The margins of the existing temporary crown on tooth 21, had invaded the biologic width with bleeding on probing, gingival recession, minimal attached gingiva, granulation tissue over exposed bone and mesio-angular bone defect (Figs. 1,2,3). Tooth 21 had a large post and core with a possible root fracture and grade 1.5mobility (Fig. 4). Retreatment of 21 was deemed to have a poor prognosis and extraction was indicated. The options for replacement were discussed and the patient chose an implant supported crown. Prior to extraction diagnostic records indicated a high smile line that created an esthetic challenge given the loss of hard and soft tissue. The gingival margins of 11 and 21 were asymmetrical and it was determined that following tooth extraction, the existing bony defect on 21 would increase the asymmetry as a result of alveolar resorption. The option of orthodontic extrusion prior to extraction to regenerate hard and soft tissue was discussed, along with the risk of post fracture during the extrusion process as a possible complication. Alternative treatment options such as bone and soft tissue augmentation or distraction osteogenesis was also discussed as part of the informed consent process. The prognosis for 22 was guarded, but it was decided that it was safer to retain tooth 22 than risk loss of the valuable interdental papilla between 21 and 22 if both teeth were extracted simultaneously.
Fig. 1

Fig. 2

Fig. 3

Fig. 4
The orthodontic treatment objective was to extrude roots of teeth 21 and 22 to regenerate bone and soft tissue prior to extraction and implant placement. Initial pretreatment records were completed and fixed mechanotherapy using ceramic twin brackets (MBT 022® prescription) was initiated. Brackets were bonded on to the temporary crowns on 21,22 and positioned 3 mm gingival to the centre point to facilitate extrusion (Fig. 5). Very light extrusion force was applied using .016 SPEED NITI® supercable wire, which permits tooth extrusion while allowing for the supporting alveolar bone to regenerate during the process. A total of 3-4 mm extrusion was achieved over the course of 8 -12 months. The incisal edges of the temporary crowns were reduced at each 6 weekly visit during the treatment duration. Once adequate bone was regenerated as confirmed by clinical evaluation and radiographs, the teeth were stabilized for a period of 6 months using a rigid 16/22 stainless steel wire (Fig. 6).
Fig. 5

Fig. 6

Tooth 21 was extracted and a Replace Select®13mm RP implant placed immediately. Primary stability was obtained at surgery, therefore an index was created and a screw retained crown temporary inserted the next day (Fig. 7). After 4 months of healing the 22 was restored with a porcelain bonded to metal crown and the 21 implant was restored with a screw retained porcelain fused to metal restoration (Fig. 8,9). Occlusion was checked to ensure clearance in centric occlusion and freedom in protrusion and lateral excursions. At treatment completion, the teeth were stabilized using a lingual bonded retainer for teeth 11,21 and Essix retainer for the upper arch.
Fig. 7

Fig. 8

Fig. 9

Orthodontic Intrusion
Replacement of missing teeth is crucial to avoid the supraeruption of opposing teeth into the edentulous space. Over erupted posterior teeth can complicate the restoration of implants due to space limitations. The minimum amount of space required to accommodate a screw retained prosthetic restoration from the head of the implant to the occlusal surface of the opposing tooth is 4-5mm for a screw retained prosthesis restored at implant level and up to 7.5mm for a screw retained prosthesis at abutment level. The latter number for a cement retained restoration is slightly less than 7.5mm.12 Space can be regained by occlusal reshaping of the opposing teeth with the risk of iatrogenically induced sensitivity. Surgical techniques such as assisted impaction using corticotomy or lateral maxillary segmental osteotomy followed by apical repositioning of the bony fragment have been utilized. Other techniques to regain space are endodontic treatment followed by coronal reduction and orthodontic intrusion.13
Tooth movement in intrusion occurs by resorption of the underlying bone and by bone deposition along the middle and coronal third of the root, due to stretching of periodontal fibres. The process requires the application of light forces concentrated over a small area and to prevent apical resorption should be carried out only for a limited period. Intrusion of multirooted teeth is a difficult process and is restricted by amount of anchorage available. The amenability of the technique depends on the amount of force exerted and direction and this declines as the individual ages. Light forces are known to preserve marginal bone while heavy forces may lead to root resorption. Additionally, negative forces generated on the adjacent tissues by these intrusive forces leads to a slight increase in bucco lingual width of the alveolar bone. Increased osteoclastic activity has been noted in patients with inflammation in the periodontal supporting tissue. To reduce the risk of marginal bone loss optimum oral hygiene must be maintained by the patient during the orthodontic treatment.14
Temporary anchorage devices (TADs) are minimally invasive and aid in molar intrusion with maximal patient comfort and minimal patient compliance.15 TADs are made of Ti alloy and are typically 6-12 mm in length and 1.2-2mm in diameter. These are placed in areas between teeth with dense cortical bone using a hand driver under local anesthetic. TADs are broadly categorised into self tapping (Conical cross section) and self driving (corkscrew cross section). The considerations for using TADs include location of the device, angulation of placement and loading forces. These are placed at a particular angle (ex maxillary posterior region at 30-45 degrees), using a defined amount of loading force (100-200 g) and at a particular location (ex between maxillary 2nd premolar and first molar). A single TAD may be used in conjunction with fixed orthodontic therapy, or 2 TADS may be used with elastics to help intrude a tooth. When used with slow controlled movements the potential for apical root resorption decreases.
Case #2
A 40 year old female patient presented to our practice with severely decayed teeth 36,37,38,48 with wanting options for treatment. An examination revealed that teeth 46 and 47 were root canal treated with inadequate ferrule (Figs.1,2). Teeth 36 and 37 were root canal treated, decayed, demonstrated inadequate ferrule and insufficient room for coronal restorations. The treatment plan included extraction of 36,37,38,48, crown lengthening of 46,47 followed by full coverage ceramic restorations and replacement of the missing 36,37 teeth with the dental implants. The concern however was the inadequate interocclusal space available for fixed implant restorations due to overeruption of 26, 27 and 28 (Fig.3). The patient accepted the option of intrusion of these teeth with fixed orthodontic treatment prior to replacement of the missing teeth.
Fig. 1

Fig. 2

Fig. 3

Sectional fixed appliances were placed on teeth number 24,25,26,27,28. Initial levelling was achieved using around round 016 NiTi wires followed by rigid 17/25 SS wire. A 10 mm TAD (Tomas® miniscrew) was inserted into infrazygomatic region above the 26-27 region and active intrusion of the posterior teeth was started using light elastic ligature forces (Fig.4). A total of 3mm of intrusion of the posterior teeth was achieved over a course of 6-9 months.
Fig. 4

However, some side effects such as buccal tipping of the posterior teeth was noticed, as well as slight intrusion of teeth 24 and 25, which were initially in occlusion with the lower teeth. A palatally placed second TAD would have resolved this issue but the patient refused palatal placement of the TAD due to a strong gag reflex. Therefore, step down bends were placed in the wire to bring 24-25 back into occlusion and increased lingual torque was placed in the posterior section to torque the molars. Once the optimal position was achieved, the TAD screw was removed and intruded teeth (26-27-28) were stabilized using a heavy rectangular 17/25 SS wire.
Teeth 36 and 37 were extracted atraumatically keeping the sockets intact. The sockets were grafted with BioOss® collagen and covered with Mucograft®Seal and closed with 5-0 monocryl continuous sutures. Seven months later, osteotomies were prepared for Biohorizons® 5.2×9 mm (4.5 mm platform) Tapered Pro fixtures placed with excellent primary stability. BioOss® collagen was used to graft the buccal surface on the 36 implant. Following a healing period of 6 months, the implants were restored with a screw retained splinted restoration (Fig. 5,6,7).
Fig. 5
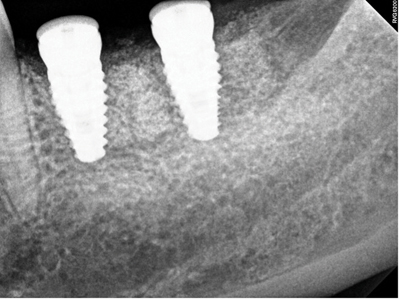
Fig. 6
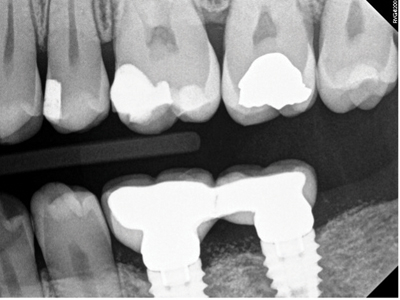
Fig. 7

Final detailing of occlusion was done using a soft, twisted rectangular wire to ensure proper occlusion with the lower teeth. Once the teeth were in good occlusion, the fixed appliance was debonded (Figs. 8, 9) and a full arch Essix retainer was delivered for retention purposes for the patient to wear at nighttime. After the prosthodontic treatment, the patient opted to go with clear aligner treatment for lower incisor rotation correction which was achieved over 6 months, and the correction was retained using a fixed lingual retainer and an overlay Essix retainer.
Fig. 8

Fig. 9

Discussion
Orthodontic extrusion is not without its limitations and disadvantages. The binomial force-time is site specific. During vertical tooth movement, the elimination of occlusal interferences requires substantial tooth reduction, which could cause sensitivity and/or pulp exposure. The total treatment time requirement of 9–18 months, depending on the severity of the bone and soft tissue defect in the site may be a deterrent to people looking for quick results.16 Meticulous follow up is required to monitor for the desired outcome and minimize complications. It is also important to note that orthodontic extrusion for the purpose of implant site development does not allow for reorganization of supracrestal fibres because it does not involve a supracrestal fibrotomy and therefore requires a longer stabilization period to reestablish the sulcus and keratinization of soft tissue.9
Orthodontic intrusion carries the risk of root resorption leading to a poor crown to root ratio. It has been postulated that the magnitude of intrusive forces is more closely associated with root shortening than the amount of intrusion desired. Genetic predisposition, presence of periodontal diseases and previous history of trauma may worsen this condition. Light controlled forces have been shown to minimise this risk. Most resorption lacunae undergo repair once the intrusive forces are withdrawn. However, breakdown of marginal bone has also been reported in cases with suboptimal oral hygiene maintenance.14
TAD use carries several risks such as relapse of tooth position, root damage and loss of tooth vitality. If the damage to the root surface is minor the surface will self heal in 3-4 months. Inaccurate positioning of the TAD can lead to several problems. If it is placed in the soft tissue, it may lead to ulceration or tissue overgrowth. If placed on the palate in the region of the 2nd or third molar it may damage the greater palatine nerve as it exits its foramen. Perforation into the maxillary sinus can be asymptomatic ( if < 2mm) or lead to sinusitis and chronic oroantral fistula depending on the size of the perforation. The stability of the TAD is generally unaffected in these cases. However, If the placement site lacks cortical bone or there is excessive loading of intrusive forces this may lead to loosening of the implant and its subsequent failure.14
Careful treatment planning and meticulous follow up helps overcome the limitations of the techniques described. Overall, the methods demonstrate the benefits of interdisciplinary treatment to achieve stable and long lasting prosthodontic results.
Oral Health welcomes this original article.
References
- Cordaro M, Staderini E, Torsello F, Grande NM, Turchi M, Cordaro M. Orthodontic Extrusion vs. Surgical Extrusion to Rehabilitate Severely Damaged Teeth: A Literature Review. Int J Environ Res Public Health. 2021;18(18).
- Planciunas L, Puriene A, Mackeviciene G. Surgical lengthening of the clinical tooth crown. Stomatologija. 2006;8(3):88-95.
- Smidt A, Lachish-Tandlich M, Venezia E. Orthodontic extrusion of an extensively broken down anterior tooth: a clinical report. Quintessence Int. 2005;36(2):89-95.
- Heithersay GS. Combined endodontic-orthodontic treatment of transverse root fractures in the region of the alveolar crest. Oral Surg Oral Med Oral Pathol. 1973;36(3):404-15.
- Krastl G, Filippi A, Zitzmann NU, Walter C, Weiger R. Current aspects of restoring traumatically fractured teeth. Eur J Esthet Dent. 2011;6(2):124-41.
- Paolone MG, Kaitsas R. Orthodontic-periodontal interactions: Orthodontic extrusion in interdisciplinary regenerative treatments. Int Orthod. 2018;16(2):217-45.
- Amato F, Mirabella AD, Macca U, Tarnow DP. Implant site development by orthodontic forced extraction: a preliminary study. Int J Oral Maxillofac Implants. 2012;27(2):411-20.
- Nagatomo K, Komaki M, Sekiya I, Sakaguchi Y, Noguchi K, Oda S, et al. Stem cell properties of human periodontal ligament cells. Journal of periodontal research. 2006;41(4):303-10.
- González-Martín O, Solano-Hernandez B, González-Martín A, Avila-Ortiz G. Orthodontic Extrusion: Guidelines for Contemporary Clinical Practice. Int J Periodontics Restorative Dent. 2020;40(5):667-76.
- Addy LD, Durning P, Thomas MB, McLaughlin WS. Orthodontic extrusion: an interdisciplinary approach to patient management. Dent Update. 2009;36(4):212-4, 7-8.
- Korayem M, Flores-Mir C, Nassar U, Olfert K. Implant site development by orthodontic extrusion. A systematic review. Angle Orthod. 2008;78(4):752-60.
- Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695-706.
- Manea A, Dinu C, Băciuţ M, Buduru S, Almășan O. Intrusion of Maxillary Posterior Teeth by Skeletal Anchorage: A Systematic Review and Case Report with Thin Alveolar Biotype. J Clin Med. 2022;11(13).
- Antoun JS, Mei L, Gibbs K, Farella M. Effect of orthodontic treatment on the periodontal tissues. Periodontol 2000. 2017;74(1):140-57.
- Kravitz ND, Kusnoto B, Tsay TP, Hohlt WF. The use of temporary anchorage devices for molar intrusion. J Am Dent Assoc. 2007;138(1):56-64.
- Andreasen JO, Andreasen FM, Andersson L. Orthodontic Management of the Traumatized Dentition. United Kingdom: John Wiley & Sons, Incorporated; 2018.
About the Authors

Dr. Neena D’Souza is an adjunct professor at the University of Toronto Faculty of Dentistry, actively involved in clinical research. She is an instructor in the graduate prosthodontic program and has a private practice at Mississauga Dental Specialists.

Dr. Girish Deshpande is the past president of the Ontario Association of Orthodontists and the Ontario director for the Great Lakes Association of Orthodontists. He is a clinical instructor at the University of Toronto, Faculty of Dentistry and has a private practice at GD Orthodontics and Mississauga Dental Specialists in Mississauga, ON.

Dr. Neha Sisodia is a third-year dental student at the University of Toronto.









