
Surgical protocols for osseointegrated implant placement have evolved significantly over time. It was not so long ago that the standard practice for implant surgeons was to place implants ‘where the bone was’ and let the restoring dentist deal with the myriad prosthetic problems this often created. In the early days of implants, this surgical paradigm was perfectly reasonable as everyone appreciated that without enough bone around an implant, osseointegration would be impaired and the implant was doomed to fail. This deeply flawed approach was eventually replaced by a new paradigm of ‘prosthetically driven’ implant placement. This approach differs fundamentally in that it redefines how success is measured. By employing a more integrated methodology, practitioners could provide implant based solutions that fulfil both functional and aesthetic requirements. New generations of products and procedures have produced outcomes that are so reliable that we now talk about implant based rehabilitation lasting for decades. As desirable as this longevity is, it mandates case planning that takes into consideration age-related stomatognathic changes in both anatomy and function.
Long-term longitudinal studies of restored implants suggest that true failures (loss of the implant) are uncommon once secondary stability has been achieved, however, complications tend to increase with time. In a classic paper by Ekelund and colleagues, they note that the survival rate of mandibular implants in their study was 98.9% at 20 years.1 The success rate is slightly lower in the maxilla and systemic conditions such as diabetes mellitus and smoking can play a role in both implant survival and complication rate.2 Mechanical factors such as implant size and immediate loading do not significantly influence longevity. The take-away message is that implants typically don’t fail when surgery follows validated protocols. However, biological and mechanical complications associated with restored implants become more frequent and more significant as time passes.1
An awareness of expected age-related changes in the stomatognathic system and planning for the long-term, is the key to limiting complications. As dentists we are trained to treat a presenting condition without giving much thought to how the jaws will change over time. In the case of most dental restorations such as filings and single unit crowns, this approach is very acceptable. However, this is not the case for implants which are too often placed to meet short-term functional and esthetic needs and do not allow us to ‘adjust’ their position once integrated.
The Dynamic Oro-facial Complex
Developmentally and histologically, the alveolar processes are different from the basal bone that forms the structural foundation of the jaw bones. (Fig. 1) Both the mandible and maxilla develop from the first branchial arch which begins to differentiate at about day 24 of gestation.3 What is important to recognize is that the alveolar bone is developmentally and functionally part of the tooth bud and not the underlying mandible or maxilla.3 This is well demonstrated in conditions where tooth buds don’t develop such as ectodermal dysplasia. In these circumstances, there is a paucity of alveolar bone where no teeth develop. In areas where teeth have been lost there is a consequential atrophy of alveolar bone.4 This suggests ongoing signalling mediated by the periodontal ligament and surrounding bone which is more complicated than just a local response to bone loading.5 Secondary to the direct relationship between alveolar bone mass and teeth, there is a relatively consistent underlying pattern of osseous change seen throughout the lifespan.
Fig. 1

Bone turnover or ‘modeling’ is a life-long process which describes the functional relationship between osteoclasts and osteoblasts. The relative rate of skeletal bone deposition by osteoblasts versus bone removal by osteoclasts is influenced by many factors such as genetics, age, gender, nutrition, local and systemic disease, as well as mechanical stresses. In the jaws, bone modeling and remodeling can lead to a net loss or net gain of bone volume as well as changes in bone density. The volumetric change in the alveolar ridges is most significantly impacted by the presence or absence of teeth. However, the rate and degree of change is highly influenced by anatomic location and local disease processes such as periodontal disease. In the edentulous maxilla, the alveolar ridge resorbs in a vertical direction as well as resorbing towards the palate. This results in a thinner ridge of smaller circumference as an individual ages. In the edentulous mandible there is the same vertical loss, however, the horizontal loss is from the lingual creating a thin arch with a relatively wider inner circumference.6 The basal bone of the maxilla in the area of the sinuses becomes thinner due to ongoing pneumatisation of the maxillary antra but remains unchanged between the anterior antral wall and the piriform aperture.7 (Fig. 2) In longitudinal studies of the dentate and edentulous mandible, Xie and colleagues found that the basal bone may actually increase in volume distal to the mental foramen with increasing age. New bone is laid down primarily on the inferior surface of the mandible creating the impression of the inferior alveolar nerve moving superiorly with age. This increase in volume is more pronounced in men than in women.7
Fig. 2
In tooth bearing areas of jaws, the pattern of functional local modeling with age is much different from edentulous jaws. There are changes to the boney architecture of the alveolar ridges as well as changes in the position of the ‘neutral zones’ (areas where forces of the tongue pushing outwards are balanced by the forces of the cheek and lip muscles pulling in) secondary to both hard and soft tissue changes with aging. Tooth eruption is an ongoing process throughout life. Even with skeletal maturity and opposing occlusion, teeth continue to erupt and with them, the alveolar ridge increases in vertical dimension. This is particularly evident in the maxilla of women.5,8,9 Longitudinal studies have clearly shown that with aging the lower face height increases primarily due to ongoing eruption of the anterior teeth. In males this is coupled with sagittal mandibular growth whereas in females there is a tendency for the mandible to rotate creating a more convex profile.10 These age-related skeletal changes can result in tooth-arch discrepancies and crowding.11 Accompanying these dentoalveolar and skeletal changes are soft tissue changes. These include a flatter lip profile as part of an increased nasolabial angle and a lower smile line.11,12
Submergence of Implants
Given the dynamic nature of the oro-facial complex, implant-supported restorations can be impacted both esthetically and functionally over an extended period of time. The esthetic issues commonly take two forms and are most evident in the maxillary anterior region. The first form is one of ‘submersion’, where the implant-borne restoration, which behaves much like an ankylosed tooth, will appear to be submerging relative to the adjacent natural teeth.13 As noted above, anterior teeth tend to continue to erupt throughout life creating a taller alveolar ridge leaving the implant position relatively more apical. (Fig. 3) This creates the impression that the implant borne restoration is too short. Studies suggest that this incisal edge asymmetry is more bothersome to the dentist than it is to the patient.14
Fig. 3

Gingival Recession
The second esthetic issue is loss of soft tissue leading to exposure of the crestal and facial aspects of the implant. Based on longitudinal studies, implant thread exposure rarely leads to implant failure and is generally considered a ‘biologic complication’.1 However, thread exposure can become an esthetic failure and usually leads to the need for increased long-term maintenance. The mechanism for this chain of events is typically multifactorial but begins with reduction of blood flow to the crestal aspect of the buccal cortex of the alveolar ridge. Jaw bone, like all other bone, receives blood flow from two main sources. The first is from perforating vessels that originate in the surrounding soft tissue and the second, internally through the Haversian system. Cancellous bone is relatively vascular and does not rely on soft tissue perfusion to the same degree as cortical bone. The cortical plate on the anterior and crestal aspects of the jaws is made of dense compact bone, which receives much of its vascular supply from the adherent soft tissue, specifically the periosteum.15 If this soft tissue is separated from the buccal plate during an extraction, such as raising a flap, the cortical bone becomes reliant on the internal vasculature. By replacing part of the cancellous bone with an implant, (particularly if the implant is placed directly adjacent to the cortex and even with the crest), the available blood flow is still further compromised which can result in early loss of the cortical plate. Since soft tissue such as gingiva follows bone, as the cortical plate resorbs from the crest where the blood flow is least abundant, the implant may become exposed.
A similar phenomenon can occur much later through a different mechanism based on anatomical changes seen in aging. There is a tendency over time for both mandibular and maxillary anterior teeth to move lingually and palatally as the neutral zones shift with changes in hard and soft tissue in the lower face. The teeth follow the neutral zones but implants devoid of a periodontal ligament cannot. As the alveolar ridge subtly migrates with the teeth, it can lead to resorption of the buccal plate over the facial aspect of an implant, resulting in a reduction in soft tissue coverage at the crest. It has been argued that the presence of functional implants will prevent or at least minimize the atrophy of the surrounding alveolar bone. The literature is inconclusive with respect to this concept as most supporting studies describe implants in the posterior arch adjacent to natural teeth. There is, however, strong support that a physiologically loaded implant regardless of location will limit age related loss of bone mineral content.16,17 In general, anterior implants, particularly in the maxilla, are prone to both hard and soft tissue loss on the facial aspect over time.13
Loss of Contact
A further potential problem arises in response to sagittal changes in the supporting bone and centripetal shifting of the neutral zones. The relative position of natural teeth within the dental arch is influenced by a number of forces which define a ‘neutral zone’. Also referred to as the ‘zone of equilibrium’, it is the area where the inward forces of the lips and masticatory muscles are offset by the protrusive forces generated by the tongue.18 This zone moves with age, initially as part of the growth pattern of the young skeleton and later in life as a function of age-related anatomic changes. As the neutral zone moves, so does the natural dentition, but not osseointegrated implants. This can lead to a loss of interproximal contact in addition to the previously described relative malocclusion or crowding of the natural teeth.19 Growth and age related ‘disequilibrium’ creating dynamic neutral zones is the most common cause of orthodontic relapse which is mitigated through long-term retention.20 These principles are not generally applied in implant dentistry as we think of the dentition as ‘stable’ in skeletally mature individuals.
Adaptive Implant Placement
To compensate for the dynamic nature of the jaws and static properties of implants, an adaptive approach to implant placement can help to reduce or eliminate many of the problematic issues experienced in long-standing implant cases.
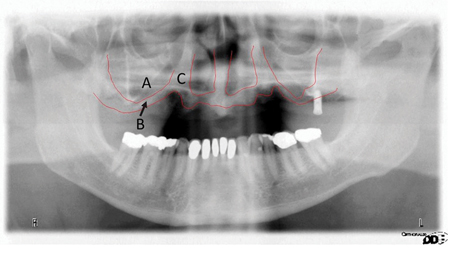
Two approaches to implant placement should be considered. The first is to choose an implant placement site in anticipation of expected anatomic changes over time. As noted, in the maxilla there is an age-dependent remodelling of the ridge towards the palate. Therefore an implant should ideally be placed in a more palatal position, particularly in the esthetic zone. This will not only allow for the option of a screw-retained restoration but also reduce the likelihood of labial bone and soft tissue loss as the ridge moves palatally over time. (Fig. 4)
Fig. 4
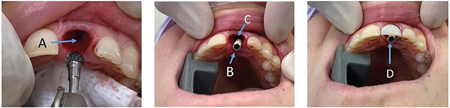
A second consideration, particularly in edentulous jaws is, to place implants into basal bone as opposed to any remaining alveolar bone. Without the presence of natural teeth and their periodontium, alveolar bone resorbs, which can leave implants that were placed at the crest of the ridge, with a considerable thread exposure. This exposure may not affect the stability of the implant but can create significant hygiene and esthetic problems particularly in full arch reconstructions. (Fig. 5)
Fig. 5
Screw Retained Restorations
Another strategy that should be considered for implants that are immediately placed and temporized with or without loading is the use of screw retention for restorations. Choosing to use cement or a screw to retain a restoration is based on a number of factors, many of which are aimed at solving short-term problems. According to Shashid, the strongest argument for cementing a restoration is either the perceived freedom to place implants in non-ideal positions or to deal with implants that were placed in a compromised position.21 All too often the alveolar ridge in the esthetic zone is thin and an implant is placed to maximize available bone support at the expense of ideal placement. Similarly, placing an immediate implant in the centre of a fresh anterior extraction socket will often lead to an implant that is too buccal. For esthetic reasons, it is critical to not have a screw channel emerge from the facial or incisal surfaces of a restoration. Using cement to retain a restoration mitigates this problem for many practitioners.
Other considerations that have historically motivated practitioners to choose the cemented option include cost, number of components (such as the retention screw), ease of access and reliable retention.21However, over the course of the past decade the wide use of CAD/CAM technology and angled screw-retained abutments allow for off-axis correction of up to 25 degrees with fewer, less expensive components. These abutments can often solve the problem of the poorly placed anterior implant or a tilted posterior implant by prescribing specifically designed abutment screws and novel accompanying drivers. Many practitioners cite difficulties placing and torqueing a retention screw in a small mouth or one with limited opening. Again, recently developed armamentarium in the form of a 90 degree variable torque driver can make placing and removing retention screws fast and safe. Arguments have also been made that a screw retained prosthesis is more likely to come loose than a cemented one. This is generally true, particularly if the restoration is not seated well during placement. With the emphasis on an ideal emergence profile in the esthetic zone, deeper implant placement can create interferences between the restoration and surrounding bone leading to incomplete seating of the restoration. As the bone undergoes remodelling, the screw retained restoration is more likely to become loose and require tightening of the retention screw.
Although most of the supportive arguments for choosing to cement a restoration are valid in the short term, they do not consider physiologic and anatomic changes in the long-term. Esthetic zone restorations are ideally placed with subgingival margins to enhance emergence profile and soft tissue contours. However, the deeper the margin, the more difficult it is to remove extruded cement. Even a small amount of cement can cause crestal bone loss and subsequent soft tissue loss. Sailer’s review of the literature comparing screw-retained and cemented restorations revealed that biologic complications at 5 years such as bone loss greater than 2 mm, were significantly higher in the cement retained group.22
Possibly the most important attribute of the screw-retained restoration is the ability to remove the restoration. In the short term, the ability to easily remove a restoration allows for immediate provisionalization of implants as well as modification of colour and shape. In the long term a removable restoration can be modified to re-establish interproximal contact that is lost through the centripetal movement of the natural teeth around it. Similarly, relative submergence of the implant over time as a function of the ongoing eruption of the adjacent teeth can be corrected if the restoration is screw retained. With a cemented restoration, there are no work-arounds for these situations that are not costly and invasive.
Conclusions
Given the longevity of implant supported restorations and the dynamic changes that the jaws and facial soft tissues go through as we age, an adaptive approach to implant placement can minimize the potential for future biologic, mechanical and esthetic problems. In summary, implants should be placed with forethought as to where the bone and soft tissue will be in the future. In the maxillary esthetic zone, the bone and corresponding neutral zone will move palatally. Ideal implant placement would therefore favour a more palatal placement rather than centered in the current alveolar ridge. When placing implants in areas where there are few remaining teeth or where full arch reconstruction is being undertaken, it is reasonable to expect any existing alveolar ridge to eventually resorb. Clinicians should therefore make use of basal bone as much as possible. This will improve long-term esthetics and reduce the risk of biologic complications such as exposed threads. Finally, when possible, use screw retention for restorations. The ability to remove a restoration not only eliminates the risk that excess cement poses to hard and soft tissue, but allows for correction of the long-term sequelae of submergence and loss of contact.
Oral Health welcomes this original article.
References
- Ekelund JA , Lindquist LW, Carlsson GE, Jemt T.,Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. Nov-Dec 2003;16(6):602-8.
- Song S, Lee J, Um H, Chang B., Factors affecting the survival of implants: a long-term retrospective study. J Dent Rehabil Appl Sci 2015;31(1):10-9
- Moore K, Persaud T, Torchia M., The Developing Human–Clinically Oriented Embryology, 11th Edition, March 2019 Saunders, NY, NY.
- Balshi T., Wolfinger G., Treatment of Ectodermal Dysplasia with Zygomatic Implants: A case report. The International journal of oral & maxillofacial implants · March 2002:277 – 281.
- Jonassona G, Skoglunda I, Rythén M, The rise and fall of the alveolar process: Dependency of teeth and metabolic aspects. Archives of Oral Biology 2018;96:195–200
- Tallgren A, The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. J Prosthetic Dent. May 2003;89(5):427- 35.
- Xie Q, Wolf J, Soikkonen K, Ainamo A. Height of mandibular basal bone in dentate and edentulous subjects. Acta Odontol Scand. 1996 Dec;54(6):379-83.
- Thilander, B., Odman, J. and Jemt, T. Single Implants in the Upper Incisor Region and Their Relationship to the Adjacent Teeth. An 8-Year Follow-Up Study. Clinical Oral Implants Research, 1999;10:346-355.
- Thilander, B.. Dentoalveolar development in subjects with normal occlusion. A longitudinal study between the ages of 5 and 31 years. European Journal of Orthodontics, 2009;31:109–120.
- C.M. Forsberg, S. Eliasson, H.Westergren, Face height and tooth eruption in adults – a 20 year follow-up investigation, Eur. J. Orthod. 1991;13:249–254.
- Albert A, Ricanek K, Patterson E. A review of the literature on the aging adult skull and face: Implications for forensic science research and applications. Forensic Sci Int. 2007 Oct 2;172(1):1-9
- Sharma P, Arora A, Valiathan A, Age Changes of Jaws and Soft Tissue Profile. https://doi.org/10.1155/2014/301501
- Daftary F, Mahallati R, Bahat O, Sullivan R, Lifelong Craniofacial Growth and the Implications for Osseointegrated Implants. Int J Oral Maxillofac Implants 2012;28:163–169
- Andersson B, Bergenblock S, Fürst B, Jemt T, Long-Term Function of Single-Implant Restorations: A 17- to 19-Year Follow-Up Study on Implant Infraposition Related to the Shape of the Face and Patients’ Satisfaction. Clin Implant Dent Relat Res. 2013 Aug;15(4):471-80
- Chanavaz M, Anatomy and histophysiology of the periosteum: quantification of the periosteal blood supply to the adjacent bone with 85Sr and gamma spectrometry. J Oral Implantology. 1994 Dec; 21(3):214-219
- von Wowern N, Gotfredsen K, Implant-supported overdentures, a prevention of bone loss in edentulous mandibles? A 5-year follow-up study. Clin Oral Implants Res. 2001 Feb;12(1):19-25.
- Oh T, Yoon J, Misch C, Wang H, The Causes of Early Implant Bone Loss: Myth or Science? J Periodontol. March 2002;73(3):322-333
- Srivastava V, Gupta NK, Tandan A, et al. The Neutral Zone: Concept and Technique. J Orofac Res. 2012;2(1):42-47
- Koori H, Morimoto K, Tsukiyama Y, Koyano K, Statistical analysis of the diachronic loss of interproximal contact between fixed implant prostheses and adjacent teeth. Int J Prosth. 2010;23(6):535-540
- Littlewood S, Kandasamy S, Huangk G, Retention and relapse in clinical practice. Australian Dental Journal 2017; 62:(1 Suppl): 51–57
- Shadid R, Sadaqa N, A Comparison Between Screw- and Cement-Retained Implant Prostheses – A Literature Review. J Oral Implantology. 2012;38(3):298-307
- Sailer I, Mühlemann S, Zwahlen M, Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res. 2012 Oct;23 Suppl 6:163-201
About the Authors

Dr. Brian Freund received his medical degree from McMaster University and received his dental and specialist training at the University of Toronto. He practices as an Oral and Maxillofacial Surgeon at the Chrysalis Dental Centre in Toronto with special interests in immediately loaded implant rehabilitation, neuromuscular dysfunction and minimally invasive facial rejuvenation.

Dr. Steven Bongard obtained his DDS degree from the University of Toronto Faculty of Dentistry. He is the founder and clinical head of Chrysalis Dental Centre in Toronto, a dental implant only facility focused on “same day” dental implant solutions. Dr. Bongard has extensive experience in implant placement, bone grafting procedures, as well as the prosthetic component of implant restoration.

Dr. Alex Bongard practices at the Chrysalis Dental Centre with extensive surgical and restorative experience in both full arch and single tooth implantology. He is passionate about simplified immediacy with a patient centered approach to overcoming treatment barriers.

Dr. John P. Zarb earned his DDS at the University of Detroit Mercy in 1995, followed by graduate prosthodontic training at the University of Toronto, earning his MSc in 2002. Dr. Zarb is a staff prosthodontist at Mt Sinai Hospital in Toronto and a Clinical Assistant Professor at the University of Rochester, Eastman Institute for Oral Health.









