
Orthognathic surgery (OGS), often referred to as “corrective jaw surgery,” involves complex three-dimensional analysis and movements of the maxilla, mandible, and chin. It includes a variety of procedures that can help manage malocclusion, a constricted airway, and esthetics.
Traditionally, OGS involved a clinical and surgical workup consisting of collecting several data points, performing a mock surgery, and then performing the same surgery in the operating room. Advances in technology have allowed us to move many of these steps from the analog to digital world, leading to faster, efficient clinical workups and more accurate surgery.1,2 This article will demonstrate these advances and present a modern, efficient protocol for working up and planning orthognathic cases.
The Clinical Exam
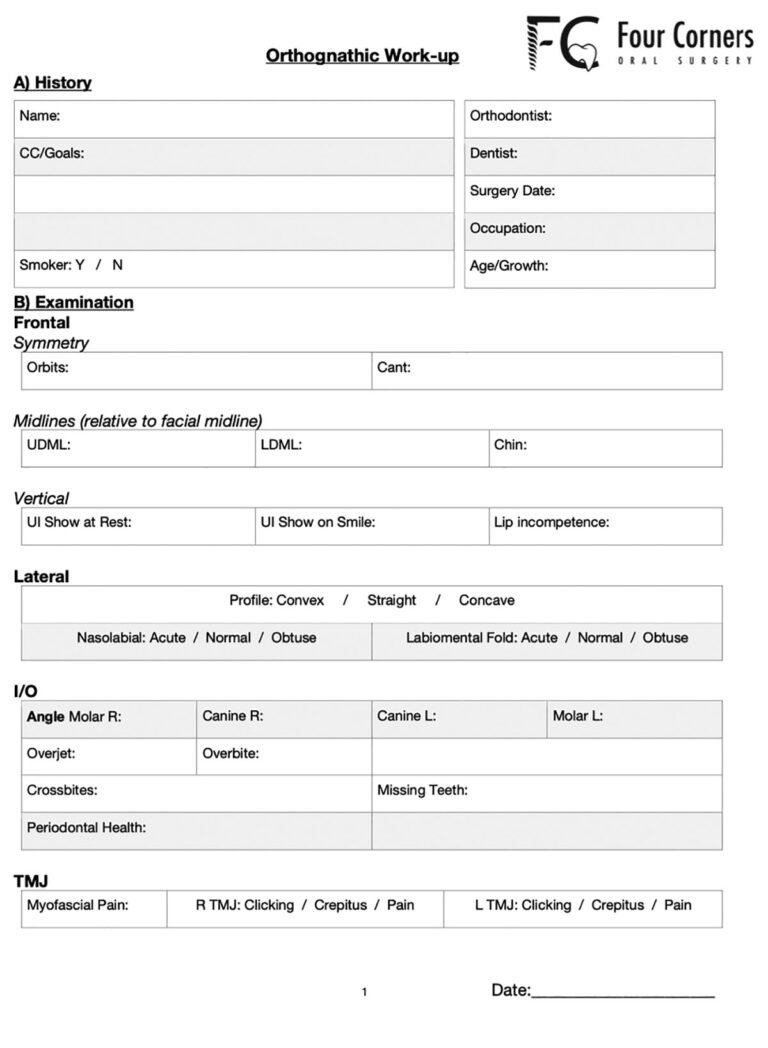
As technology advances, it is important to remember that the clinical exam and history remains the most important step in orthognathic planning. This is because certain measurements can only be taken reliably during the clinical exam, and dramatically affect the surgical plan that is created. In addition, the patient’s chief complaint regarding their occlusion, function, and esthetics helps guide which surgery and movements are most appropriate for them. After decades of orthognathic surgery, the clinical exam has stayed relatively constant and a standard workup should include, at a minimum, the following data points:
- Comprehensive medical history
- Chief complaint
- History of orthodontic treatment
- Age and growth status
- Facial asymmetry/cant
- Position of upper dental midline, lower dental midline, chin midline
- Maxillary incisal show at rest and on full smile
- Profile, nasal, and chin exam
- Overbite, overjet, missing teeth, periodontal health, Angle classification
- Myofascial pain or TMD symptoms
Although comprehensive, this data can be collected and summarized on a one-page exam sheet. (Fig. 1)
Fig. 1
Data Collection
In addition to the clinical exam, radiographs and dental model analysis are the cornerstone of OGS planning. A panoramic and lateral cephalometric radiograph are still used today and have transitioned to digital radiographs that can be analyzed, reproduced, and stored online. Dental models were traditionally taken with an alginate impression and are uncomfortable for the patient and prone to error in both the taking of the impression and pouring up the models.3 Intra-oral (IO) scanning technology has developed and digital IO impressions of the maxilla and mandible can now be taken in minutes and are extremely accurate.4 (Fig. 2) In addition, the impressions can be visualized immediately, and specific areas improved or redone. For surgeons utilizing virtual surgical planning, a medical grade CT scan was traditionally taken however the advent of cone-beam computed tomography (CBCT) has rendered this practice far less common. CBCTs can be taken in office, do not consume hospital or public resources, and expose the patient to as little as one tenth the level of radiation.5
Fig. 2A

Fig. 2B

The combination of these technological advances has resulted in a digital workflow for patients that can be done entirely in the office, beginning with a thorough clinical exam and proceeding to collection of a full skull CBCT and dental IO scans.
Surgical planning
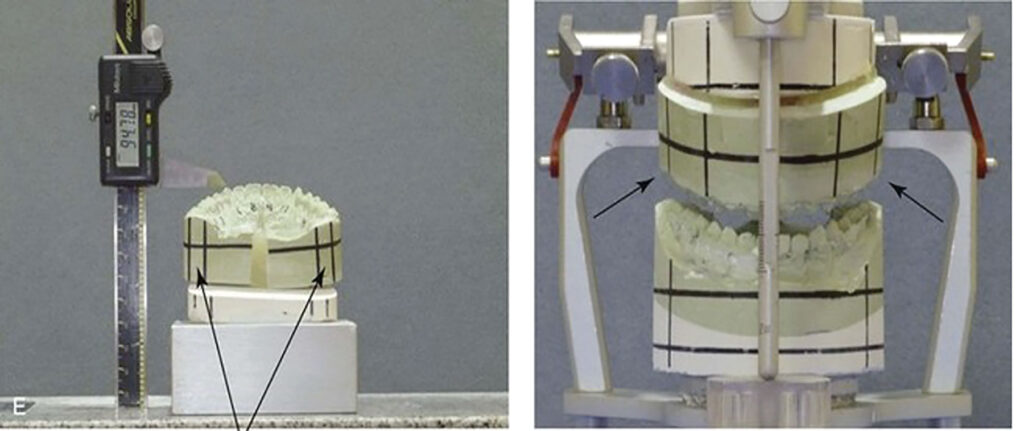
Although OGS has been around for decades, continued evolution in technology, digital surgical planning, and anesthesia have transformed the surgical workflow and improved outcomes. In single jaw cases, the maxilla OR mandible is moved and set into the final occlusion based on the reference of the opposing arch through fabrication of a splint. Prior to evolution of digital dentistry, isolated single jaw surgeries involved laboratory time with stone models fabricated from alginate impressions. These models were mounted on a Galetti articulator to haptically establish the desired occlusion followed by creation of an acrylic splint. (Fig. 3) Using computer assisted surgical simulation (CASS), a digital splint can be fabricated and 3D-printed using resin. (Fig. 4)
Fig. 3

Fig. 4

Model surgery can still be used today for single jaw cases with arguably similar occlusal results. However, CASS can help give additional information that helps practitioners at the time of surgery. For example, during an isolated bilateral sagittal split osteotomy (BSSO) advancement of the mandible, CASS can provide clinical measurements of the inferior alveolar nerve (IAN) to the buccal and inferior cortices, helping to avoid inadvertent damage and paresthesia. (Fig. 5) Visualizing interferences, alternating between segmental and single piece Lefort options to choose an ideal occlusion, and the visualization of dental roots and skeletal movements are some of the many other advantages of using CASS for single jaw cases.
Fig. 5

In double jaw surgery, both the maxilla AND mandible are moved through reference of the opposite jaw. Surgeries that encompassed both the maxilla and mandible were traditionally completed by transferring the malocclusion to a semi-adjustable articulator through facebow transfer and a centric relation bite. (Fig. 6) Traditional model surgery was labor intensive, prone to errors throughout the work up and there was a loss of perspective of the skeleton and face when limited to only the visualizing the dentition on a lab bench. Error can be introduced throughout the surgical work up through inaccurate impressions, models, facebow record, centric relation record altering the mounting, improper model surgery or within the splint fabrication stages. Even a minute error at each stage can compound and lead to a dramatically different surgical result. This is further exacerbated for more challenging cases such as facial asymmetry or those that require significant occlusal plane changes as traditional model surgery does not provide perspective of the dentofacial deformity.3 Fortunately, CASS has removed this labor intensive practice and transformed it into a brief online meeting between the surgeon and the planning engineer.
Fig. 6
Atypical Osteotomies
Segmental Lefort surgery, which involves the segmentation of the maxilla into two or more pieces to aid in transverse expansion and closure of open bites, has also greatly benefited from digital planning. The distance between roots can be visualized during the planning phase and in cases of severe proximity, cutting guides fabricated to aid in these segmental cuts. (Fig. 7) Once segmentation and mobilization is complete, 3D-printed palatal inserts can be fabricated and placed to maintain the transverse expansion of the maxilla, removing the need to wire in cumbersome final splints to the patient and decreasing overall operating time. (Fig. 8)
Fig. 7A

Fig. 7B
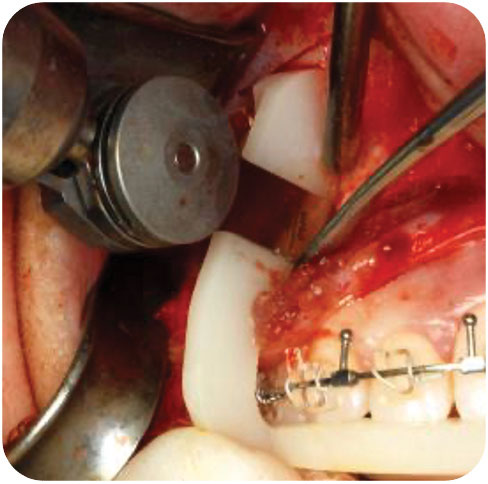
Fig. 8A
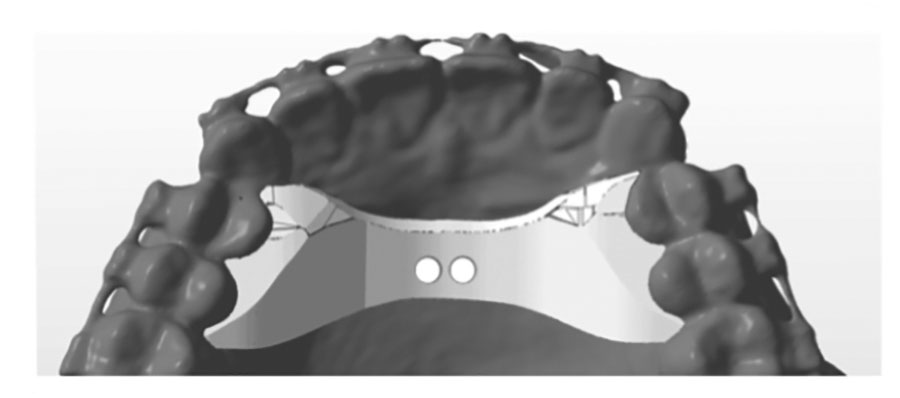
Fig. 8B

One of the major changes that CASS has led to is the visualization of atypical osteotomies and procedures that can aid in difficult cases. We are now able to simulate and design surgical options for patients that were previously difficult or impossible. Advances in guided surgery and custom fixation has re-opened the possibility of osteotomies such as the intra-oral inverted L osteotomy, C osteotomy, Z osteotomy, and total mandibular subapical osteotomy.6 These osteotomies are technique sensitive but can result in dramatic improvements in patient’s lives. (Fig. 9) Significant movements that previously required a separate donor site such as the iliac crest for autogenous bone grafting can often be harvested from the maxilla and mandible during routine osteotomies.7 (Fig. 10)
Fig. 9A

Fig. 9B

Fig. 9C

Fig. 9D

Fig. 9E

Fig. 9F
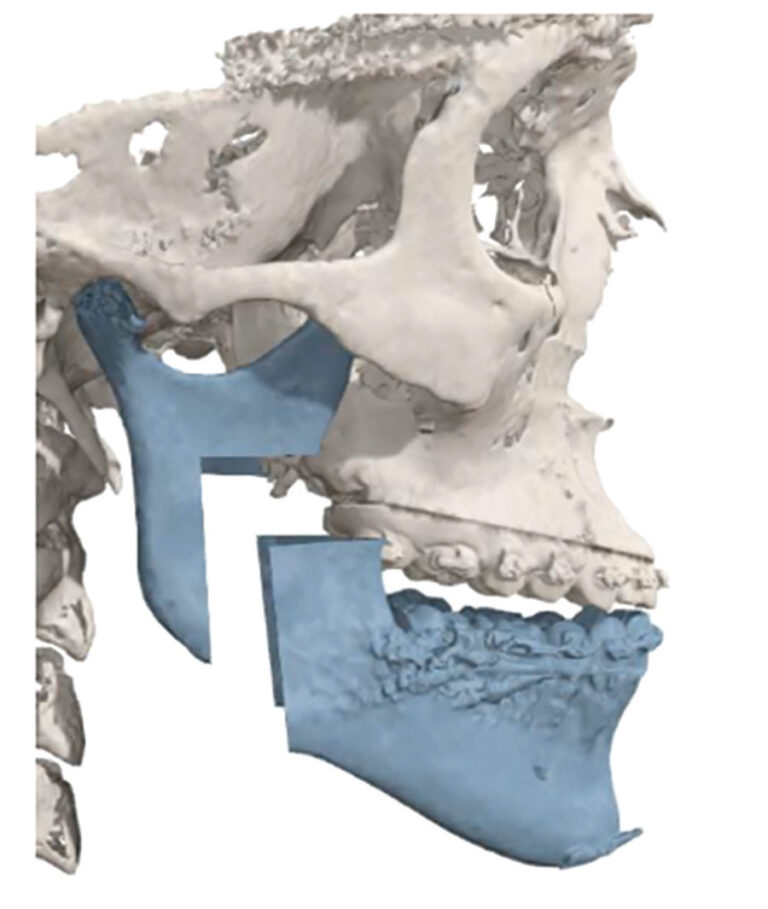
Fig. 9G
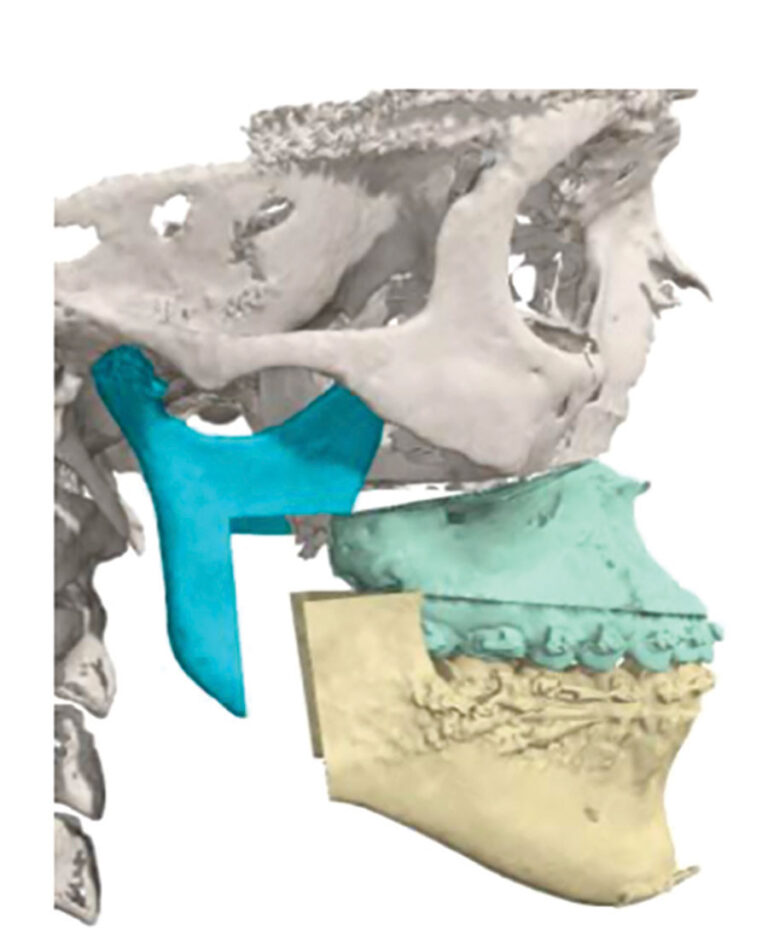
Fig. 10A
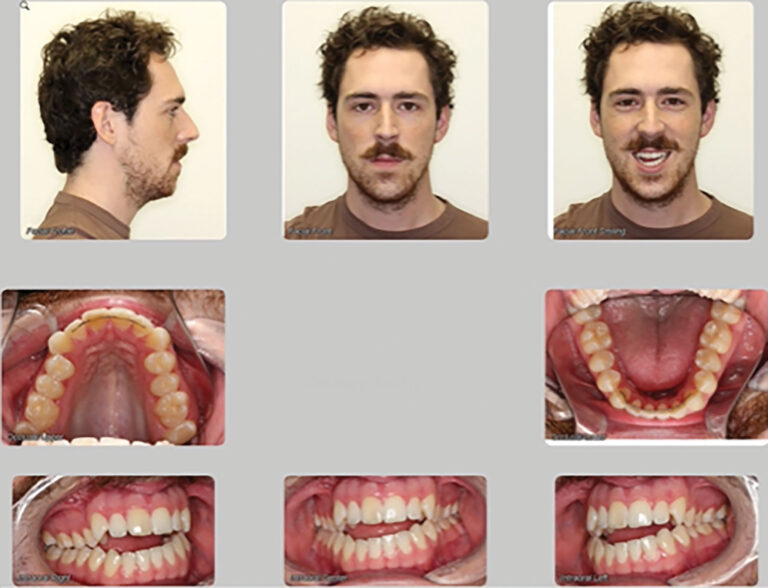
Fig. 10B

Fig. 10C

Although custom guides and fixation may sound appealing, it is important to remember that these add significant costs and should not be used for routine cases.
Conclusion
Modernizing digital workups and surgical planning has resulted in faster, more accurate surgery whilst still retaining the principles upon which the surgery was intended. In Canada, we are fortunate that the majority of costs are covered by public provincial health care plans, and patients are usually required to pay only for their orthodontic treatment and a small work-up fee associated with CASS. Portions of this work-up fee are often covered for patients who have private insurance, and this is something that can be discussed with the surgeon directly during the patient’s initial consultation visit.
Oral Health welcomes this original article.
References
- McCormick SU, Drew SJ: Virtual Model Surgery for Efficient Performance. J Oral Maxillofac Surg 69:638-644, 2011
- Hsu SS, Gateno J, Bell RB, Hirsch DL, Markiewicz MR, Teichgraeber JF, Zhou X, Xia JJ. Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: a prospective multicenter study. J Oral Maxillofac Surg 71(1):128-42, 2013
- Sharifi A, Jones R, Ayoub A, Moos K, Walker F, Khambay B, McHugh S. How accurate is model planning for orthognathic surgery? Int. J. Oral Maxillofac. Surg. 37: 1089–1093, 2008
- Dalstra M, Melsen B. From alginate impressions to digital virtual models: accuracy and reproducibility, Journal of Orthodontics, 36:1, 36-41, 2009.
- Li G. Patient radiation dose and protection from cone-beam computed tomography. Imaging Sci Dent. Jun;43(2):63-9, 2013
- Franco P, Farrell BB. Inverted L osteotomy: a new approach via intraoral access through the advances of virtual surgical planning and custom fixation. Oral and Maxillofacial Surgery Cases 2(1): 1-9, 2016
- Mascarenhas W, Dennis P, Rozanski J, Franco P, Farrell BB. Sites of autogenous bone harvesting during orthognathic surgery. Oral and Maxillofacial Surgery Cases 7(4), 2021
About the Author

Dr. Wendall Mascarenhas, is an Oral and Maxillofacial Surgeon who maintains a private practice in Brampton, ON. He is an Assistant Professor, University of Toronto, and an attending staff with the OMFS training program at Mt. Sinai Hospital. He is a supervisor of the Surgical Orthodontic clinic where he trains orthodontic and OMFS residents in orthognathic surgery.









