
Although CAD/CAM technology is not new to our profession, its widespread use is increasingly becoming the norm rather than the exception among dental professionals.
However, adopting a fully digital workflow in the dental practice can be quite challenging for those new to it. As with any learning experience, leaving behind the old ways and incorporating new ones requires effort and perseverance, not just on the part of the dentist but on the part of the entire dental team.
Once the new ways have been established and the learning curve has taken off, the benefits of having a digital dental practice can be fully enjoyed. Not only is patient experience improved, but the overall standard of care is elevated as the final outcome becomes more predictable and restorations are more precise.
This article will demonstrate how the digital workflow can be used to predictably restore a case where smile esthetics and function had been compromised due to wear and tooth loss.
CASE REPORT
A 45-year-old female patient presented to the author’s clinic with a chief complaint of small, discoloured teeth and an overall dislike of her smile esthetics. Although there were no significant findings in her medical history, she reported having a past habit of sucking lemon, which could partially explain the enamel wear observed in her upper arch during the clinical exam.
She also presented an end-to-end occlusion with worn incisal edges both in the upper and lower arches and mild lower anterior crowding (Fig. 1). She had good oral hygiene and sound periodontal tissues.
Fig. 1

Facially, she presented average lip length with an inadequate incisal display at rest. Her smile assessment revealed an average smile height, a flattened smile curve and deficient buccal corridors.
SMILE DESIGN AND TREATMENT PLANNING
Dental photography and the digital smile design associated to it are key tools in the treatment planning process of any aesthetic case.
A browser-based smile design software (Smilecloud Biometrics) was used to determine the patient’s ideal tooth size, shape and proportions (Fig. 2). Interestingly, this software uses artificial intelligence to couple the smile design with a search engine of natural tooth morphologies called a biometric library.
Fig. 2

This allows the dentist and the patient to visualize not one but several potential esthetic outcomes. The program also provides the user with stereolithography (STL) files of the chosen tooth forms which can be further used.
After the patient approved the smile design simulation, the STL files were imported into dental CAD software (Exocad), where they were merged with the patient’s intraoral scan (iTero, Align Technology) to create a 3D digital wax-up (Fig. 3).
Fig. 3
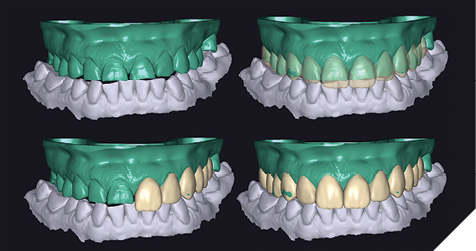
In a way somewhat similar to a conventional wax-up over a cast model, in the digital version, the tooth shapes are adapted to fit the patient’s natural teeth, gums and occlusion. In the case presented here, it was deemed necessary to open the vertical dimension to provide space for the reconstruction of the occlusal surfaces.
After completion of the digital wax-up, a 3D printer was then used to print the models using a Stereolithography (SLA) 3D printing machine (Formlabs, Form 2). These printed models are physical replicas of the initial smile design carried out in the smile design software, which can now be used to fabricate a conventional putty matrix. A polyvinyl siloxane (PVS) impression was taken of the 3D-printed model (Fig. 4).
Fig. 4

The mock-up (also known in the literature as an Aesthetic Pre-operative Temporary or APT) serves as a clinical simulation of the outcome, thus allowing the assessment of esthetics, function, and phonetics. It can be inserted into the patient’s mouth very easily using a self-curing resin (in this case, Luxatemp, DMG).
An additional benefit of the mock-up is that it can be used as a guide for minimal tooth preparations. With the mock-up still in place in the patient’s mouth, a depth cutter bur was used to provide enough space for future restorations while preserving the maximum amount of tooth structure.
PREPS, IMPRESSION AND CEMENTATION
Because of the need to increase the vertical dimension and restore both buccal and palatal surfaces, the decision was made to restore teeth 6, 7, 8, 9, 10 and 11 with full veneers, 3, 4, 5, 12, 13 with veneer-lays and 15 with an overlay. Tooth 14 was an implant-supported crown. In the lower arch, tooth 19 received an implant-supported crown, tooth 30 was restored with a crown, and the worn edges of the bottom anterior teeth were restored with direct composite (although the patient agreed to restore the lower with veneers in the future for maximum strength and aesthetics).
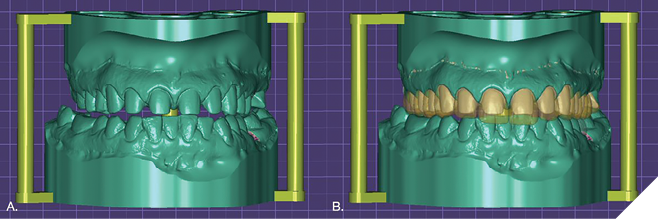
As previously described, minimal preps were achieved using the mock-up as a guide. The iTero Element 2 scanner took digital impressions of both the upper and lower arches. Subsequently, the STL files were imported into the Exocad software (Exocad) and merged with the previous digital wax-up (Fig. 5).
Fig. 5
All ceramic restorations were milled in Lithium disilicate using IPS e.max CAD blocks. The MT BL4 shade was employed (Fig. 6).
Fig. 6

All ceramic restorations were cemented following the manufacturer’s recommendations after confirming marginal fit and obtaining the patient’s approval during a trial insertion. This included conditioning the ceramic with 5% hydrofluoric acid for 20 seconds and applying a layer of silane to the etched surface (Monobond plus Ivoclar Vivadent) after rinsing and drying. The tooth substrates were treated with 35% phosphoric acid, rinsed for 20 seconds, and a layer of universal adhesive was applied to the dried surfaces (Scotchbond Universal, 3M). The full veneers, veneer-lays and only were adhesively luted using a light polymerizing resin luting agent (Relyx Veneer Cement, 3M ESPE) and photoactivated for 20 seconds with a high-power curing light device (Valo, Ultradent). The decision to use a photoactivated cement was made to ensure a light conversion and chromatic stability and is justified by the thickness (less than 1mm) and medium opacity of the restorations. The excess cement was removed, occlusal adjustments were made, and an acrylic removable appliance was made for the protection of the final restorations. The patient was satisfied with the result (Fig.s 7 & 8).
Fig. 7

Fig. 8

The digital workflow allows for high predictability of the esthetic outcome, as the final restorations can be made to match the digital wax-up with better precision than the analogue method (Fig.s 9 and 10). The learning curve involves all dental team members, including the dental lab, as good communication is still critical for treatment success.
 Fig. 9
Fig. 9

Fig. 10

Oral Health welcomes this original article.
About the Author:

Dr. Paola Ochoa graduated at the top of her class from Cayetano Heredia University in 2006. She has an Occlusion and Oral Rehabilitation degree from Universidad Científica del Sur and has received extensive training in Brazil and the United States. She is the co-founder of Infinity Dental Clinic and Infinity Advanced Dental Learning in Lima, Peru. Dr. Ochoa is a Member of the American Society for Dental Aesthetics and a Diplomate in the American Board of Aesthetic Dentistry. In her work, Dr. Ochoa employs an interdisciplinary, facially driven, and minimally invasive philosophy and utilizes digital tools for the planning and communication of all her cases.









